Clinical experience of Xiaochaihu decoction in the treatment of angina pectoris after PCI
Xue-xin Zhang, Yan-jiu Liu, Quan Li
Department of Cardiology, Qinhuangdao Hospital of Chinese Medicine Hospital, Qinhuangdao 066000,Hebei Province, China
Funding: Scientific Research Program of Hebei Provincial Administration of Traditional Chinese Medicine (No. 2015066)
Abstract Objective: To observe the clinical efficacy of Xiaochaihu decoction in the treatment of angina pectoris after PCI. Method: 122 patients with Angina pectoris after PCI were randomly divided into two groups. In the control group, 61 patients were treated with Antiplatelet, coronary dilation, lipid lowering and blood pressure lowering drugs according to the protocol of PCI. In the treatment group, 61 patients were given Xiaochaihu decoction (traditional Chinese medicine prescription granule of Sichuan New Green Pharmaceutical Science and Technology Development Co), 1 dose per day, twice. In the two groups, one course of treatment was 3 weeks. The changes of electrocardiogram and main disease were observed. Results: The treatment group significantly improved the clinical symptoms. At the same time, the number of angina attacks was reduced, and the electrocardiogram was improved. The effective rate was significantly better than that of the control group. It has statistical significance (P<0.05). Conclusion: Xiaochaihu decoction is effective and safe in the treatment of Angina Pectoris after PCI.
Key words: Traditional Chinese medicine; After PCI; Angina pectoris; Xiaochaihu decoction; Clinical observation
Introduction
After clinical coronary stenting (PCI), some patients still have recurrent angina pectoris[1], or even the occurrence of in-stent restenosis (ISR) gradually arouses clinical concern. Recurring postoperative chest pain, chest tightness, palpitations, fatigue, insomnia are accompanied by ischemic ST-T changes on the electrocardiogram seriously affect his quality of life. The pathogenesis of angina pectoris after PCI is different from other people’s angina pectoris[2]. Its mechanism is generally considered to be related to coronary artery inflammation, endothelial injury during surgery, high expression of miRNA (high-sensitivity C-reactive protein), and neuroendocrine factors[3]. Simple coronary expansion to improve myocardial blood supply is difficult to achieve satisfactory results. In recent years,Chinese medicine has achieved very high curative effects in the treatment of angina pectoris after PCI[4-5]. The author believes that the patient has angina pectoris again after PCI, although its pathogenesis is still consistent with the traditional Chinese medicine understanding of chest numbness, that is, it is summarized as the essence of the deficiency and the deficiency of yin, yang, qi, and blood.Stagnation, phlegm turbidity, and coldness are the targets,but they still have their own unique features. The first is the trauma factor of the operation itself, that is, the injury of the veins of traditional Chinese medicine is the basis,and the sudden pain is the sudden stagnation of the Qi and aggravates the blood stasis. Therefore, it is usually accompanied by clinical symptoms on the basis of angina:Symptoms caused by chest tightness, chest fullness, upset and palpitations, cold and heat in the chest, etc. Therefore,the treatment focuses on regulating the qi machine and dredging out the chest yang, and the circulation of qi is the circulation of blood, the veins of stroke can be unblocked, and the pain can be relieved. According to his clinical symptoms, he chose “Shanghan Lun” Xiaochaihu Decoction for treatment, and achieved satisfactory results.It is summarized as follows.
Materials and Methods
General information
We selected 122 patients with angina pectoris after PCI from July 2015 to February 2019 in the outpatient department of our hospital, and randomly divided them into treatment group and control group with 61 cases each. Treatment group: There were 41 males and 20 females, aged 42-78 years, with an average age of 61.7±8.3 years. There were 17 cases of diabetes and 45 cases of hypertension. The time after PCI was 5.3±1.75 months.Control group 61 cases: 38 males, 23 females, 46-75 years old, with an average age of 63.6±9.1 years, 21 cases with diabetes mellitus, 49 cases with hypertension, and the time after PCI was 4.6±1.1 months. The general data of the two groups were compared, and the difference was not statistically significant (P>0.05), and they were comparable.
Case enrollment criteria
More than 2 months after PCI, the onset of angina pectoris can be diagnosed, and the patient has repeated main symptoms:
chest pain, chest tightness, palpitations, upset; ECG may have dynamic ischemic ST-T changes, according to the “Cardiovascular Disease Treatment Guidelines and Recommendations”[6], it was in line with the diagnosis of angina pectoris.
TCM syndrome differentiation is a syndrome of Qi stagnation and blood stasis, and according to “Treatise on Febrile Diseases” Xiao Chai Hu Decoction, with Xiao Chai Hu Decoction:
chest fullness, chest tightness, chest pain, palpitations,upset, and other main symptoms.
Case exclusion criteria
New myocardial infarction occurs after operation:
my o cardial enzymes are elevated, and the electrocardiogram indicates myocardial infarction;
Acute phase with other diseases such as heart failure and lung infection.
Except for angina pectoris caused by heart diseases that are clearly diagnosed as other non-coronary heart diseases.
TCM dialectics are of other syndrome types, or the syndrome of Qi stagnation and blood stasis does not have the main symptom of Xiaochaihu Decoction
Treatment methods
Therapeutic medication
During the treatment period, both groups can continue to take basic disease treatment drugs and standard post-PCI medications: aspirin, clopidogrel double antibody,atorvastatin calcium, isosorbide mononitrate and other basic treatments.
In the control group, Bayer Aspirin (Bayer Healthcare Company, National Medicine Standard J20130078) was taken orally 100 mg 3 times a day; clopidogrel (Sanofi(Hangzhou) Pharmaceutical Co., Ltd., National Medicine Standard J20130083) 75 mg each time, daily 1 time;Isosorbide mononitrate (Livzon Pharmaceutical Factory of Livzon Group, National Medicine Standard H10930189) 10 mg each time, 3 times a day; Atorvastatin calcium (Pfizer Pharmaceutical Company, National Medicine Standard H20051407) 20 mg each time, 1 time per night.
The treatment group was given Xiaochaihu Decoction on the basis of the control group, referring to the drug composition ratio of the original prescription of “Treatise on Febrile Diseases” and the prescription drug composition of “Hu Xishu Medical Records Collection”[7]: Bupleurum 24 g, Scutellaria baicalensis 9 g, Pinellia Ternata 12 g,codonopsis 20 g, sweet 9 g, ginger 9 g, Cyperus rotundus 10 g, Aucklandia Lappa 10 g, and salvia 15 g. Sichuan New Green Pharmaceutical Technology Development Co., Ltd.produces the standard preparation of traditional Chinese medicine granules, one dose per day, twice in the morning after breakfast and in the afternoon before dinner.
Modification: Difficult or dry stools, red tongue, thick yellow coating, dry mouth and bitter mouth, choose raw Bupleurum, add Coptis 10 g, and raw Atractylodes 30 g;if loose stools, several times a day, pale tongue, fat side and tooth marks, Choose vinegar Bupleurum and stirfry Atractylodes macrocephala with bran 30 g; if the chest and flanks are full and heavy, go to the party to participate in the melon root 30 g; if the pain is severe, remove the skullcap and red peony 15 g; if you are upset, add 30 g raw keel and 30 g raw oysters. For those with hot flashes and night sweats, add silver Bupleurum 12 g, Schisandra 15 g,and Ephedra root 12 g. Take 1 dose a day, take 12 jujubes with boiled water except for nuclei after breakfast and lunch.
One course of treatment for the two groups was 3 weeks.During the treatment, when angina pectoris occurred,nitroglycerin or Suxiao Jiuxin Pills could be taken, and the number of times should be counted.
Outcome measures and evaluation criteria for curative effect
According to the 1979 National Research Conference on the Prevention and Treatment of Coronary Heart Disease Angina Pectoris and Arrhythmia with Integrated Traditional Chinese Medicine and Western Medicine[8]standards, observe the onset of angina pectoris before and after treatment; use times of nitroglycerin or Suxiao Jiuxin Pills per day; The degree of changes in the T wave and ST segment of the ECG and the number of leads.
Significant effect: The clinical symptoms disappeared or basically disappeared, or the number of angina pectoris episodes was reduced by more than 80%, basically no need to take nitroglycerin; the ECG returned to normal or roughly normal at rest.
Effective: The clinical symptoms are alleviated, the number of angina pectoris and the dosage of nitroglycerin are reduced by more than 50% and less than 80%; the ECG shows that the ST segment moves down, and the inverted T wave recovers more than 50% and less than 80%compared with before treatment.
Ineffective: No change in clinical symptoms, number of angina pectoris, and dosage of nitroglycerin, or although it has been reduced, the degree of improvement has not been achieved, and there is no change in electrocardiogram.Efficacy criteria for changes in main symptoms before and after treatment: Refer to the “Guiding Principles for Clinical Research of New Chinese Medicines” (Trial)[9]Quantification Table of Coronary Heart Disease and Angina Pectoris, and score changes in TCM symptoms according to no, mild, moderate, and severe degrees, such as chest pain: None, score 0; when the attack is relieved by rest, it does not affect daily life, and it is counted as 2 points; when the attack is relieved, drug treatment is required, and normal activities can be continued after remission. The score is 4 or 6; the attack is frequent and affects activities of daily living (such as Dressing, eating,walking, or large can induce symptoms) score 10 points,compare the score difference before and after treatment,and include the main symptoms of the score: chest pain,chest tightness, heart palpitations, upset, cold and heat exchanges.
In addition, the safety index was evaluated before and after the patient takes the medicine: liver function, blood lipids,blood rheology, etc., all examinations were performed with the chemiluminescence method, using the following reagents.
Statistical methods
Statistical analysis was performed using SPSS23.0 software,measurement data were expressed as mean ± standard deviation(±s),ttest wasusedforcomparison,count datawasexpressedaspercentage,andx2test was used for comparison.P<0.05 indicates that the difference is statistically significant.
Results
The results showed that the two groups were significantly different in the effective rate of relieving angina pectoris observed by the changes of ECG and the number of times of taking nitroglycerin (P<0.05). The results are shown in Table 1 and Table 2. After treatment, the main clinical symptoms of the two groups were significantly improved compared to before treatment, and there was a significant difference (P<0.05); there was a significant difference between the two groups after treatment (P<0.05). The treatment group was better than the control group. The results are shown in Table 3. It shows that the treatment group improved the overall condition of the patient while alleviating the symptoms of local angina pectoris.
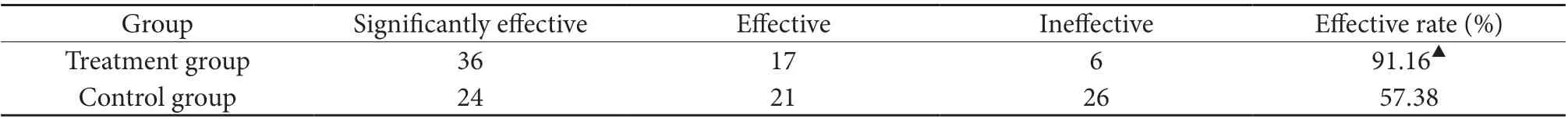
Table 1 Statistical table of ECG improvement after treatment (n=61)
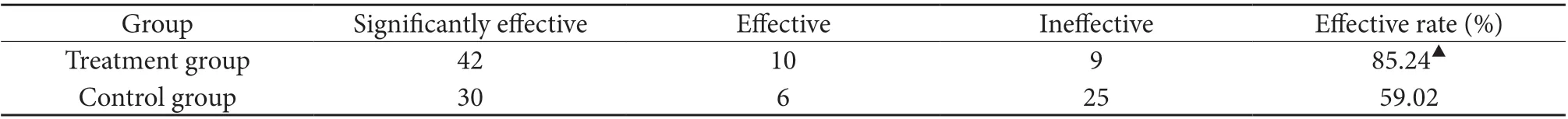
Table 2 Statistical table of nitroglycerin usage before after treatment (n=61)

Table 3 Statistic table of integrated scores of main symptoms before and after treatment (x±s) (n=61)
Other safety indexes: After treatment, triglyceride (TG),total cholesterol (CHO), and low-density lipoprotein cholesterol (LDL-C) were significantly improved between the two groups after treatment, and there was a significant difference (P<0.05); after treatment, the two groups had a significant improvement in TG, total cholesterol (CHO),and low-density lipoprotein cholesterol (LDL-C). There is a significant difference between CHO and LDL-C (P<0.05).The treatment group is better than the control group. The results are shown in Table 4, indicating that the treatment group has significantly improved blood lipids on the basis of relieving angina pectoris. The results are shown in Table 4. After treatment, plasma viscosity, whole blood lowshear viscosity, and whole blood high-shear viscosity were significantly improved in the two groups compared with before treatment, with significant differences (P<0.05);after treatment, plasma viscosity, whole blood low-shear viscosity, whole blood There was a significant difference in high shear viscosity (P<0.05). The treatment group was better than the control group. The results are shown in Table 5, indicating that the treatment group significantly improved blood viscosity on the basis of relieving angina pectoris. There was no statistical difference between the two groups of aspartate aminotransferase (ALT) and alanine aminotransferase (AST) before and after treatment(P>0.05). The results are shown in Table 6.
Table 4 Statistical table of changes in blood lipids before and after treatment (±s) (n=61)
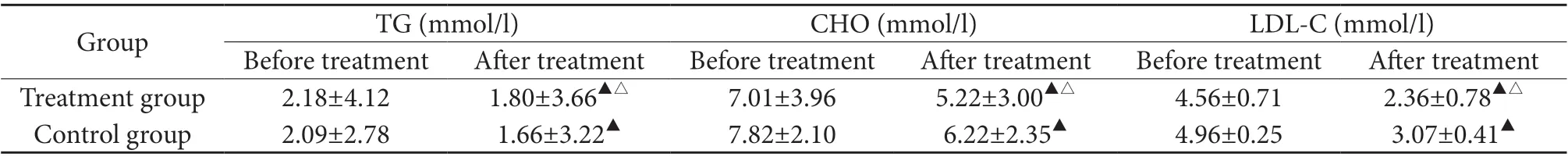
Table 4 Statistical table of changes in blood lipids before and after treatment (±s) (n=61)
Note: Compared with before treatment, ▲P<0.05, compared with control group, △P<0.05
Group TG (mmol/l) CHO (mmol/l) LDL-C (mmol/l)Before treatment After treatment Before treatment After treatment Before treatment After treatment Treatment group 2.18±4.12 1.80±3.66▲△ 7.01±3.96 5.22±3.00▲△ 4.56±0.71 2.36±0.78▲△Control group 2.09±2.78 1.66±3.22▲ 7.82±2.10 6.22±2.35▲ 4.96±0.25 3.07±0.41▲
Table 5 Statistical table of changes in blood rheology before and after treatment (±s) (n=61)

Table 5 Statistical table of changes in blood rheology before and after treatment (±s) (n=61)
Note: Compared with before treatment, ▲P<0.05, compared with control group, △P<0.05
Whole blood high shear viscosity(mpa • s)Before treatment After treatment Before treatment After treatment Before treatment After treatment Treatment group 2.58±0.22 1.48±0.26▲△ 22.01±1.86 14.98±1.18▲△ 7.77±0.62 7.77±0.62▲△Control group 2.06±0.24 1.90±0.22▲ 21.07±2.01 19.88±1.64▲ 7.75±0.56 6.22±0.49▲Group Plasma viscosity (mpa • s) Whole blood low shear viscosity(mpa • s)
Table 6 Statistical table of liver function changes before and after treatment (±s) (n=61)

Table 6 Statistical table of liver function changes before and after treatment (±s) (n=61)
Note: There is no statistical difference in liver function between the two groups before and after treatment, P>0.05
Group ALT (U/L) AST (U/L)Before treatment After treatment Before treatment After treatment Treatment group 40.220±4.16 42.09±3.07 75.51±7.16 75.02±5.44 Control group 41.66±2.98 40.13±4.12 77.82±8.11 75.22±6.30
Discussion
Coronary heart disease and angina pectoris belong to the“chest pain” and “true heart pain” diseases of traditional Chinese medicine. Although the disease position is in the “heart”, it is closely related to the whole body’s circulation of qi and blood, emotions, and other four internal organs[10]. Many clinical studies have explored the relationship between pathological changes in Western medicine and TCM syndromes. Although it has been proved that hemorheology, blood lipids, and serum interleukin-6 levels, homocysteine are related[11-13], but still it can not accurately guide TCM clinical diagnosis and treatment. Clinical dialectics should be based on the dialectical principles guided by the overall concept of Chinese medicine. In addition, angina pectoris is a clinical emergency, and relieving the onset of pain is the first priority of treatment. Although TCM believes that the pathological basis of coronary heart disease and angina pectoris, coronary atherosclerosis, or arterial plaque formation, is closely related to “phlegm” and “blood stasis”[14], it belongs to “chest pain” and “heart pain”, and restenosis after stent Qi stagnation during angina pectoris is still the most important pathological factor. In the Ming Dynasty “Xue’s Medical Records: Seeking Visceral Diseases”, it was said: “The circulation of liver qi will result in harmony of heart qi, and stagnation of liver qi will result in lack of heart qi.” Stagnation of phlegm and blood leads to impaired blood vessels, causing pain to occur,which promotes blood circulation and unblocked blood vessels. The power of qi still depends on the rising and falling of Qi[15]. In the clinical treatment of angina pectoris after PCI, in addition to paying attention to the basic pathogenesis of phlegm, stagnation, blood stasis, deficiency and deficiency, it is more important to emphasize the smoothness of the Qi machine[16]. This is also in accordance with the principle of treating the symptoms of emergency in Neijing, at this time, treating the symptoms of emergency, eliminating evil as the key,supplemented by tonic, and cast the product of Xuanbi,broad chest, activating blood and regulating qi[17].
Xiaochaihu Decoction is the main prescription of Shaoyang disease and the representative prescription of harmony method in “Treatise on Febrile Diseases”. It has been respected by many doctors since ancient times. In history, many physicians have modified Xiao Chai Hu Decoction, deriving many complicated prescriptions to treat diseases in various clinical departments. The clinical application of Xiaochaihu Decoction is based on the principle of Zhang Zhongjing’s prescriptions, and should grasp the key points of Shaoyang cardinal disadvantage and qi failure. “Symptoms and symptoms are treated, there is evidence and prescriptions are used”. The conditions for applying Xiaochaihu Decoction must be met during clinical trials, that is, to meet the four major requirements of “exchanging cold and heat”, “chest and frustration”,“not eating silently”, and “upset and vomit One of the symptoms or one or several of the contingencies, flexibly grasp the essence of the disease and use medicine. A good clinical grasp of the above principles can expand the scope of application of Xiaochaihu Decoction and improve the prevention and treatment of many refractory diseases such as angina after PCI. For example, Xu Zhongke’s note:Xiaochaihu can lead to clear qi into the Yang Dao, can lead the stomach qi to go up and make spring orders, and can disperse the menstrual blood to condense the qi.
The pathological mechanism of restenosis after PCI in Western medicine still has many mechanisms of action that we have not yet discovered. The mechanism for improving angina pectoris after PCI is comprehensive,and it is difficult to explain its therapeutic mechanism by a pathological mechanism. Research on the etiology and pathogenesis of Chinese medicine also needs to be further deepened. With the integration of Chinese and Western medicine, combined with the current research results, we should effectively combine their respective advantages, learn from each other’s strengths and make up for their weaknesses, and take a step forward in preventing restenosis and alleviating angina pectoris after PCI in the future.
 Global Traditional Chinese Medicine2021年1期
Global Traditional Chinese Medicine2021年1期
- Global Traditional Chinese Medicine的其它文章
- Exploration on YE Tianshi’s thinking of medication in the treatment of metrorrhagia and metrostaxis based on data mining
- A systematic review and meta-analysis of the efficacy and safety of Coix Seed Decoction in the treatment of rheumatoid arthritis
- Analysis of the medication for impotence based on data mining
- Etiology, pathogenesis and treatment of granulomatous mastitis
- Etiology analysis and treatment progress of diminished ovarian reserve function in traditional Chinese and Western medicine
- Traditional Chinese Medicine syndrome and treatment of brucellosis in chronic stage
