尿液中性粒细胞明胶酶相关脂质运载蛋白和白细胞介素-6水平对心脏外科术后患者严重液体超负荷的风险价值
胡星 蒋炘纹 蒋礼 雷迁


【摘要】目的 分析尿液中性粒細胞明胶酶相关脂质运载蛋白(NGAL)和白细胞介素-6(IL-6)水平对心脏外科术后患者严重液体超负荷(FO)的风险价值。方法 选取2020年4月—2023年3月在成都市第三人民医院接受心脏外科手术的患者220例,根据术后24 h FO,将FO≥10%的患者记为A组,将FO<10%的患者记为B组。分析两组一般资料,比较两组术前及术后尿液NGAL和IL-6水平,采用logistic回归模型分析心脏外科术后24 h内患者发生严重FO的危险因素,绘制ROC曲线,分析尿液NGAL、IL-6对患者发生严重FO的风险价值。亚组分析不同原发病对FO的影响。结果 A组男性ICU停留时间比例高于B组(P<0.05),术前白蛋白水平及术后当天尿量低于B组(P<0.05),两组体重指数、年龄、病程、手术时间、术中尿量、原发疾病类型、术前左室射血分数、肌酐水平、白细胞计数、血红蛋白水平、机械通气时间、体外循环时间,以及急性肾损伤、左心功能不全、高血压、心力衰竭、糖尿病占比比较无差异(P>0.05);两组术后2 h、术后12 h尿液NGAL和IL-6水平均高于术前(P<0.05),术后12 h尿液NGAL和IL-6水平均高于术后2 h(P<0.05),且A组术前、术后2 h及术后12 h均高于B组(P<0.05);logistic回归分析发现,术前尿液NGAL和IL-6水平高是心脏外科术后患者发生严重FO的危险因素(P<0.05);ROC结果显示,术前尿液NGAL和IL-6水平对心脏外科术后患者发生严重FO的最佳截断点分别为48.04 ng/mL和32.26 pg/mL,AUC分别为0.865和0.704,二者联合检测AUC为0.894。冠心病、先天性心脏病、心脏瓣膜病亚组之间FO情况、ICU停留时间、体外循环时间、术后当天尿量及术前NGAL和IL-6之间无显著差异(P均>0.05)。结论 心脏外科术后患者尿液NGAL和IL-6水平异常升高,术前尿液NGAL和IL-6水平是其发生严重FO的危险因素。
【关键词】心脏外科手术;液体超负荷;中性粒细胞明胶酶相关脂质运载蛋白;白细胞介素-6
【DOI】10.16806/j.cnki.issn.1004-3934.2024.03.020
Risk Value of Urinary Neutrophil Gelatinase-Associated Lipocalin and Interleukin-6 Levels on Severe Fluid Overload in Patients After Cardiac Surgery
HU Xing1,JIANG Xinwen2,JIANG Li1,LEI Qian2
(1.Department of Cardiac Surgery ICU,The Third Peoples Hospital of Chengdu,Chengdu 610034,Sichuan,China;2.Department of Anesthesiology,Sichuan Provincial Peoples Hospital,Sichuan Academy of Medical Sciences,Chengdu 610072,Sichuan,China)
【Abstract】Objective To analyze the risk value of urinary neutrophil gelatinase-associated lipocalin (NGAL) and interleukin-6 (IL-6) levels on severe fluid overload (FO) in patients after cardiac surgery.Methods A total of 220 patients underwent cardiac surgery in The Third Peoples Hospital of Chengdu from April 2020 to March 2023 were enrolled.Patients with FO≥10% were classified into group A and FO<10% into group B according to FO within 24 h after surgery.General data were analyzed and urinary NGAL and IL-6 levels were compared before and after surgery.Logistic regression model was used to analyze risk factors for severe FO after surgery.ROC curve was plotted to analyze the risk value of urinary NGAL and IL-6 on severe FO.The influence of different primary diseases on FO was analyzed by subgroups.Results The proportion of male patients and stay time in ICU were higher in group A than group B (P<0.05),while the preoperative albumin level and urine volume the day after surgery were lower (P<0.05).There was no significant difference in body mass index,age,course of disease,operation time,urine volume during operation,primary disease types,preoperative left ventricular ejection fraction,creatinine,leukocytes,hemoglobin,mechanical ventilation time,extracorporeal circulation time,intraoperative urine volume,the proportion of acute kidney injury,left cardiac insufficiency,hypertension,heart failure and diabetes between the two groups (P>0.05).Urinary NGAL and IL-6 levels of two groups were increased (P<0.05) at 2 h and 12 h after surgery,not only the higher at 12 h than 2 h (P<0.05),but also the higher in group A than group B before surgery,after surgery and 12 h after surgery (P<0.05).Logistic results showed high urinary NGAL and IL-6 levels before operation were risk factors for severe FO in patients after cardiac surgery (P<0.05).ROC results showed the optimal cut-off point of preoperative NGAL and IL-6 levels on severe FO after surgery was 48.04 ng/mL and 32.26 pg/mL,with the AUC of 0.865,0.704 respectively and 0.894 for their combined detection.There was no difference in FO,ICU stay time,cardiopulmonary bypass time,urine volume the day after operation and preoperative NGAL and IL-6 among the subgroups of coronary,congenital and valvular heart diseases (all P>0.05).Conclusion Urinary NGAL and IL-6 were abnormally elevated in patients after cardiac surgery,the levels of which before surgery could be risk factors for severe FO.
【Keywords】Cardiac surgery;Fluid overload;Neutrophil gelatinase-associated lipocalin;Interleukin-6
液体超负荷(fluid overload,FO)是腹腔间隙综合征的原因之一,临床将液体蓄积大于或等于基线体重10%定义为FO[1]。FO是心脏病外科手术后常见且严重的并发症之一,严重影响患者的康复及预后结局[2]。液体管理是心脏病外科手术后的重要组成部分,早期积极的液体复苏能增加心脏前负荷以及心输出量,促进氧气输送,提升组织器官的氧状态,改善患者预后,但由于无法统一液体复苏目标,多数心脏外科术后患者在经过液体复苏后血流动力学改善不明显,且部分患者出现不同程度FO[3-4]。液体过多对肾脏不利,会造成肾间质水肿、肾盂压力升高,静脉及肾小管压力升高,导致肾血流减少、肾小球滤过率下降、肾小管渗漏增加,进而造成胸腔内压剧增、组织器官水肿、血管扩张,对患者术后治疗及康复造成不良影响[5]。有研究[6]显示,肾替代治疗的危重症患儿FO>10%与死亡在内的不良结局有关。有研究[7]显示,FO≥10%可增加急性肺损伤患者不良事件的发生风险。因此,临床上对行重症外科手术患者进行FO风险评估对患者的预后结局具有重要意义。鉴于此,现探讨尿液中性粒细胞明胶酶相关脂质运载蛋白(neutrophil gelatinase-associated lipocalin,NGAL)和白细胞介素(interleukin,IL)-6水平评估心脏外科术后患者严重FO的风险价值,对临床诊断FO具有重要意义。
1 资料与方法
1.1 一般资料
经医院伦理委员会审核批准(FA-2020220A),选取2020年4月—2023年3月在成都市第三人民医院接受心脏外科手术的患者220例,根据术后24 h FO,将FO≥10%的患者记为A组,将FO<10%的患者记为B组。纳入标准:年龄>18岁;均接受体外循环下心脏病开胸根治术治疗;患者及家属签署知情同意书。排除标准:心功能>Ⅳ级者;近期服用过肾损伤药物或糖皮质激素类药物;心脏移植者;合并自身免疫性疾病者;近期或术后伴有尿路感染者;术前存在肾功能损伤或急慢性肾脏病者;术前存在气道或肺部疾病气管插管者;合并恶性肿瘤者;妊娠及哺乳期者。
1.2 方法
患者均经心脏中心熟练手术医师,遵循相同手术标准,在体外循环下实施根治手术,根据患者情况改良超滤,最大限度减轻水肿。均于术后进行标准的液体治疗,动态检测中心静脉压,结合病情判断容量,保证循环稳定、心率正常的前提下做利尿处理使FO降至最低。根据术后24 h FO值以FO=10%为截断点进行分组。FO值计算方法为:FO=[输入液体量(L)-排出液体量(L)]/手术前体重(kg)×100%。
1.3 观察指标
比较两组一般资料,包括性别、年龄、病程、体重指数、术前白蛋白水平、术后当天尿量、术前左室射血分数(left ventricular ejection fraction,LVEF)、肌酐水平、白细胞计数、血红蛋白水平、机械通气时间、手术时间、体外循环时间、术中尿量、急性肾损伤(acute kidney injury,AKI)、左心功能不全、高血压、心力衰竭、糖尿病;比较两组术前及术后尿液NGAL和IL-6水平,分别于术前及术后2 h收集患者尿液,采用酶联免疫吸附法检测尿液NGAL和IL-6水平,操作步骤严格按照说明书进行;分析心脏外科术后24 h内患者发生严重FO的危险因素;分析尿液NGAL和IL-6对患者发生严重FO的风险价值;亚组分析不同原发疾病类型对FO的影响。
1.4 统计学方法
采用SPSS 26.0处理分析数据,以±s表示计量资料,以t检验分析两样本数据;计数资料以n(%)表示,采用χ2检验,P<0.05为差异有统计学意义;以logistic回归分析法分析导致心脏外科术后24 h内患者发生严重FO的OR及95%CI;通过建立ROC曲线分析尿液NGAL和IL-6对患者发生严重FO的风险价值。
2 结果
2.1 比较两组一般资料
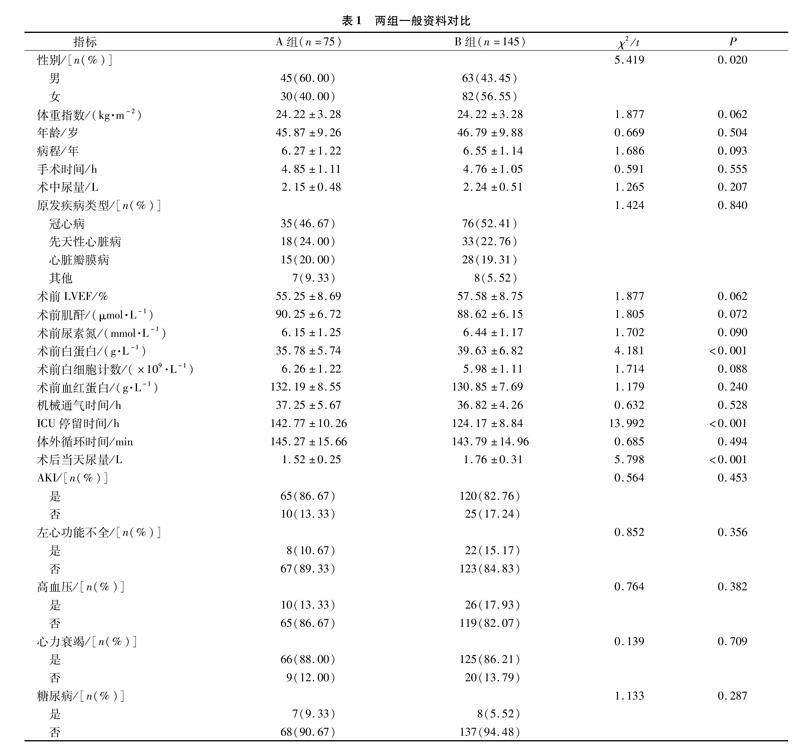
A组男性比例、ICU停留时间均高于B组(P<0.05),术前白蛋白水平及术后当天尿量低于B組(P<0.05),两组体重指数、年龄、病程、手术时间、术中尿量、原发疾病类型、术前LVEF、肌酐、白细胞计数、血红蛋白水平、机械通气时间、体外循环时间以及AKI、左心功能不全、高血压、心力衰竭、糖尿病占比比较无差异(P>0.05),见表1。
2.2 比较两组术前及术后尿液NGAL和IL-6水平
两组术后2 h、术后12 h尿液NGAL和IL-6水平均高于术前(P<0.05),术后12 h尿液NGAL和IL-6水平均高于术后2 h(P<0.05),且A组术前、术后2 h及术后12 h均高于B组(P<0.05),见表2。
2.3 心脏外科术后患者严重FO的多因素分析
以心脏外科术后患者是否发生严重FO为因变量,以性别、原发疾病类型、术前LVEF、体外循环时间、术前白蛋白水平、ICU停留时间、术后当天尿量以及术后2 h尿液NGAL和IL-6水平为自变量赋值;logistic回归分析发现,术前尿液NGAL和IL-6水平高是心脏外科术后患者发生严重FO的危险因素(P<0.05),见表3。
2.4 术前尿液NGAL和IL-6水平对心脏外科术后患者发生严重FO的预测价值
ROC曲线分析结果显示,术前尿液NGAL和IL-6水平对心脏外科术后患者发生严重FO的最佳截断点分别为48.04 ng/mL和32.26 pg/mL,AUC分别为0.865和0.704,二者联合检测AUC为0.894,见表4,图1。
2.5 亚组分析结果
冠心病、先天性心脏病、心脏瓣膜病亚组之间FO情况、ICU停留时间、体外循环时间、术后当天尿量及术前NGAL和IL-6之间无显著差异(P均>0.05),见表5~7。
3 讨论
FO在心脏外科术后患者中具有较高的发病率及死亡率[8],早期发现并及时治疗FO可逆转,多数患者肾功能及组织损伤都可恢复,因此早期预测FO风险对临床意义重大[9]。本研究以心脏外科术后患者FO=10%为截断点,探讨尿液NGAL和IL-6水平对心脏外科术后患者发生FO的预测价值。
心脏外科术后患者出现FO是临床常见问题,会对肾功能造成明显影响,而心脏外科术后患者FO与炎症因子、肾功能损伤有关。NGAL是在激活的中性粒细胞中发现的小分子量蛋白,可直接反映早期肾功能损伤情况,在肾脏组织正常形态下水平极低,但心脏外科术后FO患者肾小管上皮细胞受损导致肾功能损伤,激活中性粒细胞,分泌大量NGAL,造成尿液NGAL水平异常升高[10-11]。IL-6是趋化因子,也是临床常用的感染性检测指标,在机体发生炎症反应或组织受伤时水平升高[12]。心脏外科术后FO患者出现明显的临床炎症反应,使机体处于微炎症反应状态,体内多种物质对机体免疫系统反应刺激促进IL-6的分泌,导致IL-6水平显著升高[13]。本研究对比分析发现,心脏外科术后患者尿液NGAL和IL-6水平持续升高,且A组水平更高,说明心脏外科术后出现FO的患者存在肾损伤、炎症状态。此外,术后发生严重FO患者在ICU停留时间明显延长,说明FO会加重患者病情,从而延长患者停留ICU时间。
本研究进一步分析发现,术后当天尿量少、术前尿液NGAL和IL-6水平高是心脏外科术后患者发生严重FO的危险因素。有研究[14]显示,FO是老年ICU患者发生AKI的独立危险因素,造成静脉压升高,加重心力衰竭,继发腹腔间隙综合征,影响肾脏灌注。肾功能受损会引起肾血流量减少、肾小球滤过率下降,导致患者尿量减少。术后发生严重FO可造成肾功能损伤,促进NGAL分泌,肾功能受损时肾小球滤过率下降,NGAL经过肾小管重吸收受阻,而肾小管上皮细胞受损可造成NGAL从肾小管溢出到尿液中,因此患者发生严重FO后尿液NGAL水平升高[15]。术后FO患者更易發生炎症反应,促进IL-6等炎性因子的分泌,引起肺水肿或外周组织水肿,加重机体感染,进一步促进炎症反应,而肾间质水肿可损害肾功能,导致肾血流量及肾小球滤过率降低,IL-6经过肾小管重吸收时大量溢出至尿液中,导致尿液IL-6水平升高[16]。
ROC曲线分析结果显示,术前尿液NGAL和IL-6水平对心脏外科术后患者发生严重FO的AUC分别为0.865和0.704,准确度分别为77.27%和69.09%,二者联合检测AUC为0.894,准确度为80.91%,因此术前尿液NGAL和IL-6联合检测能提高严重FO的检出率。Thompson等[17]研究显示,术后早期的尿液NGAL与术后48 h内FO相关。Elitok等[18]研究表明ICU患者入院时的尿液NGAL和IL-6水平可能有助于预测心脏手术后的严重FO。因此,临床可在术前动态检测心脏外科手术患者尿液NGAL和IL-6水平,根据实测值评估患者术后发生FO的风险,以利于在术后对患者及时进行有效的针对性措施,尽早改善肾脏灌注、减少肾损伤及耗氧量,改善患者预后。此外,本研究还进一步亚组分析冠心病、先天性心脏病、心脏瓣膜病等不同原发病对FO的影响,结果显示各亚组临床指标无明显差异,可能与纳入样本量的范围有关。
综上所述,术前尿液NGAL和IL-6检测均可预测早期FO的发生,联合检测效能更高,可大幅提高心脏外科术后患者严重FO的检出率。
参考文献
[1]Casas-Aparicio GA,León-Rodríguez I,Hernández-Zenteno RJ,et al.Aggressive fluid accumulation is associated with acute kidney injury and mortality in a cohort of patients with severe pneumonia caused by influenza A H1N1 virus[J].PLoS One,2018,13(2):e0192592.
[2]Lopez T,Banerjee D.Management of fluid overload in hemodialysis patients[J].Kidney Int,2021,100(6):1170-1173.
[3]Patil VP,Salunke BG.Fluid overload and acute kidney injury[J].Indian J Crit Care Med,2020,24(suppl 3):S94-S97.
[4]Castauela-Sánchez V,Hernández-Suárez A,García-Benítez L,et al.Fluid overload as a predictor of morbidity and mortality in pediatric patients following congenital heart surgery[J].Bol Med Hosp Infant Mex,2022,79(3):187-192.
[5]Fu MR,Li Y,Conway C,et al.The effects of exercise-based interventions on fluid overload symptoms in patients with heart failure:a systematic review and meta-analysis[J].Biomedicines,2022,10(5):1111.
[6]Luppes VAC,Willems A,Hazekamp MG,et al.Fluid overload in pediatric univentricular patients undergoing Fontan completion[J].J Cardiovasc Dev Dis,2023,10(4):156.
[7]Woodward CW,Lambert J,Ortiz-Soriano V,et al.Fluid overload associates with major adverse kidney events in critically ill patients with acute kidney injury requiring continuous renal replacement therapy[J].Crit Care Med,2019,47(9):e753-e760.
[8]Arslan AH,Aksoy T,Ugur M,et al.Factors affecting the clinical outcomes in pediatric post-cardiotomy patients requiring perioperative peritoneal dialysis[J].Rev Assoc Med Bras(1992),2022,68(5):627-631.
[9]Carlisle MA,Soranno DE,Basu RK,et al.Acute kidney injury and fluid overload in pediatric cardiac surgery [J].Curr Treat Options Pediatr,2019,5(4):326-342.
[10]Loomba RS,Villarreal EG,Dhargalkar J,et al.The effect of dexmedetomidine on renal function after surgery:a systematic review and meta-analysis[J].J Clin Pharm Ther,2022,47(3):287-297.
[11]Kot K,Kupnicka P,Witulska O,et al.Potential biomarkers in diagnosis of renal acanthamoebiasis[J].Int J Mol Sci,2021,22(12):6583.
[12]Xie M,Chen YT,Zhang H,et al.Diagnostic value of procalcitonin and interleukin-6 on early postoperative pneumonia after adult cardiac surgery:a prospective observational study[J].Heart Surg Forum,2022,25(1):E020-E029.
[13]Puchinger J,Ryz S,Nixdorf L,et al.Characteristics of interleukin-6 signaling in elective cardiac surgery—A prospective cohort study[J].J Clin Med,2022,11(3):590.
[14]Ethgen O,Murugan R,Echeverri J,et al.Economic analysis of renal replacement therapy modality in acute kidney injury patients with fluid overload[J].Crit Care Explor,2023,5(6):e0921.
[15]Santos MG,Pontes JPJ,Gonalves Filho S,et al.Impact of colloids or crystalloids in renal function assessed by NGAL and KIM-1 after hysterectomy:randomized controlled trial[J].Braz J Anesthesiol,2022,72(6):720-728.
[16]林博,韓冉,寿好长,等.尿IL-6与血IL-6、SOD、C1q联合检测在2型糖尿病肾病诊断中的应用价值[J].标记免疫分析与临床,2021,28(8):1261-1265,1304.
[17]Thompson EJ,Chamberlain RC,Hill KD,et al.Association of urine biomarkers with acute kidney injury and fluid overload in infants after cardiac surgery:a single center ancillary cohort of the steroids to reduce systemic inflammation after infant heart surgery trial[J].Crit Care Explor,2023,5(5):e0910.
[18]Elitok S,Isermann B,Westphal S,et al.Urinary biomarkers to predict severe fluid overload after cardiac surgery:a pilot study[J].Biomark Med,2021,15(16):1451-1464.
收稿日期:2023-06-29
基金项目:2019年四川省卫生健康委员会科研课题(普及应用项目)立项课题(19PJ126)
通信作者:胡星,E-mail:mei90512@163.com

