Drug Utilization Review of Itraconazole Injection for Treating Deep Fungal Infection in a Hospital
DONG Wei-hua, HUANG Tai-kang, DONG Ya-lin
(1. Research Center of Modern Social Pharmacy, Shenyang Pharmaceutical University, Shenyang 110016, China; 2. The First Affiliated Hospital, Medical School of Xi’an Jiaotong University, Xi’an 710061, China; 3. China Food and Drug Administration, Beijing 100810, China)
Drug Utilization Review of Itraconazole Injection for Treating Deep Fungal Infection in a Hospital
DONG Wei-hua1,2, HUANG Tai-kang1,3, DONG Ya-lin2
(1. Research Center of Modern Social Pharmacy, Shenyang Pharmaceutical University, Shenyang 110016, China; 2. The First Affiliated Hospital, Medical School of Xi’an Jiaotong University, Xi’an 710061, China; 3. China Food and Drug Administration, Beijing 100810, China)
Objective To investigate the utilization of itraconazole injection for treating deep fungal infection in a hospital. Methods The utilization of itraconazole injection in a hospital from 2008 to 2012 was investigated retrospectively and analyzed statistically. Results and Conclusion There are 152 cases with itraconazole injection. 90.8% received short-term medication of less than 14 days, 75.7% received irrational loading dose, 6.6% changed antifungal drugs frequently, and 24.3% used drugs potentially interacting with itraconazole, but the doses of itraconazole and combined drugs are not adjusted. Rational use of itraconazole injection should be improved.
itraconazole injection; deep fungal infection; drug utilization review
Deep fungal infection is an infectious disease that caused by fungi on the dermis, mucosa and organs. In recent years, the incidence rate of deep fungal infection increased significantly. It has become an important factor which threatens the patients’ lives. Many factors lead to the incidence of fungal infection. The factors include chemotherapy, the use of many kinds of canal, hematopoietic stem cell transplantation, the occurrence of graft versus host disease, utilization of broad-spectrum antibiotic etc. Itraconazole, a new generation of triazole broad spectrum antifungal, works better than fluconazole against aspergillus, sporothrix dermatitis, blastomycosis, histoplasmosis. Itraconazole has become the first choice drug for non-fatal histoplasmosis and blastomycosis[1]. Although it has the advantage of efficacy and safety, itraconazole is expensive. It may lead to the increase of hospitalization spending if itraconazole is abused. Therefore, it is necessary for us to investigate its situation and guide the clinical rational use. In this study, the utilization of itraconazole injection in a tertiary hospital in the past five years was investigated retrospectively and analyzed statistically to evaluate the rationality of the drug use.
1 Material and methods
A retrospective survey of the utilization of itraconazole injection in a hospital from 2008 to 2012 was carried out. The data covered the following aspects: ①the patients’ name, age, and gender; ②admission departments, discharge diagnosis; ③the course of treatments, names of disease, dosage and administration, sequential therapy and combined drugs of itraconazole injection; ④Fungal culture results, Fungal infection diagnosis; ⑤liver and kidney function, adverse reactions. 159 cases of hospitalized patients who used itraconazole injection and 152 copies of medical records were obtained ultimately. 97 patients were males, and 55 were females. The age ranged from 7 to 85 years old, and the average age was (58.10 ± 15.6).
2 Findings
2.1 The division of the cases
Patients who used itraconazole injection were distributed among 15 departments in this hospital. Patients in hematology department ranked the first and the percentage was up to a total of 55.9%,the other departments such as respiratory department, geriatrics department, oncology department, renal transplant department, and center ICUfollowed respectively. The details are shown in Table 1.
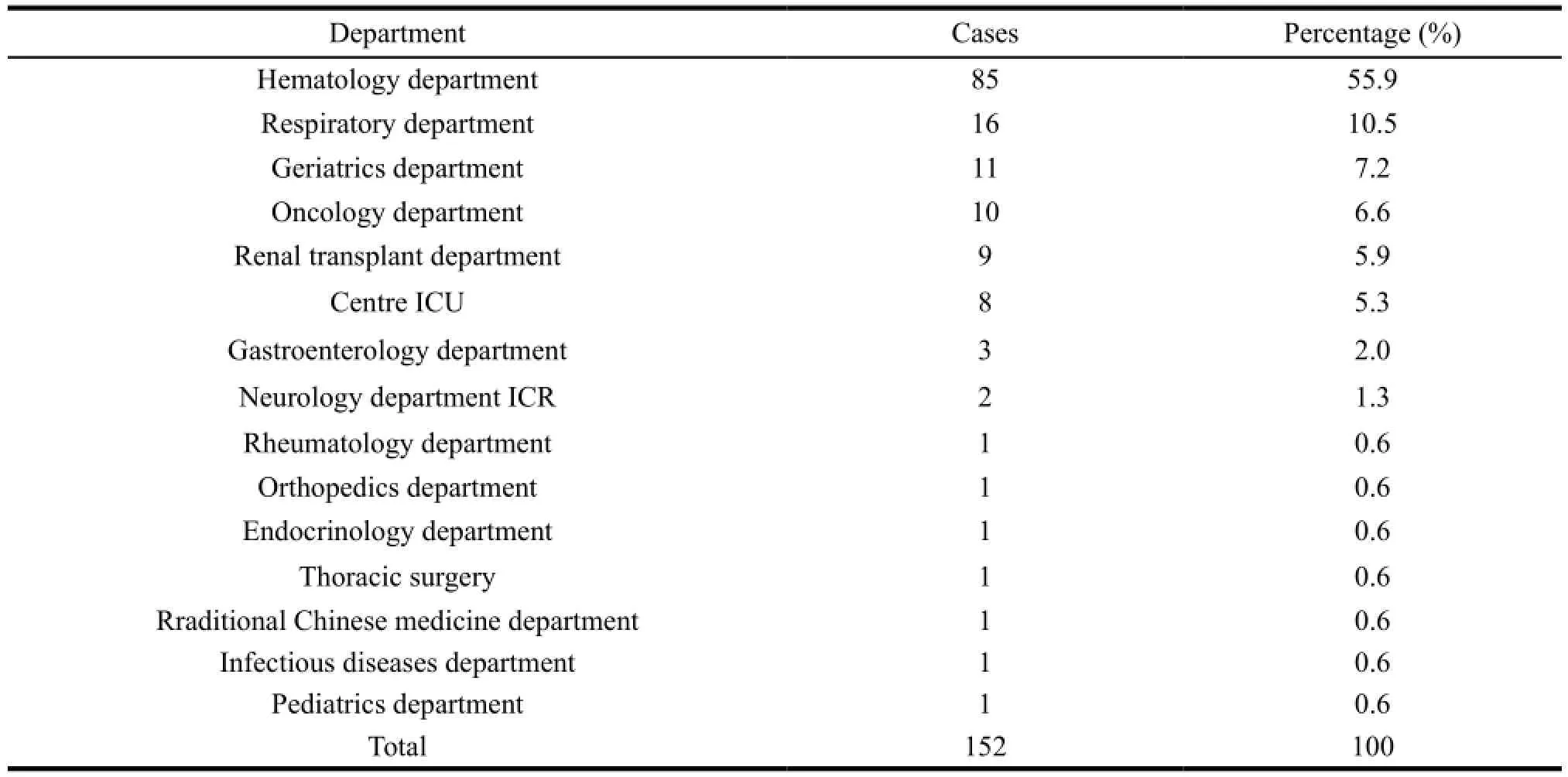
Table 1 The division of the cases using itraconazole injection
2.2 Underlying disease situation
Among the 152 patients, 109 cases suffered from three or more kinds of diseases and the percentage was 72%. The rest suffered from two kinds of diseases. And 95 cases suffered from respiratory diseases (such as pneumonia, respiratory tract infections, bronchitis, chronic obstructive pulmonary disease, emphysema, et al), 84 cases with hematologic malignancies (such as Leukemia, lymphoma, myeloma, myeloproliferative syndrome, aplastic anemia, et al), 33 cases with cardiovascular disease (such as hypertension, coronary heart disease, arrhythmia, et al), 22 cases with diabetes, 19 cases with malignancy, 15 cases with chronic renal insufficiency, 10 cases with organ transplant (kidney and liver transplant), and 7 cases with stroke.
149 patients (98.0%) received broad-spectrum antibiotics treatment, 126 (82.9%) got glucocorticoid treatment, 102 (67.1%) with chemotherapy. And 95 (62.5%) with hypoproteinemia and 13 (8.6%) received immunosuppressive therapy.
2.3 The details of Fungi culture before and after using itraconazole injection
A total of 119 patients carried out fungal finding and fungal culture, and 8 patients carried out G test and GM test. 87 patients (57.2%) carried out fungal finding and 79 (52.0%) carried out fungal culture. 31 patients carried out fungal culture before using itraconazole injection, and the positive rate was 74.2%. After using itraconazole injection, 58 patients carried out fungal culture and the positive rate was 10.3%. In the positive culture results, candida infections account for the majority. The details are shown in Table 2.
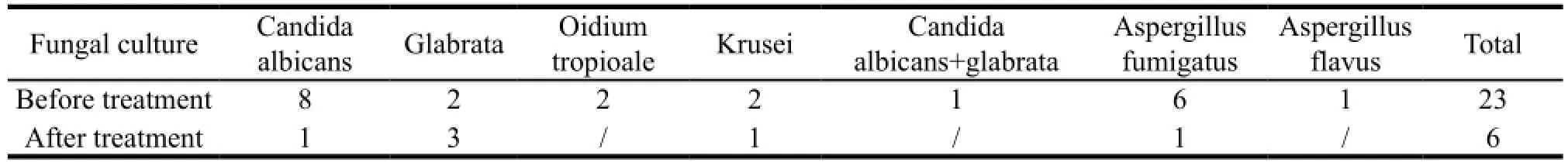
Table 2 The results of fungi culture before and after using antifungal drugs
2.4 The usage of itraconazole injection
The usage of itraconazole injection were analyzed and evaluated, including the routes of administration, course of treatment, loading dose and sequential therapy of itraconazole injection in these patients. The details are shown in Table 3.
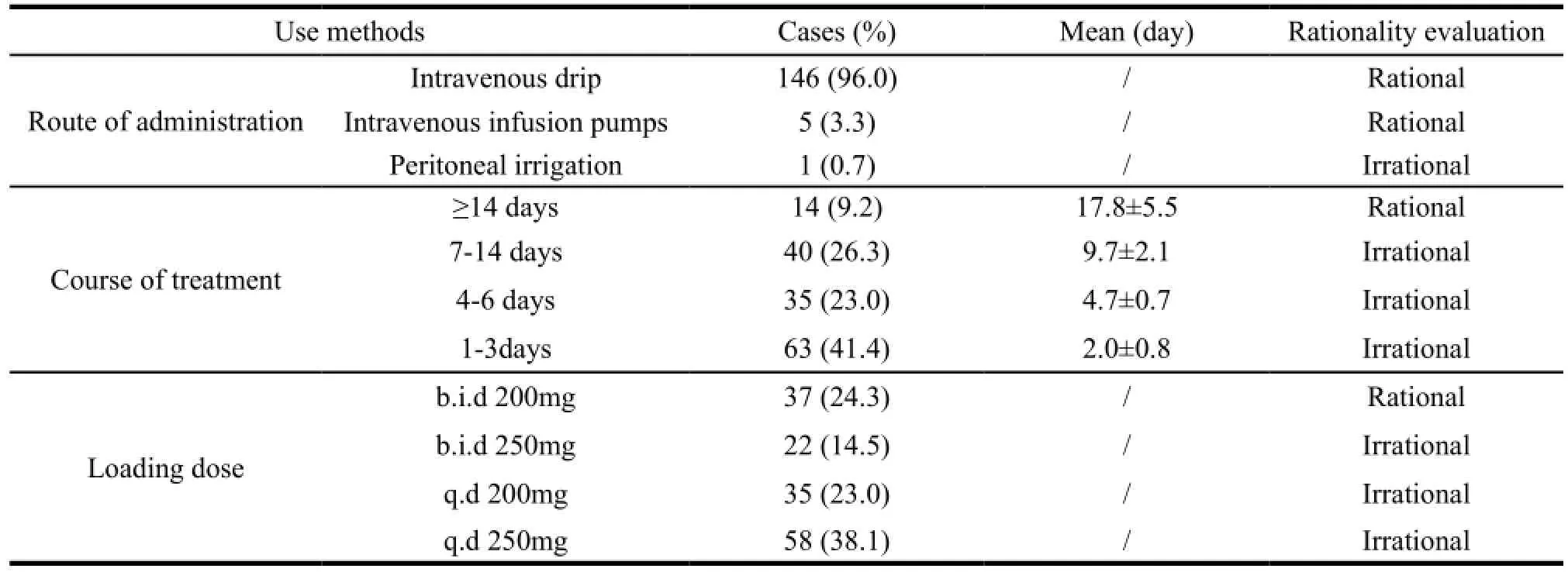
Table 3 Rational evaluation of the use of itraconazole(n=152)
2.5 The details of other combined antifungal
36 patients (23.7%) used itraconazole injection only, 72 patients (47.4%) used 2 kinds of antifungal, 35 patients (23.0%) used 3 kinds of antifungal, and 9 patients (5.9%) used 4 kinds of or more antifungal. These combined antifungal were: itraconazole capsules and oral solution, fluconazole capsule and injection, voriconazole tablets and injection, caspofungin injection, micafungin injection, amphotericin B injection and liposomal amphotericin B. The details are shown in Table 4.
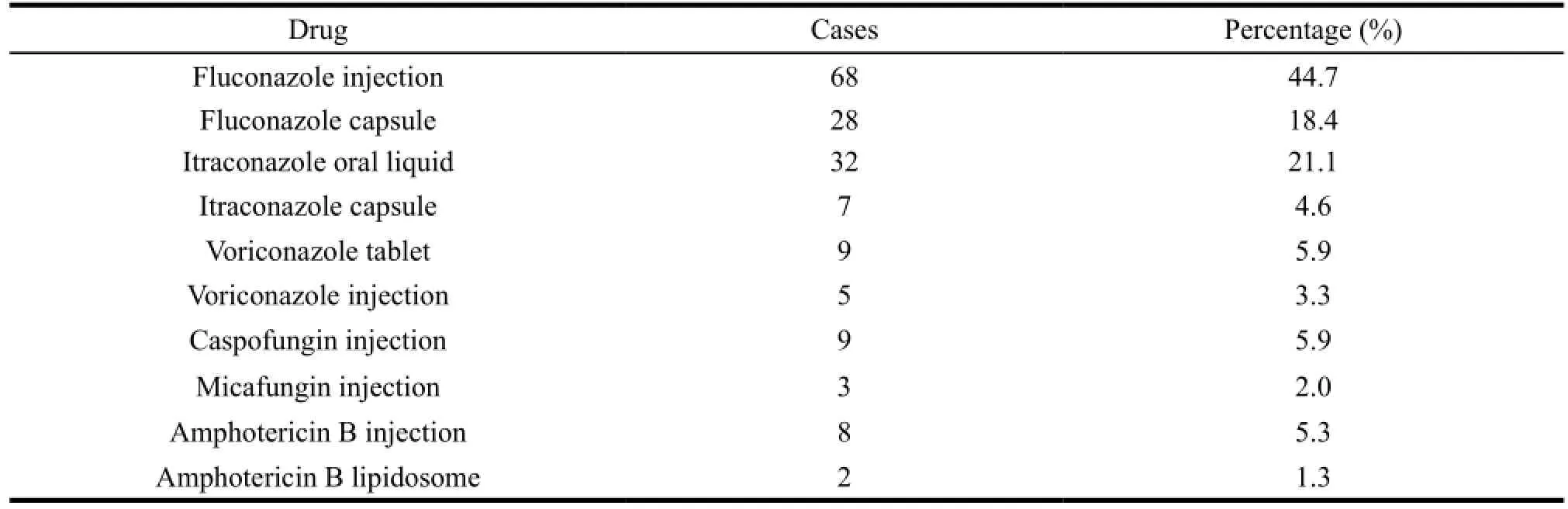
Table 4 The utilization of other antifungal drugs combined with itraconazole
Of all cases with combined antifungal, 10 cases were unreasonable, mainly for frequent replacement of antifungal without basis. This will not only increase the incidence of fungal drug resistance, but also be harmful to the recovery of the disease, and increase the economic burden of patients.
2.6 The details of other combined antibiotic
149 patients used other antibiotics jointly. Among these patients, 42 patients used 1 or 2 antibiotics and 107 patients with three or more. These antibiotics were cefodizime, cefmenoxime, cefoperazone, piperacillin tazobactam, meropenem, imipenem cilastatin, and vancomycin. The first three antibiotics had higher frequency of use.
2.7 The details of potential drug interactions
Of all the 152 patients, 37 (24.3%, see Table 5) used drugs potentially interacting with itraconazole. They were rifampicin, erythromycin, cyclosporine, tacrolimus, nifedipine, docetaxel, and methylprednisolone. The combined rate (24.3%) was 8.7% higher than the reported abroad literature[2].
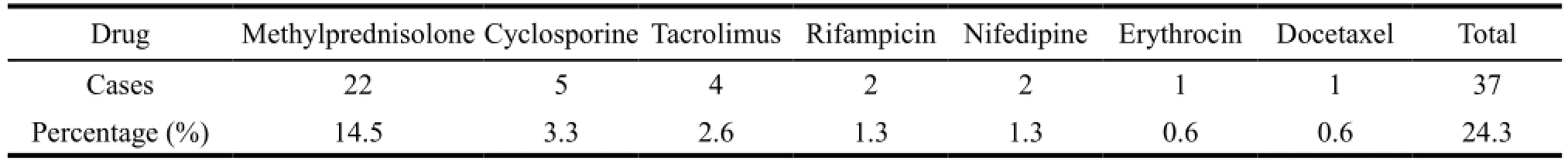
Table 5 The utilization of drugs potentially interacting with itraconazole
3 Discussions
This study indicated that the irrational clinical use of itraconazole injection was shown in four aspects:
(1) Irrational loading dose. Unused loading dose or use of non-standard loading dose accounted for 75.7%. The correct usage of itraconazole injection is: day 1 and 2, 200mg, twice daily; days 3 to 14, once a day, 200mg. The clinical efficacy of itraconazole is related with its plasma concentration. To achieve the desired concentration of itraconazole injection as soon as possible, initial treatment is a critical period. Therefore a loading dose is needed.
(2) Inadequate course of treatment. Among 152 patients, only 14 cases were reasonable. 90.1% of the patients were less than 14 days, of which 41.4% patients were only 1-3 days. A survey[3]found that when patients were diagnosed with fungal infection, clinicians were reluctant to give patients itraconazole injection or used it later, or gave small dose and short course, considering it is potentially hepatotoxic. At the same time, due to the patients’ economic condition, itraconazole injection was often replaced by lower prices antifungal or stopped using it.
(3) Combined use of drugs potentially interacting with itraconazole. 24.3 percent patients used AEDs which has interaction with itraconazole. Because of its inhibition to CYP3A4, itraconazole can affect the plasma concentration of lots of drugs that can be metabolized by CYP3A4, thus changing the drugs’ effect and adverse reaction. Such drugs are oral anticoagulants, protease inhibitors, calcium channel blockers metabolized by CYP3A4, some immunosuppressant and other drugs as digoxin, carbamazepine, buspirone, alfentanil, alprazolam, midazolam, rifabutin and methylprednisolone. Some drugs transform the plasma concentration of itraconazole through influencing CYP3A4. For examples, rifampicin, isoniazid, phenobarbital, phenytoin and carbamazepine can lower the plasma concentration of itraconazole while erythromycin, clarithromycin, ritonavir and indinavir can raise it. In clinical application, it should depend on the circumstances to adopt Therapeutic Drug Monitoring or use drugs jointly after adjusting dose. In a word, commercial and synergistic interaction should be encouraged and adverse interaction and reaction should be reduced or avoided.
(4) Frequent replacement of antifungals. 6.6 percent patients replace antifungal without basis, and it’s up to 5 kinds at most. It’s really difficult to treat deep fungal infections, due to a few alternative drugs with so many adverse reactions for antifungal. In addition, most of these patients have serious diseases. Another difficulty is that it is uncertain whether the bacterial infection is under control and then the clinicians stop using antibiotics. The difficulty of treating this disease brought some confusion to clinicians which maybe partly account for the frequent replacement of antifungals.
The results of this study show that itraconazole injection is mainly applied to hematologic malignancies patients. These patients receive chemotherapy repeatedly and use high-dose glucocorticoids, immunosuppressant and broad-spectrum antibiotics so that deep fungal infections increase significantly. Their prevalence of fungal infection on mucous membrane can be 20% to 40%. Since 1950s, amphotericin B has become the first choice to treat various kinds of serious fungal infection. The drug has a broad spectrum antifungal activity. But it is limited because of the serious adverse reactions such as nephrotoxicity, gastrointestinal reactions, phlebitis, chill, high fever and headache. It is reported by home literature that the efficiency of itraconazole injection for fungal infection and unexplained fever after hematologic malignancies chemotherapy is 76.2%. It’s similar to that of Amphotericin B by home report. For aspergillus infection, it has better effect, less side effect and good tolerance for patients. So itraconazole injection can be the first choice to treat deep fungal infection[4].
4 Conclusions
The level of clinical rational use of itraconazole needs to be improved. Taking the types of pathogens, characteristics of the drugs, primary disease status and economic status of the patients into account, clinicians are recommended to use antifungal reasonably and avoid replacing antifungal easily. During the application, an appropriate dose and appropriate course of treatment should be considered. If necessary, other drugs can be used jointlyand attention also should be paid to the correct application of the loading dose. At the same time, in order to improve the cure rate of fungal infection, effective measures must be taken to control primary diseases, avoiding long-term high-dose glucocorticoids, correcting hypoproteinemia and improving immune function.
[1] FENG Shu-ling, ZHANG Yang-lian. Pharmacotherapy of Common Fungal Infection [J]. Strait Pharmaceutical Journal, 2010, 22 (11): 142-144.
[2] Laura Galatti, Giampiero Mazzaglia, Antonella Greco, et al. Coprescriptions with Itraconazole and Fluconazole as a Signal for Possible Risk of Drug-drug Interactions: A Four-year Analysis from Italian General Practice [J]. Pharmacoepidemiology and Drug Safety, 2007, 16: 422-428.
[3] WU Jian-bo, XU Ting, LI Tian-ping, et al. Retrospective Analysis of Itraconazole’s Adverse Reactions [J]. China Pharmacist, 2008, 11 (8): 956-957.
[4] MAO Li-ping, MENG Hai-tao, QIAN Wen-bin, et al. Curative Efficacy of Itraconazole Injection in Patients with Deep Fungal Infections of Hematological Malignancies after Chemotherapy [J]. Chinese Journal of Internal Medicine, 2005, 44 (8): 618-619.
Author’s information: HUANG Tai-kang, Professor. Major research area: Social pharmacy. Tel: 029-85323243, E-mail: dwh751001@sina. com
- 亚洲社会药学杂志的其它文章
- Current Research Status of Atorvastatin Calcium
- General Influence Factors on Chinese Online Pharmacy Management: A Study Based on Literature Analysis
- British NHS and Its Enlightenment to Healthcare System Reform in China
- Development Strategies of Pharmaceutical Industry in China
- Drug Pricing Methods in Australia and Its Enlightenment
- Pharmaceutical Enterprises in China: Patent Infringement Risks and Management Strategies