脊柱侧凸患者站立位与平卧位脊柱骨盆矢状面序列差异
李杰静,郭鸿飞,赵 陆,张永刚,宋 凯,唐翔宇,苏晓静
解放军总医院 骨科专科医院脊柱外科,北京 100853
脊柱侧凸患者站立位与平卧位脊柱骨盆矢状面序列差异
李杰静,郭鸿飞,赵 陆,张永刚,宋 凯,唐翔宇,苏晓静
解放军总医院 骨科专科医院脊柱外科,北京 100853
目的比较不同体位和不同病因分型对脊柱骨盆矢状面序列的影响。方法选取我科2010年2月- 2014年6月110例脊柱侧凸患者,按病因分为特发性脊柱侧凸(31例)、先天性脊柱侧凸(36例)、神经肌肉型脊柱侧凸(32例)、退行性脊柱侧凸(11例)4组。分别行自然站立位全脊柱骨盆侧位X线和平卧位低剂量三维CT重建检查,分别测量脊柱侧凸患者矢状面平衡距离(sagittal vertical axis,SVA)、胸后凸角(Cobb T5-T12,TK)、胸腰段后凸角(Cobb T11-L2,TLK)、腰前凸角(Cobb L1-S1,LL)、骨盆入射角(pelvic incidence,PI)、骨盆倾斜角(pelvic tilt,PT)、骶骨倾斜角(sacral slope,SS),比较各组站立位与平卧位参数差异。结果从站立位到平卧位,4组TK和PT均减小(P<0.05),SS均增大(P<0.05)。退行性脊柱侧凸组SVA、LL、PI和PT与其他3组差异均有统计学意义。当从站立位变换为平卧位时,退行性脊柱侧凸组LL增大(P<0.05),而特发性脊柱侧凸组和神经肌肉型脊柱侧凸组LL均减小(P<0.05);先天性脊柱侧凸组LL差异无统计学意义。结论脊柱侧凸患者的站立位与平卧位的脊柱骨盆矢状面序列存在差异。无论站立位还是平卧位,退行性脊柱侧凸患者与特发性、先天性和神经肌肉型脊柱侧凸患者的脊柱骨盆矢状面序列明显不同。
脊柱侧凸;脊柱;骨盆;矢状面序列
脊柱侧凸是一种脊柱三维结构畸形疾病,包括结构性冠状面侧凸畸形、轴位椎体旋转和矢状面前凸的丢失。目前公认将自然站立位影像作为评价脊柱侧凸的“金标准”,但临床工作中仍会有患者携带平卧位X线或CT影像片前来就诊,这与患者初诊的医疗机构不能行站立位脊柱全长片检查或接诊医生缺乏脊柱侧凸知识有关。一些学者已经证实,冠状面的Cobb角和轴位的椎体旋转可能因为姿势的改变而发生变化[1-6]。但是对于姿势导致脊柱骨盆矢状面参数变化的研究很少。脊柱矢状面序列与临床症状有明显相关性[7-9]。因此,本研究比较不同姿势和不同病因分类对脊柱骨盆矢状面序列的影响,为没有条件行站立位的脊柱全长片检查的医疗机构医生评估脊柱侧凸时提供参考。
资料和方法
1 资料 回顾我科2010年2月- 2014年6月脊柱侧凸(包括特发性脊柱侧凸、先天性脊柱侧凸、神经肌肉型脊柱侧凸、退行性脊柱侧凸)患者的资料,均符合脊柱侧凸学会对特发性、先天性、神经肌肉型、退行性脊柱侧凸的定义。本研究中神经肌肉型脊柱侧凸的诱因仅是脊髓空洞,而不是肌无力、共济失调、感觉丧失或者其他病因导致的神经肌肉型脊柱侧凸。入选患者需要有完整的临床和影像检查资料。排除标准:肌力异常,下肢不等长,既往有脊柱或髋关节的手术史,代谢性骨病,结缔组织疾病,脊柱的骨折、感染或肿瘤等病史。最终110例入选,根据病因分类将其分为特发性脊柱侧凸、先天性脊柱侧凸、神经肌肉型脊柱侧凸、退行性脊柱侧凸4组。4组脊柱侧凸患者一般资料见表1。
2 影像学资料 包括手术前自然站立位全脊柱骨盆侧位X线和平卧位的低剂量CT扫描重建的二维矢状面脊柱骨盆影像。CT扫描时保持患者的髋、膝关节伸直。用Image-Pro Plus 6.0影像分析软件测量自然站立位的影像,用西门子CT工作站测量卧位的CT影像。测量脊柱侧凸患者以下几何参数:矢状面平衡距离(sagittal vertical axis,SVA)、胸后凸角(Cobb T5-T12,TK)、胸腰段后凸角(Cobb T11-L2,TLK)、腰前凸角(Cobb L1-S1,LL)、骨盆入射角(pelvic incidence,PI)、骨盆倾斜角(pelvic tilt,PT)、骶骨倾斜角(sacral slope,SS)。其中,颈7铅垂线落在骶1上终板后缘前方时SVA取值为正数,在后方时取值为负数。当骶1上终板中点在髋轴连线中点后方时PT取值为正数,在前方时取值为负数。当弧度为后凸时TK、TLK、LL取值为正数,前凸时取值为负数。为了减少组间和组内差异,由2名脊柱外科医生分别测量3次,各次测量间隔时间为2周,取6次测量的均值用于最终结果分析。
结 果
1 测量参数的可靠性 各参数ICC组内差异和组间差异均值为0.952和0.858,所有ICC值均>0.8。
2 站立位与平卧位参数比较 4组脊柱侧凸患者平卧位TK较站立位均显著减小(P=0.000,0.013, 0.000,0.002)。4组脊柱侧凸患者的骨盆参数PT和SS站立位与平卧位,差异有统计学意义。从站立位到平卧位,4组脊柱侧凸患者PT明显减小,而SS明显增大(图1)。4组TLK和PI差异无统计学意义。见表2。
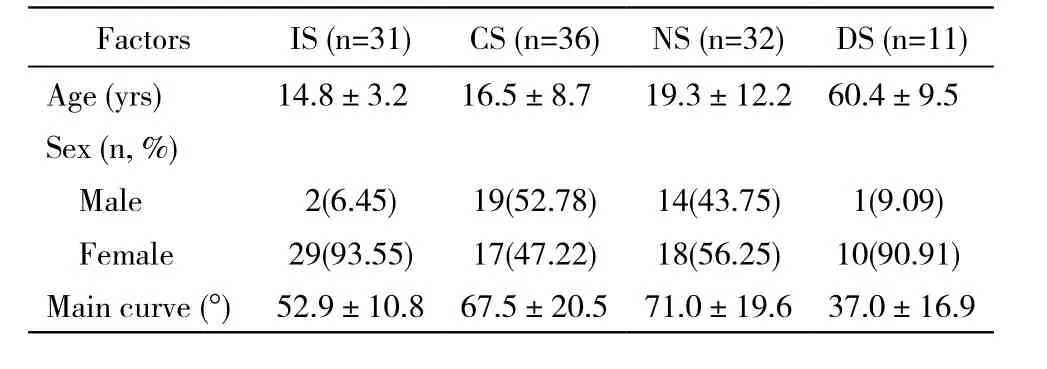
表1 特发性、先天性、神经肌肉型、退行性脊柱侧凸各组的一般资料Tab. 1 General data of idiopathic, congenital,neuromuscular and degenerative scoliosis groups
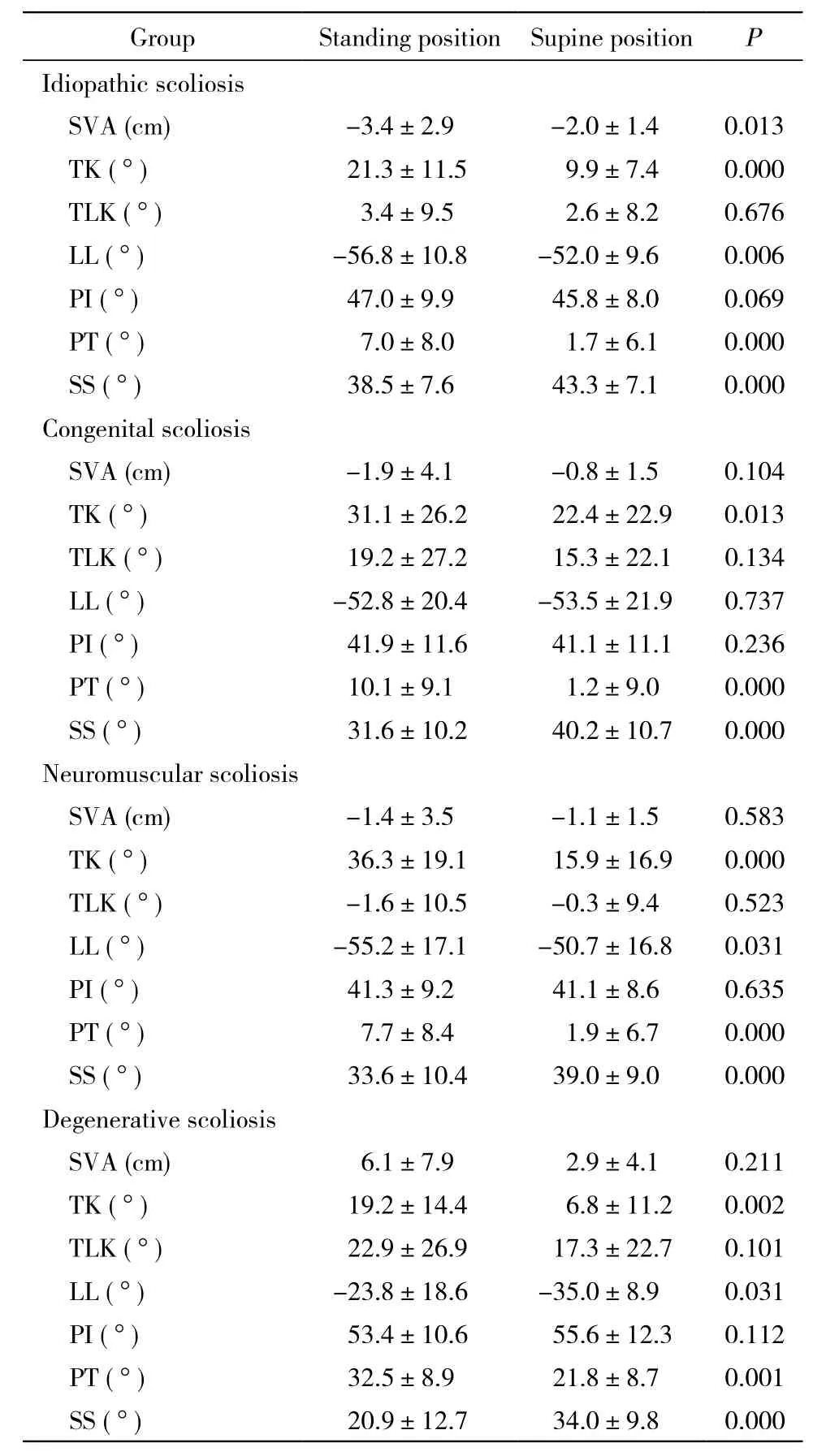
表2 4组脊柱侧凸患者站立位和平卧位矢状面脊柱骨盆参数比较Tab. 2 Comparison of standing and supine position of sagittal and pelvic parameters in four groups
3 4组间参数比较 无论站立位还是平卧位,退行性脊柱侧凸组SVA、LL、PI和PT与其他3组比较,差异均有统计学意义。退行性脊柱侧凸组SVA站立位和平卧位均数为正数,其他3组SVA站立位和平卧位均数为负数。退行性脊柱侧凸组LL与其他3组明显不同。从站立位到平卧位,退行性脊柱侧凸组LL从-23.8°±18.6°增大至-35.0°±8.9°(P=0.031)(图2),而特发性和神经肌肉型脊柱侧凸两组LL分别从-56.8°±10.8°、-55.2°±17.1°减小到-52.0°±9.6°、-50.7°±16.8° (P=0.006,0.031),先天性脊柱侧凸组LL差异无统计学意义。见表2。
讨 论
随着研究的深入,学者们证实了脊柱骨盆矢状面平衡的重要性[7-13]。一些学者推荐使用三维CT重建或MRI来评估脊柱侧凸畸形,甚至使用CT重建或MRI影像来制订治疗方案或者评价治疗效果[14-16]。许多医疗机构由于医疗条件有限,仍然使用平卧位X线来评估病情,这会影响医生对畸形严重程度的判断。学者们已经证实冠状面Cobb角和椎体旋转畸形由于检查姿势的不同而发生改变。也有报道证明,正常人群或者腰痛患者的腰椎形态,由于站立位、坐位或者平卧位等检查姿势的不同而发生变化[16-20]。
本研究发现,4组脊柱侧凸患者站立位PT均比平卧位大,相反站立位SS均较平卧位小,且差异均有统计学意义,这一结果在之前的脊柱侧凸研究中未见报道。Eddine等[21]报道了一组24名健康人的研究,得出了类似结果。他们发现当姿势从平卧变为站立时,骨盆位置参数发生明显变化,22名研究对象的骨盆平均后旋了7°,另外2名研究对象的骨盆平均前旋了3°。Legaye等[11]发现无论是正常人群或是侧凸患者,PI与SS明显相关,而SS又决定了LL。椎体和骨盆是通过椎间盘、小关节和肌肉软组织连接在一起的。以上均提示从站立位到平卧位时,骨盆的旋转使LL增大。
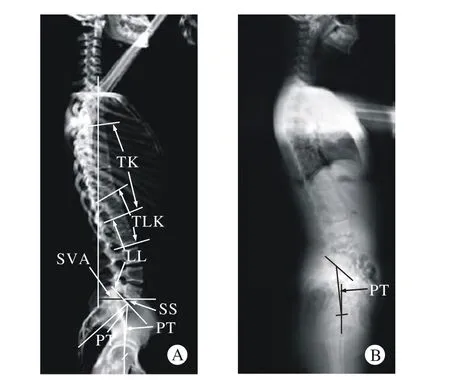
图 1 特发性脊柱侧凸患者平卧位和站立位影像的脊柱骨盆矢状面序列比较A:特发性脊柱侧凸患者术前CT扫描重建的平卧位矢状面二维影像; B:同一患者术前自然站立位侧位全长片Fig. 1 Radiographic example of a patient with idiopathic scoliosis in supine and standing position. The PT of supine position is obviously different with the PT of standing positionA: Preoperative supine sagittal two dimensional images reconstructed from CT scan using a low-dose scanning protocol; B: Preoperative natural standing sagittal plain radiographs of the same patient
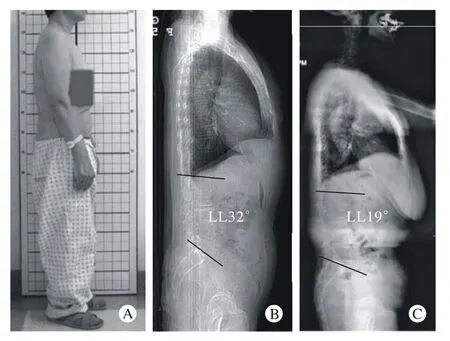
图 2 退行性脊柱侧凸患者站立侧位外观照及平卧位和站立位影像的脊柱骨盆矢状面序列比较A:退行性脊柱侧凸患者术前外院平卧位矢状位X线提示腰前凸32°;B:该患者的侧位外观照;C:该患者术前我院站立位脊柱全长片提示19°Fig. 2 The patient’s appearance and supine lateral radiographs may confuse the doctor’s judgment of the severity of scoliosisA: The appearance of a patient with degenerative scoliosis. B: Supine lateral radiograph of this patient shows that lumbar lordosis is 32° in another hospital. C: Upright long cassette lateral radiograph of the same patient shows that lumbar lordosis is 19° in our hospital
Lee等[19]认为年轻人从站立变为平卧时,上腰椎对LL影响要比下腰椎对LL影响大,但是该研究未考虑到姿势变换时胸椎和骶骨对LL的作用。胸腰段椎体像纽带一样连接着胸后凸和腰前凸,并且维系着它们之间的平衡。从站立位到平卧位,由于TK减小,胸椎的终板更接近于垂直于人体的长轴,进而导致上腰椎的前凸变小。Wood等[17]证实了站立位的腰前凸和胸腰段后凸明显比平卧位的大。本研究同样显示,特发性和神经肌肉型脊柱侧凸患者从站立到平卧LL明显变小,表明特发性和神经肌肉型脊柱侧凸患者,当姿势从站立位变为平卧位时,TK减小导致LL减小的度数大于骨盆前旋导致LL增大的度数。
本研究中先天性脊柱侧凸组患者大部分是楔形椎或半椎体畸形,并且这些畸形椎体多数都位于胸腰段,多数半椎体都在上下椎体间的后外侧。这一结构改变可能会影响局部椎体的活动度,并且可能增加胸腰段后凸。这可能是姿势改变时,先天性脊柱侧凸组LL没有显著变化的原因。
许多研究已经证明腰椎退行性脊柱侧凸患者的腰前凸较小。Jackson等[22]发现在成年志愿者、有症状的腰椎间盘退变患者、特发性或者退行性脊柱侧凸患者中,如果腰前凸较小,会表现出典型的SVA很大的前倾站立姿势。本研究中退行性脊柱侧凸组也表现出LL较小、SVA较大的站立姿势,同时骨盆后旋来保持脊柱矢状面序列的平衡。因此站立位时退行性脊柱侧凸组SS比其他3组大,而PT比其他3组小。当退行性脊柱侧凸患者从站立到平卧时,脊柱会后移并且骨盆会前旋。Lee等[19]证明了当姿势从站立到平卧时,老年人上腰椎的活动度较青年人小。因此当姿势从站立到平卧时,骨盆前旋导致了退行性脊柱侧凸患者LL的增大。
Harimaya等[23]发现,手术前腰前凸不足的成年脊柱畸形患者平卧或者术中俯卧位时,他们的腰前凸较术前站立位大,术前平卧位腰前凸与术中俯卧位腰前凸没有显著差异。
综上,我们推断脊柱侧凸患者平卧位的脊柱骨盆矢状面整体形态和平衡可能与术中俯卧位相似。鉴于收集俯卧位整体的脊柱骨盆影像资料比较困难,目前这一假设未能得到证实,还需进一步研究论证。由于X线暴露等原因,一般在脊柱侧凸患者达到手术标准,需要进一步评估病情时才有针对性地对患者行脊柱CT检查,故本研究样本量有限,暂不能针对不同严重程度脊柱侧凸是否会对脊柱骨盆矢状面序列各参数产生影响进行更加深入的研究,需要在今后进一步完善。
1 Lee MC, Solomito M, Patel A. Supine magnetic resonance imaging Cobb measurements for idiopathic scoliosis are linearly related to measurements from standing plain radiographs[J]. Spine (Phila Pa 1976), 2013, 38(11): E656-E661.
2 Wessberg P, Danielson BI, Willen J. Comparison of Cobb angles in idiopathic scoliosis on standing radiographs and supine axially loaded MRI[J]. Spine (Phila Pa 1976), 2006, 31(26): 3039-3044.
3 Torell G, Nachemson A, Haderspeck-Grib K, et al. Standing and supine Cobb measures in girls with idiopathic scoliosis[J]. Spine(Phila Pa 1976), 1985, 10(5):425-427.
4 Keenan BE, Izatt MT, Askin GN, et al. Supine to standing Cobb angle change in idiopathic scoliosis: the effect of endplate preselection[J]. Scoliosis, 2014, 9:16.
5 Lee CS, Hwang CJ, Lee SW, et al. Changes of deformity due to the position and anesthesia in adolescent idiopathic scoliosis[J]. J Spinal Disord Tech, 2010, 23(6): 377-382.
6 Yazici M, Acaroglu ER, Alanay A, et al. Measurement of vertebral rotation in standing versus supine position in adolescent idiopathic scoliosis[J]. J Pediatr Orthop, 2001, 21(2): 252-256.
7 Lagrone MO, Bradford DS, Moe JH, et al. Treatment of symptomatic flatback after spinal fusion[J]. J Bone Joint Surg Am, 1988, 70(4):569-580.
8 Chaléat-Valayer E, Mac-Thiong JM, Paquet J, et al. Sagittal spino-pelvic alignment in chronic low back pain[J]. Eur Spine J,2011, 20(Suppl 5): 634-640.
9 Bernstein P, Hentschel S, Platzek I, et al. Thoracal flat back is a risk factor for lumbar disc degeneration after scoliosis surgery[J]. Spine J, 2014, 14(6): 925-932.
10 Vedantam R, Lenke LG, Keeney JA, et al. Comparison of standing sagittal spinal alignment in asymptomatic adolescents and adults[J]. Spine (Phila Pa 1976), 1998, 23(2):211-215.
11 Legaye J, Duval-Beaupère G, Hecquet J, et al. Pelvic incidence:a fundamental pelvic parameter for three-dimensional regulation of spinal sagittal curves[J]. Eur Spine J, 1998, 7(2):99-103.
12 Roussouly P, Gollogly S, Berthonnaud E, et al. Classification of the normal variation in the sagittal alignment of the human lumbar spine and pelvis in the standing position[J]. Spine (Phila Pa 1976),2005, 30(3): 346-353.
13 Glassman SD, Bridwell K, Dimar JR, et al. The impact of positive sagittal balance in adult spinal deformity[J]. Spine (Phila Pa 1976), 2005, 30(18): 2024-2029.
14 Guarino J, Tennyson S, McCain G, et al. Rapid prototyping technology for surgeries of the pediatric spine and pelvis: benefits analysis[J]. J Pediatr Orthop, 2007, 27(8):955-960.
15 Mao K, Wang Y, Xiao S, et al. Clinical application of computerdesigned polystyrene models in complex severe spinal deformities: a pilot study[J]. Eur Spine J, 2010, 19(5): 797-802.
16 Scheufler KM, Cyron D, Dohmen HA. Less invasive surgical correction of adult degenerative scoliosis, part I: technique and radiographic results[J]. Neurosurgery, 2010, 67(3): 696-710.
17 Wood KB, Kos P, Schendel M, et al. Effect of patient position on the sagittal-plane profile of the thoracolumbar spine[J]. J Spinal Disord, 1996, 9(2):165-169.
18 Mauch F, Jung C, Huth J, et al. Changes in the lumbar spine of athletes from supine to the True-Standing position in magnetic resonance imaging[J]. Spine (Phila Pa 1976), 2010, 35(9):1002-1007.
19 Lee ES, Ko CW, Suh SW, et al. The effect of age on sagittal plane profile of the lumbar spine according to standing, supine, and various sitting positions[J]. J Orthop Surg Res, 2014, 9(1): 11.
20 Dolan P, Adams MA, Hutton WC. Commonly adopted postures and their effect on the lumbar spine[J]. Spine (Phila Pa 1976), 1988,13(2): 197-201.
21 Eddine TA, Migaud H, Chantelot C, et al. Variations of pelvic anteversion in the lying and standing positions: analysis of 24 control subjects and implications for CT measurement of position of a prosthetic cup[J]. Surg Radiol Anat, 2001, 23(2):105-110.
22 Jackson RP, Peterson MD, McManus AC, et al. Compensatory spinopelvic balance over the hip axis and better reliability in measuring lordosis to the pelvic radius on standing lateral radiographs of adult volunteers and patients[J]. Spine (Phila Pa 1976), 1998,23(16):1750-1767.
23 Harimaya K, Lenke LG, Mishiro TA, et al. Increasing lumbar lordosis of adult spinal deformity patients via intraoperative prone positioning[J]. Spine (Phila Pa 1976), 2009, 34(22): 2406-2412.
Changes of sagittal spino-pelvic alignment in scoliosis patients in standing and supine position
LI Jiejing, GUO Hongfei, ZHAO Lu, ZHANG Yonggang, SONG Kai, TANG Xiangyu, SU Xiaojing
Department of Orthopedics, Chinese PLA General Hospital, Beijing 100853, China
ZHANG Yonggang. Email: zhangyg301@hotmail.com
ObjectiveTo compare the influence of different position and diverse pathogeny in patients on sagittal spino-pelvic balance.MethodsOne hundred and ten patients with scoliosis were included in this retrospective study. They were divided into four groups according to pathogeny: idiopathic scoliosis group (n=31), congenital scoliosis group (n=36), neuromuscular scoliosis group (n=32) and degenerative scoliosis group (n=11). Sagittal vertical axis (SVA), thoracic kyphosis (TK), thoracolumbar kyphosis (TLK), lumbar lordosis (LL), pelvic incidence (PI), pelvic tilt (PT), and sacral slope (SS) were measured on preoperative upright and supine lateral radiographs.ResultsThe TK and PT decreased, and SS increased when the position changed from standing to supine in the four groups (P<0.05). Compared with the other three groups, the SVA, LL, PI and PT of degenerative scoliosis group showed statistically significant difference no matter in which positions. The LL of degenerative scoliosis group increased (P<0.05) when the position changed from standing to supine. In contrast, the LL of idiopathic and neuromuscular scoliosis group decreased (P<0.05). However, the congenital scoliosis group showed no significant difference in LL.ConclusionThis study shows that the sagittal alignment of scoliosis in standing position is different with which in supine position. And neither in upright nor in supine position, the sagittal parameters of degenerative scoliosis is different with the idiopathic, congenital and neuromuscular scoliosis.
scoliosis; spine; pelvis; sagittal alignment
R 682.3
A
2095-5227(2015)06-0603-04
10.3969/j.issn.2095-5227.2015.06.022
时间:2015-03-20 10:11
http://www.cnki.net/kcms/detail/11.3275.R.20150320.1011.002.html
2015-01-22
李杰静,男,在读硕士,医师。研究方向:脊柱畸形的诊治。Email: 89721610@qq.com
张永刚,男,博士,主任医师,博士生导师,解放军总医院骨科医院副院长兼脊柱外科主任。Email: zhangyg301@hotmail. com