Pattern of acute poisoning in Jimma University Specialized Hospital, South West Ethiopia
Eyosias Teklemariam, Shibiru Tesema, Awol Jemal Department of Pharmacy, College of Health Sciences, Jimma University, Jimma, Ethiopia Corresponding Author: Shibiru Tesema, Email: shibtesema007@yahoo.com
Pattern of acute poisoning in Jimma University Specialized Hospital, South West Ethiopia
Eyosias Teklemariam, Shibiru Tesema, Awol Jemal Department of Pharmacy, College of Health Sciences, Jimma University, Jimma, Ethiopia Corresponding Author: Shibiru Tesema, Email: shibtesema007@yahoo.com
BACKGROUND: Poisoning is a common cause of morbidity and mortality worldwide. People can be exposed to poisons either intentionally or accidentally. Designing appropriate treatment or prevention approaches depends on understanding of the nature and pattern of poisoning in a specifi c place. Information on the patterns of acute poisoning in Ethiopian hospitals is limited. This study was, therefore, conducted to evaluate the patterns of acute poisoning in Jimma University Specialized Hospital (JUSH), South West Ethiopia.
METHODS: A record based retrospective analysis of acute poisoning cases presented to JUSH from January 1, 2012 to December 31, 2013 was conducted. The collected data was analyzed using SPSS version 16.
RESULTS: Of the 103 patients, 49 (47.6%) were male and 54 (52.4%) were female. The highest prevalence of poisoning was observed in persons aged 12–20 years (70, 67.96%). Majority of the cases were intentional poisoning (52, 50.5%), and 28 (27.2%) of the cases were accidental. The common causes of poisoning were house hold cleansing agents (43, 41.7%), organophosphates (28, 27.2%) and drugs (13, 12.6%). Diarrhea and vomiting (49.5%), altered consciousness (16.5%) and epigastric pain (13.6%) were the common presenting symptoms.
CONCLUSION: Majority of the victims of the acute poisoning in this study were aged 12–20 years. The most common mode of poisoning was intentional poisoning resulting from temporary quarrel. The common poisons used by the victims were found to be household cleansing agents.
Poisoning; Mode; Reasons
World J Emerg Med 2016;7(4):290–293
INTRODUCTION
Poisoning either accidental or intentional is a significant global public health problem. According to WHO estimates, in 2004 there were 346 000 deaths worldwide from unintentional poisoning. Of these deaths, 91% occurred in low- and middle-income countries. In the same year, unintentional poisoning caused the loss of over 7.4 million years of healthy life (disability adjusted life years, DALYs).[1]Poisoning is one of the major causes of patient admissions to emergency departments and intensive care units, especially in developing countries.[2]
The prevalence and types of poisoning vary considerably across the world and depend on socioeconomic status and cultural practices, as well as on local industrial and agricultural activities.[3]Advances in technology and social development have resulted in the availability of most drugs and chemical substances in the community.[4,5]
Household chemical agents and prescribed drugs are the most common poisoning agents in developed world, but agro-chemicals are the most common poisoning agents in developing countries.[6]The pesticides used for agricultural purposes are easily available in the market and poisoning with such products are more commonly noticed in rural area where people largely depend on agriculture for their living.[7]Despite the rapidly growing role of chemicals in their economies, many Africancountries like Ethiopia lack poison centres, toxicological expertise among health professionals and laboratory analytical facilities which may increase the likeliwood of adverse health impacts.[8]
Continuous surveillance of cases of acute poisoning is important for planning and evaluating public health interventions.[9]It is important to know the nature and severity of poisoning in order to take appropriate preventive measures. There has been no study of this nature conducted at Jimma University Specialized Hospital (JUSH) to date, hence this study was carried out with the objectives to assess patterns of acute poisonings along with various parameters such as poisoning mode, type of poison used, and outcomes of acute poisoning cases presented to JUSH over a period of one year.
METHODS
Retrospective analysis of poisoning case records was conducted among attendants of JUSH from January 1, 2012 to December 31, 2013. JUSH is one of the few teaching hospitals in the country, and the only referral hospital in the south west part of Ethiopia. It is located in Jimma town, Oromia region, 346 km from the capital city, Addis Abeba. It has four major clinical departments (Internal medicine, surgery, pediatrics and OB/GYN) and four minor departments (psychiatry, ophthalmology, dermatology, and dentistry) along with other follow up and special clinics for specifi c diseases.
All patients seen at medical and pediatric OPD and patients admitted to the medical and pediatrics ward with case of acute poisoning from January 1, 2012 to December 31, 2013 were included in the study.
Data was collected using a structured format, from the patient cards by the principal investigator. The collected data was summarized and analyzed using SPSS version 16.0.
Ethical consideration
Formal letter written by pharmacy department, Jimma University was sent to the hospital's documentation department. The objective of the study was briefed to the staff of documentation department. Documents were kept confi dential.
RESULTS
During the specifi ed study period, there were a total of 110 patients with acute poisoning cases seen at JUSH.
However, only the 103 patient cards with adequate information were included in this study.
Table 1 showed out of the total 103 patients, 49 (47.6%) were males and 54 (52.4%) were females. The highest prevalence of poisoning was in persons aged 12–20 years (70, 67.96%), followed by ages less than 12 years (15.5%). Majority of the victims were Muslims (49, 47.6%) followed by Orthodox Christians (37, 35.9%).
Majority of the cases were intentional poisoning (52, 50.5%), 28 (27.2%) were accidental, and in the rest of the cases, circumstances of poisoning was not specifi ed (23, 22.3%). Intentional poisoning was signifantly associated (P<0.05) with the age (P=0.0002) and the marital status of the victims (P<0.0001).
The most common involved toxic agents were house hold cleansing agents (43, 41.7%), organophosphates (28, 27.2%) and drugs (phenobarbitone and antidepressants) (13, 12.6%), alcohol (9, 8.7%), and hydrocarbons (benzene, kerosene) (6, 5.8%) (Figure 1).
Among 54 patients who reported their reason for poisoning, quarrel (family, marital) (41, 75.9%), psychiatric problem (8, 14.8%) and substance abuse (5, 9.3%) were frequently cited.
Most of the patients were presented to the hospital between 30 minutes and 1 hour after exposure (54, 52.4%), and only 9 (8.7%) arrived within 30 minutes. The rest arrived between 1 hour and 24 hours (40, 38.8%).
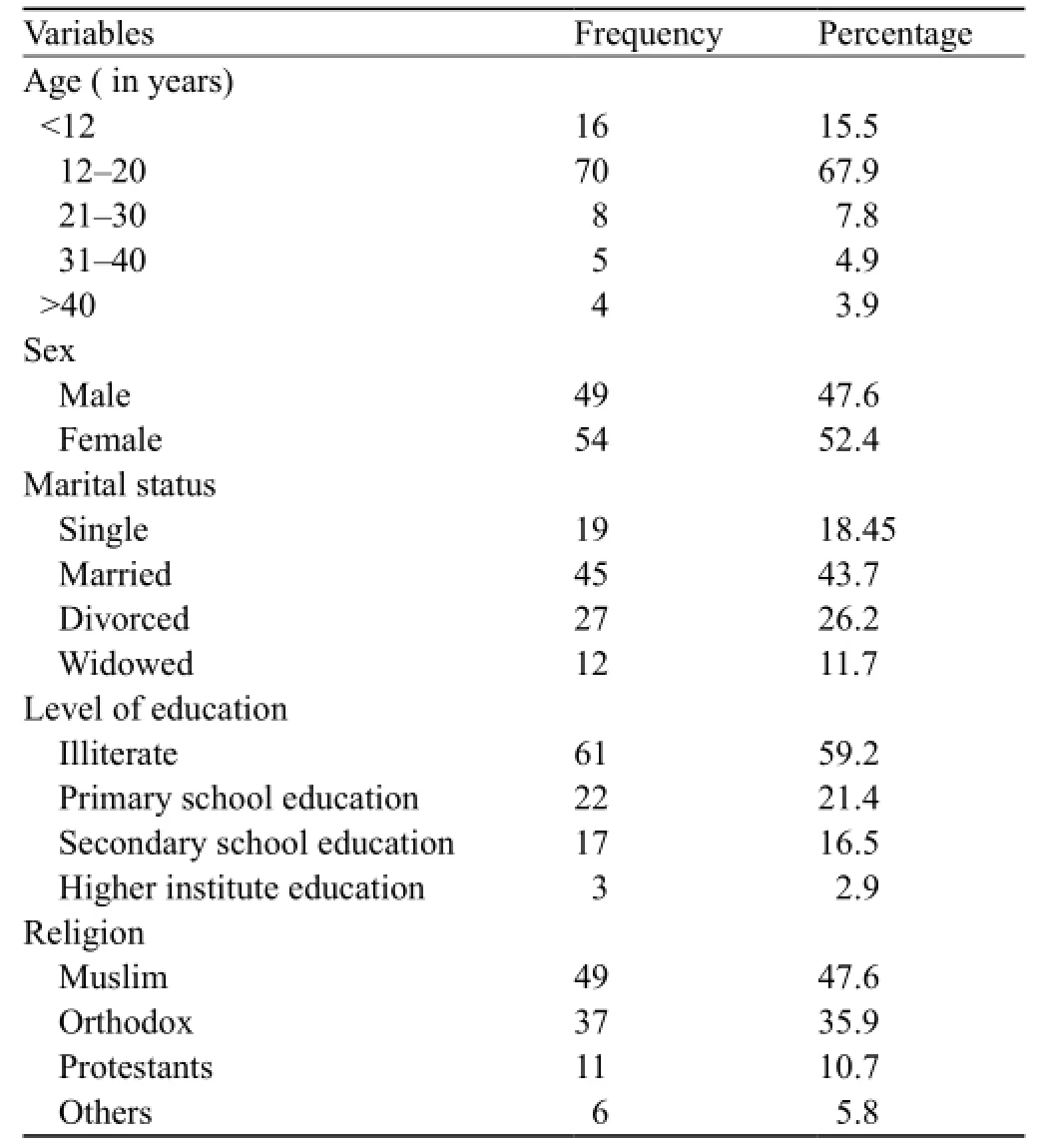
Table 1. Socio-demographic characteristics of the patients
Almost in all cases of poisoning the route of exposure was through oral ingestion accounting for 97.1% (100), and the rest was through inhalation (3, 2.9%).
Diarrhea and vomiting, altered consciousness, and epigastric pain were the most common presenting symptoms accounting for 49.5% (51), 16.5% (17), and 13.6% (14) respectively (Figure 2).
GI decontamination and specific antidotes were given in 81 (78.6%) and 13 (12.6%) of the patients respectively. The rest of the victims obtained other managements (9, 8.7%). Most of the cases were improved and discharged (63, 61.2%). The case fatality rate was 5.8% (6). Psychiatric referral and specific education on further prevention was given in 8.7% and 40.8% of the cases respectively during discharge.
DISCUSSION
The majority of the poisoning victims were in ages between 12 and 20 years (70, 67.96%), followed by ages less than 12 years accounting for 15.5%. This indicates that poisoning was most prevalent in adults which was largely intentional and in children who were accidentally exposed to toxic agents. This fi nding is consistent with a study in Turkey where many patients were between the ages of 16 and 25 years (46.9%).[10]With regard to sex distribution, poisoning was found to be slightly higher in females than in males, with 1.10:1 female to male ratio which is comparable to the fi ndings of other studies.[11,12]
有些疫苗,例如甲肝和脊髓灰质炎疫苗,国产的是减毒活疫苗,是活的病毒,而进口的是灭活疫苗,是死的病毒。中国已经没有自然感染的小儿麻痹症了,反而是有因为服用糖丸引起的小儿麻痹症,虽然概率很小,但是也要注意。
The toxic agents causing poisoning in this study were similar to other local study done at Tikur Anbessa Specialized Teaching Hospital (TASTH),[11]the most common cause of poisoning being household cleansing agents and organophosphates. A study in South Africa similarly reported household chemicals as the leading poisoning agents (45.7%).[13]
Poisoning can occur either accidentally or intentionally. Intentional poisoning was the most common mode of poisoning (50.5%) in this study, which is in agreement with the fi ndings of other studies done in Nepal (56.4%)[5]and TASTH, Ethiopia (96.5%),[11]Ondokuz Mayis University Hospital (68.6%),[10]Rift Valley Provincial General Hospital, Nakuru, Kenya (48.96%),[14]tertiary care hospital, Salem, Tamilnadu (98.66%).[15]People may intentionally poison themselves because of various reasons. Temporary quarrel with a family member or a spouse was the most common (41, 75.9%) underlying cause of the intentional poisonings in the present study. Similar result have been reported in another local study.[11]
Diarrhea and vomiting was the major presenting symptom (49.5%) followed by altered consciousnes (16.5%) and epigastric pain (13.6%). GI decontamination (78.6%) was the most common management approach employed for the victims in this study. This can be explained by the fact that majority of the patients presented before or exactly one hour post-poisoning, and is consistent with another local study report.[16]
As per this study, most of the cases were improved and discharged (63, 61.2%). The case fatality rate was 5.8%. This fi nding is comparable to the reported mortality rates in some other local studies.[11,16]Oral injestion was the most common route of exposure (100, 97.1%), which is consistent with the result reported in other studies.[6,17]
In conclusion, the present study showed that the most affected age group was 12–20 years. The common agents involved in causing poisoning were found to be household cleansing agents. The most common mode of poisoning was intentional resulting from temporary quarrel.
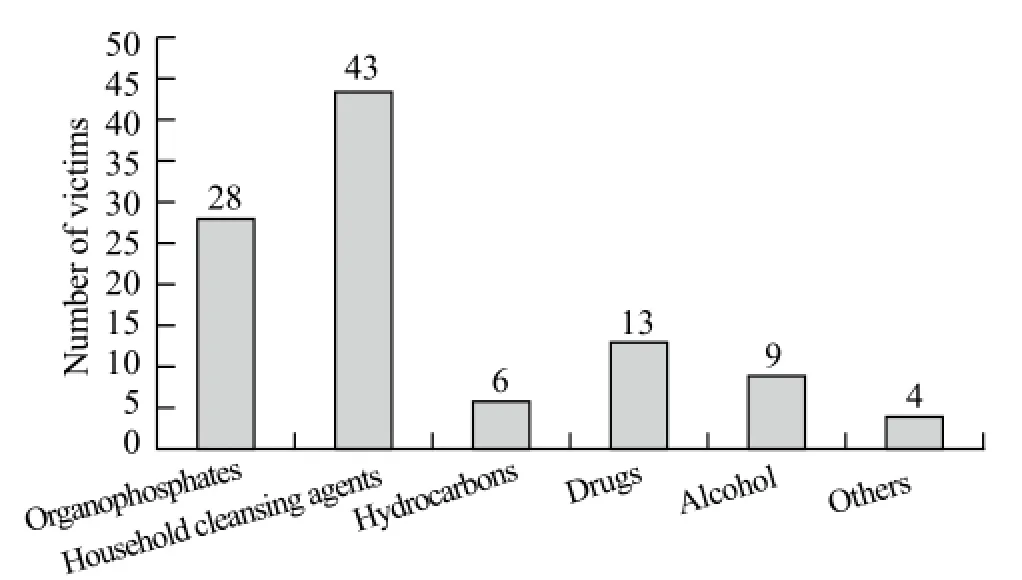
Figure 1. Types of poisoning substances involved in the poisoning cases.
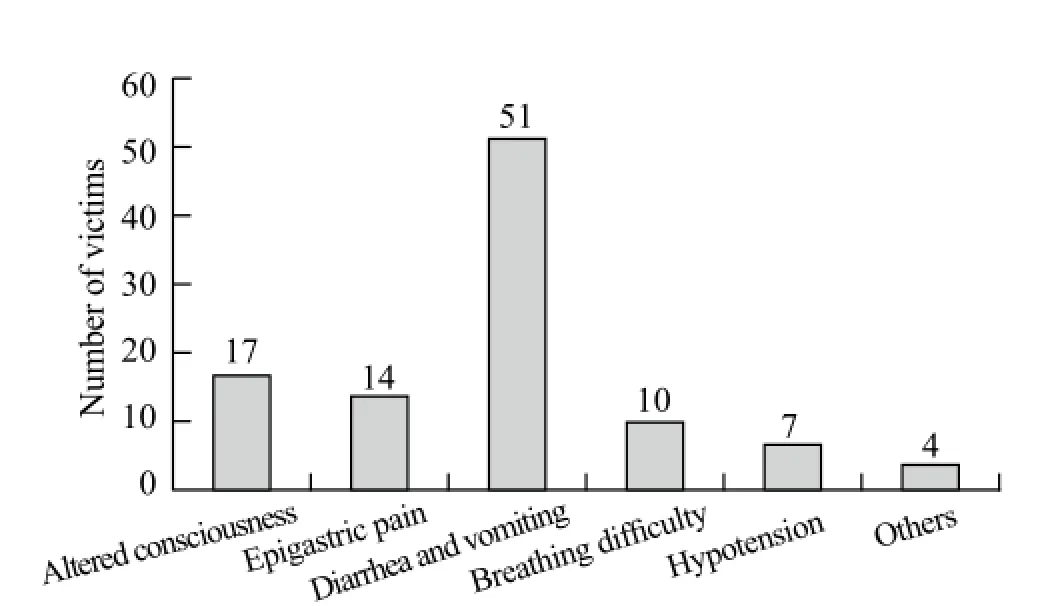
Figure 2. Clinical presentations of the acute poisoning cases.
ACKNOWLEDGEMENT
The authors express their gratitude to Jimma University for its financial support. We would also like to thank the hospital administration for allowing us to conduct this study in their hospital.
Ethical approval: The study was approved by the Institutional Review Board of the hospital.
Conflicts of interest: The authors declare there is no competing interest related to the study, authors, other individuals or organizations.
Contributors: Teklemariam E proposed the study and wrote the fi rst draft. All authors read and approved the fi nal version of the paper.
REFERENCES
1 WHO. The intentional program on chemical safety (IPCS) -poisoning prevention and management, 2010.
2 Zöhre E, Ayrik C, Bozkurt S, Kose A, Narci H, Cevik I, et al. Retrospective analysis of poisoning cases admitted to the emergency medicine. Arch Iran Med 2015; 18: 117–122.
3 Hassan BA, Siam MG. Patterns of acute poisoning in childhood in Zagazig, Egypt: an epidemiological study. Int Sch Res Notices 2014; 2014: 245279.
4 Moazzam M, Al-Saigul AM, Naguib M, Al Alfi MA. Pattern of acute poisoning in Al-Qassim region: a surveillance report from Saudi Arabia, 1999–2003. East Mediterr Health J 2009; 15: 1005–1010.
5 Pokhrel D, Pant S, Pradhan A, Mansoor S. A comparative retrospective study of poisoning cases in central, zonal and district hospitals. Kathmandu University Journal of Science, Engineering and Technology 2008; 1: 40–48.
6 Sheetu MK, Naik JD, Thakur MS, Langare SD, Pandey VO. Retrospective analysis of poisoning cases admitted in a tertiary care hospital. International Journal of Recent Trends in Science and Technology 2014;10: 365–368.
7 Naveen N, Madhuvardhana T, Arun M, Balakrishna Rao AJ, Kagne RN. Profile of suicidal poisoning in Puducherry area. International Journal of Recent Trends in Science and Technology 2015; 14: 76–79.
8 WHO. Improving the availability of poisons centre services in Eastern Africa. Highlights from a Feasibility Study for a Subregional Poison Centre in the Eastern Africa Subregion, including a toolkit on setting up a poisons information service. 2015.
9 Senarathna L, Buckley NA, Jayamanna SF, Kelly PJ, Dibley MJ, Dawso AH. Validity of referral hospitals for the toxicovigilance of acute poisoning in Sri Lanka. Bull World Health Organ 2012; 90: 436–443A.
10 Baydin A, Yardan T, Aygun D, Doganay Z, Nargis C, Incealtin O. Retrospective evaluation of emergency service patients with poisoning: a 3-year study. Adv Ther 2005; 22: 650–658.
11 Desalew M, Aklilu A, Addisu M, Ethiopia T. Pattern of acute adult poisoning at Tikur Anbessa specialized teaching hospital, a retrospective study, Ethiopia. Hum Exp Toxicol 2011; 30: 523–527.
12 Singh DP, Aacharya RP. Pattern of poisoning cases in Bir Hospital. Journal of Institute of Medicine 2006; 28: 1–6.
13 Malangu N, Ogunbanjo GA. A profile of acute poisoning at selected hospitals in South Africa. South Afr J Epidemiol Infect 2009; 24: 14–16.
14 Bundotich Jk, Gichuhi MM. Acute poisoning in the Rift Valley Provincial General Hospital, Nakuru, Kenya: January to June 2012. South African Family Practice 2015; 57: 214–218.
15 Maharani B, Vijayakumari N. Profile of poisoning cases in a tertiary care hospital, Tamil Nadu, India. Journal of Applied Pharmaceutical Science 2013; 3: 91–94.
16 Abula T, Wondmikun Y. Pattern of acute poisoning in a teaching hospital, North West Ethiopia. Ethiop Med J 2006; 44: 183–189.
17 Al-Barraq A, Farahat F. Pattern and determinants of poisoning in a teaching hospital in Riyadh, Saudi Arabia. Saudi Pharm J 2011; 19: 57–63.
Accepted after revision July 25, 2016
10.5847/wjem.j.1920–8642.2016.04.009
Original Article
January 21, 2016
 World journal of emergency medicine2016年4期
World journal of emergency medicine2016年4期
- World journal of emergency medicine的其它文章
- The state and future of emergency medicine in Macedonia
- Amiodaron in atrial fi brillation: post coronary artery bypass graft
- Short lessons in basic life support improve self-assurance in performing cardiopulmonary resuscitation
- Is current training in basic and advanced cardiac life support (BLS & ACLS) effective? A study of BLS & ACLS knowledge amongst healthcare professionals of North-Kerala
- Effects of a general practitioner cooperative co-located with an emergency department on patient throughput
- Acute Care/Trauma Surgeon's role in obstetrical/ gynecologic emergencies (The OBCAT Alert)
