Procedural simulation: medical student preference and value of three task trainers for ultrasound guided regional anesthesia
Shadi Lahham, Taylaur Smith, Jessa Baker, Amanda Purdy, Erica Frumin, Bret Winners, Sean P. Wilson,Abdulatif Gari, John C. Fox
1 Department of Emergency Medicine, University of California, Irvine, Orange, California 92868, USA
2 UC Irvine School of Medicine, Irvine, California, USA
Original Article
Procedural simulation: medical student preference and value of three task trainers for ultrasound guided regional anesthesia
Shadi Lahham1, Taylaur Smith2, Jessa Baker2, Amanda Purdy2, Erica Frumin1, Bret Winners1, Sean P. Wilson1,Abdulatif Gari1, John C. Fox1
1Department of Emergency Medicine, University of California, Irvine, Orange, California 92868, USA
2UC Irvine School of Medicine, Irvine, California, USA
Ultrasound guided nerve block; Task trainer; Regional anesthesia
INTRODUCTION
Ultrasound guided regional anesthesia has been shown to have many practical uses in emergency situations including shoulder reduction, extremity injury, abscess drainage or localized severe burns.[1–5]When properly performed, regional nerve blocks have an improved safety profile, and decrease the need for nursing and monitoring when compared to procedural sedation.[6,7]However, these procedures are not without complications and still require proper technique and sterile precautions.[8]These risks can be minimized with the use of ultrasound and effective training methods.[8,9]
Traditionally, regional anesthesia has been taught within anesthesiology residency training programs using models and anatomic guidance.[10]Recently, this technique has been done using ultrasound guidance.While real-time ultrasound has allowed the practitioner to dynamically guide the needle tip toward it's target, it does require training to optimize the technique. Initially,resident physicians and medical students may not have sufficient exposure to performing these procedures.Thus, residency programs and medical schools have incorporated simulation training to allow for multiple clinical attempts. Several models have been used for this purpose, however, there is variability in model technology, image acquisition, cost, and their overall efficacy.[11–13]
Chao et al[14]has shown that practitioners are more comfortable and more successful in executing regional blocks after simulation training. However, few studies have evaluated which models are best for training.Currently, high fidelity and low fidelity models are used for teaching. High fidelity models include a staged clinical patient encounter or cadaveric model; whereas lower fidelity models include phantom models and task trainers.While both classes have inherent limitations, low fidelity models tend to be more frequently used due to their lower cost, ease of use and availability. Commercially available models are also used, however their significantly higher cost can be prohibitive. An alternative has been to create"homemade" models which can potentially provide similar fidelity at a lower cost. While these models are often used, the literature is sparse regarding their efficacy when compared with the more costly high fidelity ones.
The purpose of this study is to compare three different regional nerve block task trainer models(homemade gelatin model, a homemade tofu model and a commercially available model manufactured by Blue Phantom) to determine self-reported performance at an ultrasound training session.
METHODS
We conducted a prospective, observational study and recruited participants from an ultrasound guided nerve block educational tutorial event held January 24 th,2015. All participants provided both verbal and written consent prior to participation in the study. The study was approved by our institutional review board (IRB).
Participants consisted of medical students of varying degrees of experience. This included first, second, third and fourth year medical students. The students were from various American medical schools and had variable ultrasound experience. All participants were recruited following an ultrasound guided regional nerve block tutorial. All participants approached for enrollment in the study were over the age of 18 and fl uent in English.
Prior to enrollment in the study, we gave all participants a 15-minute oral and visual tutorial using a PowerPoint presentation (Microsoft, Seattle, WA). This presentation included images and videos of ultrasound guided nerve blocks on both live models and task trainers. Following the tutorial, we asked participants to utilize ultrasound to visualize basic anatomy of the brachial plexus on each other using a GE Venue 50 ultrasound machine with a linear probe at a frequency of 5–10 MHz (General Electric,Wauwatosa, WI, USA). No attempt was made to provide regional anesthesia on participants. Once participants felt comfortable identifying the brachial plexus on each other,they then attempted ultrasound guided nerve blocks using three different task trainers (Table 1). The first task trainer was a Blue Phantom pediatric vascular access task trainer(CAE Healthcare products, Canada) with a cost of $599(Figure 1). This phantom includes three 5 mm nerves and a branched 6 mm vessel that bifurcates into three individual vessels. The second task trainer was a homemade gelatin phantom (Figure 2). This phantom was constructedusing Metamucil and gelatin. 250 mL of boiling water was mixed with 20 g of unflavored gelatin and 10 g of sugar free Metamucil. Vessels were constructed with thin balloons filled with water. Nerves were constructed with shoe laces running longitudinally within the gelatin structure. Total construction time was two hours and total cost of supplies was $10. The final task trainer was preformed Tofu purchased from a supermarket (Figure 3). Traditional hollow, air-filled drinking straws were inserted into the tofu to simulate vessels while uncooked spaghetti was inserted into the tofu to simulate nerves.Total construction time was 15 minutes and total cost was approximately $3.
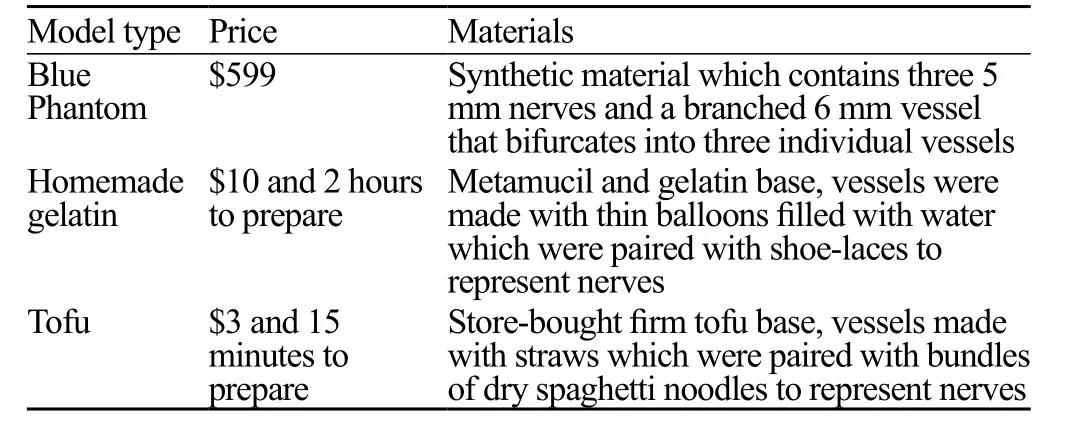
Table 1. Three models listed with price and description of materials

Figure 1. Ultrasound image showing the Blue Phantom model with simulated vascular structure and surrounding nerves.

Figure 2. Ultrasound image showing the homemade gelatin model with simulated vascular structure at left side of image and nerve on right side of image.
After performing ultrasound guided nerve blocks using all three task trainers (homemade gelatin,homemade tofu, and a commercial Blue Phantom task trainer), study participants were asked to assess the "realism" of the task trainers. Participants were randomly assigned to each station but ultimately completed all three stations. Each participant had 15 minutes per station to practice nerve blocks. We gave all participants a numbered questionnaire and asked them to give a numerical score between 1 and 5 for the following categories: realism, durability, cleanliness and preference. After obtaining the scores for each participant, a cost sheet was given to all participants detailing the cost of each trainer. Next, preferences were again recorded after cost of each model was revealed.The participants were blinded to the scores of other participants. A score of 1 was deemed least preferred,a score of 3 was deemed adequate and a score of 5 was deemed most preferred.

Figure 3. Ultrasound image showing the Tofu model with simulated vascular structure at left side of image and nerve on right side of image.
Data is described using descriptive statistics. In order to compare three groups of non-parametric ordinal data with regards to their potential differences, a Friedman test was performed. The Friedman test was applied for all sets of paired data as there were responses in all categories for all participants in all task trainer groups.We analyzed the data using Stata SE (Version 13.1,StataCorp, College Station, Tx) statistical software.
RESULTS
We enrolled a total of 25 participants into the study.Twenty-three (92%) of the participants reported prior ultrasound experience prior to participating in the tutorial session. The Blue Phantom model was favored in regard to realism, durability and cleanliness, with scores of 3.64(P<0.02), 4.52 (P<0.01) and 4.8 (P<0.01), respectively(Table 2). Prior to revealing the cost of the task trainers,the Blue Phantom and homemade gelatin models were both preferred equally by 40% (n=10) of participants,while the tofu trainer was only preferred by 20% (n=5)of participants (P<0.02). After revealing the cost of each trainer, the homemade gelatin trainer was preferred by the majority with a 72% (n=18) preference, next was the Blue Phantom with a 20% (n=5) preference and least the tofu model with an 8% (n=2) preference (P<0.01) (Figure 4).
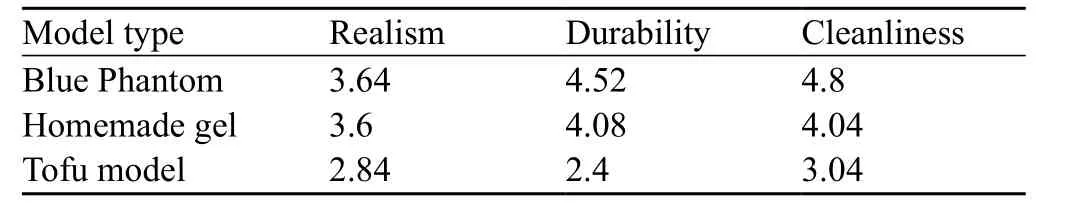
Table 2. Three models, scores for realism, durability and cleanliness

Figure 4. Participant self-reported preferences prior to and following cost considerations.
DISCUSSION
Our study aimed to evaluate participant preference for three different task trainers used for ultrasound guided anesthetic nerve block training. Based on our data, prior to cost considerations, the Blue Phantom model was identified to have the highest fidelity and was preferred equally to the homemade gelatin model. This concept has been validated in previous studies.[11–14]However, when cost was considered, most demonstrated a preference for the homemade gelatin model. This suggests that a less expensive, homemade version of the task trainer may be a reasonable alternative to a commercial device.As ultrasound use is becoming increasingly pervasive across multiple specialties it is essential that providers acquire the skills and competency to effectively use this technology. Decreased training costs allow for reallocation of resources and increased availability,especially in non-traditional settings. Low cost models are already being utilized in settings where commercial models are not readily available or affordable.[15]
Based on our data, each model had various advantages and disadvantages. While the Blue Phantom is highly durable, self-healing, realistic, requires least amount of preparation time and has the longest shelf life of all the models tested, at $599 it is significantly more expensive than the other models.[16]Furthermore,the Blue Phantom design does provide realistic, tactile feedback and very low background echogenicity,however, there was concern that exaggerated needle visibility does not translate into clinical practice. Other drawbacks include the inability to change structures within the model.[17]
In contrast, the homemade tofu was the least expensive model tested and was advantageous over the homemade gelatin in preparation time. It requires minimal time to create while utilizing common and cheap ingredients; this study used spaghetti to represent the nerves and straws to simulate arteries. Setup includes placement of the"structures" through the tofu and the model is immediately ready to scan. The tactile feedback and resistance of the "tissue" was less realistic as compared to the other phantoms, but there was appropriate needle visibility.However, participants found this model to be less clean and realistic when compared to either the Blue Phantom or homemade gelatin model.
With the Homemade gelatin phantom, a major advantage includes the cost, being about $10 in total for all the necessary supplies. However, there is a significant time investment in obtaining the materials and creating the phantom (approximately 1–2 hours).[18]This model is appropriate for repeated use because it can be frozen and re-used. It has been demonstrated that cycles of heating and re-setting allows for the gelatin model to "heal"thus preventing needle tract artifact.[18,19]However, this model only lasts 2–3 weeks even when antiseptic agents are incorporated during construction.[17]Though it is less durable than blue phantom, the needle visibility is objectively more indicative to what is seen in clinical practice. Structures can be placed in the gelatin to increase or decrease the difficulty of correct needle placement.[19]To combat low background echogenicity and over-visualization of the needle, adding millet flour to homemade gelatin models increasing echogenicity.[15,17,18]
Overall, there are several considerations when determining which task trainer is best used for training.Realism, image quality, tactile feel, cleanliness and durability are all factors in determining which model is best.Ultimately, these factors along with cost consideration can be used to determine which model can be used for specific training. Our data indicates that homemade models can provide similar fidelity at a lower cost but may require preparation, have decreased life span and be messier. Future,large scale studies are required to determine the durability and effectiveness of skill acquisition for each model.
LIMITATIONS
There were several limitations to this study. First, this was a single center study with a small sample size. Given the small number of participants, our results may not be generalizable. Additionally, the metrics were based on participant opinion as opposed to objective findings.
There is also concern for selection bias given the participants (medical students) included in this study.Furthermore, participants were not grouped based on previous experience with ultrasound or ultrasound models. Additionally, no attempt was made to assess the effectiveness of training or the durability of models. Future studies are needed to determine if the use of higher fidelity models can translate into improved success and if more advanced users can relate these models to human patients.
CONCLUSION
Participants identified the commercially available Blue Phantom model to have the highest fidelity;however, after factoring in device cost, there was a preference for the homemade gelatin model. Further large scale studies are required to determine which model is best for teaching ultrasound guided nerve blocks.
Funding: None.
Ethical approval: The study was approved by our institutional review board (IRB).
Conflicts of interest: Dr. J Christian Fox does have a disclosure which includes Sonosim stock for consulting. However, no Sonosim products were used for study purposes. There are no copyright infringement or third party data used. Any information from previous articles are cited appropriately.
Contributors: Lahham S led the design of the study and data collection, and drafted the manuscript. All authors contributed to the interpretation of the results and the critical revision of the manuscript.
1 Kosnik J, Shamsa F, Raphael E, Huang R, Malachias Z,Georgiadis GM. Anesthetic methods for reduction of acute shoulder dislocations: a prospective randomized study comparing intraarticular lidocaine with intravenous analgesia and sedation.Am J Emerg Med. 1999;17(6):566–70.
2 De Buck F, Devroe S, Missant C, Van de Velde M. Regional anesthesia outside the operating room: indications and techniques. Curr Opin Anaesthesiol. 2012;25(4):501–7.
3 Herring A, Price DD, Nagdev A, Simon B. Superior cluneal nerve block for treatment of buttock abscesses in the emergency department. J Emerg Med. 2010;39(1):83–5.
4 Norman A, Judkins K. Pain in the patient with burns. Contin Educ Anaesth Crit Care Pain. 2004;4 (2): 57–61.
5 Shank ES, Martyn JA, Donelan MB, Perrone A, Firth PG,Driscoll DN. Ultrasound-guided regional anesthesia for pediatric burn reconstructive surgery: A prospective study. J Burn Care Res. 2016;37(3):e213–7.
6 Bellolio MF, Gilani WI, Barrionuevo P, Murad MH, Erwin PJ, Anderson JR, et al. Incidence of adverse events in adults undergoing procedural sedation in the emergency department:a systematic review and Meta-analysis. Acad Emerg Med.2016;23(2):119–34.
7 Neal JM, Barrington MJ, Brull R, Hadzic A, Hebl JR, Horlocker TT, et al. The Second ASRA Practice Advisory on Neurologic Complications Associated With Regional Anesthesia and Pain Medicine: Executive Summary 2015. Reg Anesth Pain Med.2015;40(5): 401–30.
8 Hatch N, Wu TS, Barr L, Roque PJ. Advanced ultrasound procedures. Crit Care Clin. 2014;30(2):305–29.
9 McGaghie WC, Draycott TJ, Dunn WF, Lopez CM, Stefanidis D. Evaluating the impact of simulation on translational patient outcomes. Simul Healthc. 2011;6 Suppl:S42–7.
10 Nix CM, Margarido CB, Awad IT, Avila A, Cheung JJ,Dubrowski A, et al. A scoping review of the evidence for teaching ultrasound-guided regional anesthesia. Reg Anesth Pain Med. 2013;38(6):471–80.
11 Chantler J, Gale L, Weldon O. A reusable ultrasound phantom.Anaesthesia. 2004;59(11):1145–6.
12 Bude RO, Adler RS. An easily made, low-cost, tissue-like ultrasound phantom material. J Clin Ultrasound. 1995;23(4):271–3.
13 Wells M, Goldstein L. The polony phantom: a cost-effective aid for teaching emergency ultrasound procedures. Int J Emerg Med.2010;3(2):115–8.
14 Chao SL, Chen KC, Lin LW, Wang TL, Chong CF. Ultrasound phantoms made of gelatin covered with hydrocolloid skin dressing. J Emerg Med. 2013;45(2):240–3.
15 Cheruparambath V, Sampath S, Deshikar L, Ismail HM,Bhuvana K. A low-cost reusable phantom for ultrasound-guided subclavian vein cannulation. Indian J Crit Care Med. 2012;16(3): 163–165.
16 Blue Phantom. Regional Anesthesia Ultrasound Training Block Model. Available from: http://www.bluephantom.com/details.aspx?pid=61
17 Sultan SF, Shorten G, Iohom G. Simulators for training in ultrasound guided procedures. Med Ultrason. 2013;15(2):125–31.
18 Bude RO, Adler RS. An easily made, low-cost, tissue-like ultrasound phantom material. J Clin Ultrasound. 1995;23(4):271–3.
19 Hocking G, Hebard S, Mitchell CH. A review of the benefits and pitfalls of phantoms in ultrasound-guided regional anesthesia.Reg Anesth Pain Med. 2011;36(2):162–70.
Shadi Lahham, Email: slahham@uci.edu
BACKGROUND:Ultrasound guided regional anesthesia is widely taught using task trainer models. Commercially available models are often used; however, they can be cost prohibitive. Therefore,alternative "homemade" models with similar fidelity are often used. We hypothesize that professional task trainers will be preferred over homemade models. The purpose of this study is to determine realism,durability and cleanliness of three different task trainers for ultrasound guided nerve blocks.
METHODS:This was a prospective observational study using a convenience sample of medical student participants in an ultrasound guided nerve block training session on January 24th, 2015.Participants were asked to perform simulated nerve blocks on three different task trainers including,1 commercial and 2 homemade. A questionnaire was then given to all participants to rate their experiences both with and without the knowledge on the cost of the simulator device.
RESULTS:Data was collected from 25 participants. The Blue Phantom model was found to have the highest fidelity. Initially, 10 (40%) of the participants preferred the Blue Phantom model, while 10(40%) preferred the homemade gelatin model and 5 (20%) preferred the homemade tofu model. After cost awareness, the majority, 18 (72%) preferred the gelatin model.
CONCLUSION:The Blue Phantom model was thought to have the highest fidelity, but after cost consideration the homemade gelatin model was preferred.
World J Emerg Med 2017;8(4):287–291
10.5847/wjem.j.1920–8642.2017.04.007
November 26, 2016
Accepted after revision May 23, 2017
 World journal of emergency medicine2017年4期
World journal of emergency medicine2017年4期
- World journal of emergency medicine的其它文章
- Evaluation of a point of care ultrasound curriculum for Indonesian physicians taught by first-year medical students
- Instructions for Authors
- Evaluation of modified Alvarado scoring system and RIPASA scoring system as diagnostic tools of acute appendicitis
- Education in cardiopulmonary resuscitation in Russia:A systematic review of the available evidence
- Rehabilitation of vulnerable groups in emergencies and disasters: A systematic review
- Paediatric-appropriate facilities in emergency departments of community hospitals in Ontario:A cross-sectional study
