Ankle-brachial index and brachial-ankle pulse wave velocity are risk factors for ischemic stroke in patients with type 2 diabetes
Ting Li, Xiu-juan Wu, Xiao-min Chen, Si-bo Wang, Kang-ding Liu, Ying-qi Xing
Neuroscience Center, Department of Neurology, the First Hospital of Jilin University, Changchun, Jilin Province, China
How to cite this article:Li T, Wu XJ, Chen XM, Wang SB, Liu KD, Xing YQ (2017) Ankle-brachial index and brachial-ankle pulse wave velocity are risk factors for ischemic stroke in patients with type 2 diabetes. Neural Regen Res 12(11):1853-1859.
Introduction
Major improvements in primary prevention and acute treatment have led to a decline in global stroke incidence.However, rates observed in young adults are on the rise(Kissela et al., 2012; Aigner et al., 2017), signaling a need for improved preventative strategies. In addition, as the global population ages, the absolute number of strokes is expected to dramatically increase in coming years: by 2025, 1.5 million European people will suffer a stroke each year (Béjot et al., 2016). Diabetes mellitus is one of the main risk factors for ischemic stroke. With the recent increase in incidence of diabetes mellitus, the prevention of ischemic stroke among diabetes patients is an increasingly important public health concern (Pan et al., 2016).
The ankle-brachial index (ABI) is calculated separately for each foot by dividing the higher of the two systolic pressures in the ankle by the higher of the two systolic pressures in the arm (Wang et al., 2008; Gómez-Marcos et al., 2012).It is a standard measure of arterial blood flow in the lower extremities and the non-invasive gold standard for detecting peripheral artery disease (Aboyans et al., 2012). Low ABI is associated with an increased risk of incident coronary events,stroke, and mortality in the general population (Fowkes et al.,2008; Diehm et al., 2009). The brachial-ankle pulse wave velocity (BaPWV), expressed in meters per second, is calculated as the ratio of the distance travelled and the arm-to-foot time delay between pulse waves (Gómez-Marcos et al., 2012). The BaPWV can be used to assess arterial stiffness, and to predict and detect cardiovascular disease (Lee, 2015; Munakata, 2016;Murakami et al., 2017). In recent years, ABI and BaPWV have been used to predict ischemic heart disease and cerebrovascular disease (Chung et al., 2015; Saji et al., 2015).
ABI and BaPWV are simple, non-invasive, convenient,and quick measures that are being increasingly accepted as meaningful clinical indicators (Yamashina et al., 2002; Cortez-Cooper et al., 2003; Wang et al., 2012; Davies et al., 2014;Herráiz-Adillo et al., 2016). However, whether ABI and BaPWV can be used to predict risk in patients with type 2 diabetes is unclear. To address this, we evaluated risk of cerebrovascular disease, specifically ischemic stroke in patients with type 2 diabetesviaABI, BaPWV, head MRI, transcranial Doppler ultrasonography, and carotid ultrasound scans.
Subjects and Methods
Subjects
We recruited 117 patients with type 2 diabetes who met the WHO (1999) diagnostic criteria for diabetes mellitus and sought medical treatment between May and October 2015 at the First Hospital of Jilin University, China (WHO, 1999).
Inclusion criteria
Patients presenting with all of the following criteria were considered for study inclusion: (1) a history of type 2 diabetes mellitus; (2) no evidence of subclavian artery stenosis on carotid ultrasound scan; and (3) participation and cooperation with examinations.
Exclusion criteria
Patients with one or more of the following conditions were excluded from this study: (1) arrhythmia; (2) thrombolytic therapy; (3) arterial stent implantation or lower-limb revascularization; (4) limb-related disabilities; (5) unable to cooperate with certain tests.
The study protocol was approved by the Ethics Committee of The First Hospital of Jilin University of China (approval No. 2015-241). The study was performed in accordance with theDeclaration of Helsinki. All participants provided informed consent.
Outpatient or inpatients from the First Hospital of Jilin University of China were selected between May 1 and October 31, 2015. The general clinical data collected included sex,age, height, body weight, body mass index (BMI), hypertension, and smoking habits. Enrolled patients underwent the following blood tests under fasting conditions: glycosylated hemoglobin, fasting blood glucose, cholesterol, triglycerides,high-density lipoprotein (HDL) cholesterol, and low-density lipoprotein (LDL) cholesterol. In addition, the 117 participants underwent head MRI, transcranial Doppler ultrasonography, carotid ultrasound scans, lower extremity artery ultrasonography, ABI, and BaPWV measurements.
The diagnostic criteria for transcranial Doppler ultrasonography and carotid ultrasound scans were from the Ultrasound Guide for Vessels and Superficial Organs (Chinese medical doctor association). The ABI measures included ABI value,upper extremity upside time (UT), lower extremity UT, upper limb systolic blood pressure, lower limb systolic blood pressure, upper limb diastolic blood pressure, lower limb diastolic blood pressure, upper extremity mean pressure, lower extremity mean pressure, upper limb pulse pressure, and lower limb pulse pressure. According to results from the head MRI, the patients were divided into a diabetes-only group (n= 55) and a diabetes and ischemic stroke group (n= 62).
Transcranial Doppler ultrasonography and carotid ultrasound scan
We used transcranial Doppler ultrasonography (EMS-9, Delica, China, 2-MHz probe) to scan the middle cerebral artery,anterior cerebral artery, posterior cerebral artery, internal carotid artery siphon, ophthalmic artery, basilar artery, and vertebral artery. The severity of cerebrovascular stenosis was measured using Sacco RL diagnostic criteria (Sacco et al.,1995). Color Doppler ultrasound scans (IU-22, Philips, the Netherlands, L9-3, C5-1 probes) were used to bilaterally scan the common carotid artery, extracranial internal carotid artery, external carotid artery, subclavian artery, and vertebral artery. The severity of each carotid artery lesion was assessed based on the diagnostic criteria outlined by the Society of Radiologists in Ultrasound Consensus Conference, 2003(Grant et al., 2003).
ABI and BaPWV measurements
We used a blood pressure and pulse monitor manufactured by Beijing Yue Qi Chuang Tong Technology Co., Ltd., China(model VBP-10S). The sphygmomanometer cuffwidth was 10 cm and the length was 25–30 cm. Participants were instructed to lie in a supine position on the examination table.The four cuffs were placed on the brachial arteries of the upper limbs and the posterior tibial arteries of the lower limbs.Once the participants assumed the standard supine position,they maintained a completely relaxed state for 5 minutes.The blood pressure and pulse monitor then automatically and simultaneously measured arterial blood pressure in the limbs (Forbang et al., 2014; Cheng et al., 2016). As shown inFigure 1, BaPWV, which was expressed in meters per second, was calculated as the ratio of the distance travelled and the arm-to-foot time delay between the pulse waves (Mc-Dermott et al., 2002). Experienced technicians took all ABI and BaPWV readings.
Statistical analysis
We used SPSS version 17.0 software (IBM, West Grove, PA,USA) for statistical analysis. We compared the count data between groups using a chi-square test. If the measurement data had a normal distribution, we used the mean ± SD to describe the quantitative data. We used a two independent samplet-test to compare the quantitative data between groups. If the data did not obey a normal distribution, we used the Wilcoxon rank-sum test. We used multivariate logistic regression to analyze the risk factors of ischemic stroke among patients with diabetes. AP-value less than 0.05 was considered statistically significant.

Figure 1 Monitoring model images of normal and abnormal bilateral ABI values.Abscissa: UT; ordinate: amplitude. UT: Upside time; ABI: ankle-brachial index.

Figure 2 Trial flow chart.

Figure 3 Magnetic resonance imaging (MRI) images of a 59-year-old male patient with diabetes without ischemic stroke.The patient presented a headache for half a year. Head MRI: normal. MRI showed normal signal in the T1-weighted image (T1WI),T2-weighted image (T2WI), and Flair image.
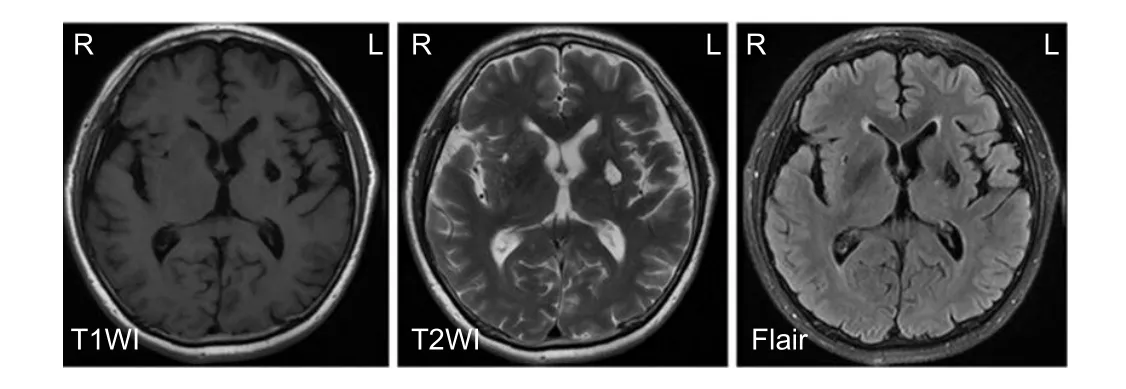
Figure 4 Magnetic resonance imaging (MRI) images of a 62-year-old male patient with diabetes and ischemic stroke.The patient presented body paralysis on the right side for 1 day. Head MRI: Cerebral infarction on the right side of the basal ganglia. MRI showed low signal in the T1-weighted image (T1WI), high signal in the T2-weighted image (T2WI), and low signal in the Flair image on the right side of the basal ganglia.
Results
Characteristics of the participants
We recruited 117 patients (77 males and 40 females) with an average age of 59.75 years (range, 39–84). Patients were separated into a diabetes-only group or a diabetes and ischemic stroke group based on whether cerebral infarction lesions were detected on the head MRI (Figure 2). In the diabetes-only group, there were 55 participants (33 males and 22 females) aged 39 to 77 years old, with a mean age of 58.07± 9.49 and a BMI of 26.02 ± 3.04 (Figures 3and4). In the group of patients with diabetes and ischemic stroke, there were 62 participants (44 males and 18 females) aged 43 to 84 years old, with a mean age of 61.32 ± 9.52 and a BMI of 25.48 ± 2.93.
The diabetes-only group and diabetes and ischemic stroke group were not significantly different in terms of the male/female ratio (P> 0.05), height (P= 0.455), body weight (P=0.739), BMI (P= 0.328), history of hypertension (P> 0.05),or smoking habits (P> 0.05). Similarly, levels of glycated hemoglobin, fasting blood glucose, cholesterol, triglycerides,LDL cholesterol, HDL cholesterol, and triglycerides were not significantly different between the two groups (P> 0.05).The transcranial Doppler ultrasound and carotid ultrasound revealed no significant differences between the two groups (P> 0.05) (Table 1).
Comparison of ABI and BaPWV between the two groupsDifferences in BaPWV, ABI, upper extremity UT, lower extremity UT, upper limb systolic pressure, upper limb mean pressure, and upper limb pulse pressure were statistically significant (P< 0.05) between the two groups. To exclude confounding factors and assess the possibilities with respect to clinical application, we selected the BaPWV and ABI for a multivariate logistic regression analysis. The results indicated that BaPWV and ABI were independent risk factors for the incidence of ischemic stroke among the patients with type 2 diabetes mellitus (Tables 2and3).
Discussion
We found that the ABI and BaPWV measures were independent predictors of ischemic stroke in our patient group.Specifically, a higher BaPWV and lower ABI were associated with an increased risk of ischemic stroke.
The concept of ABI was first proposed in 1950 by Winsor,and has been widely used in clinical and epidemiological studies of lower extremity arterial disease. Many related national and international research studies have demonstrated that ABI is an independent risk factor for atherosclerotic heart disease.Therefore, ABI monitoring has an important role in preventing coronary atherosclerotic heart disease. In addition, low ABI values and elevated serum creatinine may predict chronic kidney disease (O’Hare et al., 2005; Vinuesa et al., 2005).
The relationship between ABI values and ischemic stroke has gradually received more attention in recent years. In 2001, Tsai AW et al. conducted a large-scale study of 14,839 patients over a period of 7 years, as a component of the Atherosclerosis Risks in Communities study (Tsai et al., 2001).Murabito et al. (2003) studied 674 patients over a 4-year period. Both studies found that a reduction in ABI values was correlated with increased ischemic stroke. These studies were preliminary; however, they did confirm the association between ABI values and ischemic stroke.
Nakano et al. (2004) compared ABI values in patients with ischemic stroke and healthy controls. They found that low ABI may be a risk factor for ischemia. Ovbiaqele et al. (2009)found that low ABI values predicted ischemic stroke. Both of these studies support the association between low ABI and ischemic stroke. Gronewold et al. (2014) found that among the general population, ABI appears to be a strong predictor of stroke, specifically for patients with classical risk factors.In addition, low ABI values appear to be associated with a higher risk of early recurrent stroke in patients with acute cerebral ischemia and no history of symptomatic peripheral arterial disease (Tsivgoulis et al., 2012). Moreover, Ratanakorn et al. (2012) conducted a study of 747 patients with ischemic stroke or transient ischemic attack. TOAST classification results demonstrated that ABI values significantly differed between patients with diverse characteristics. Chung et al. (2013) reported the same finding.
Subsequent studies have found that ABI values and symptoms of neurological impairment are correlated in patients with stroke such that lower ABI values are associated with greater severity of neurological impairment (Chotik-anuchit et al., 2011; Kim et al., 2012, 2014). Therefore, these studies support an association between ABI values and ischemic stroke. Ishizuka et al. (2014) continued this research by demonstrating that ABI values < 0.9 were a predictive indicator of neurological impairment in patients with acute ischemic stroke, and that ABI values < 1.0 predicted ischemic cerebrovascular disease. Alvarez-Sabin et al. (2014) studied 977 patients with ischemic stroke and found that among patients with non-cardiac ischemic stroke, a low ABI was an independent risk predictor for cerebrovascular disease and neurological impairment. Gronewold et al. (2014) conducteda screening analysis of 4,299 participants. They found that ABI values independently predicted stroke in the general population, particularly when combined with other stroke risk factors.

Table 1 General participant characteristics
Park et al. (2009) demonstrated that increased BaPWV values are associated with the degree of cerebral arterial calcification in patients with acute ischemic stroke. In addition, Hong et al. (2016) concluded that low ABI values are independent predictors of ischemic and recurrent strokes.Furthermore, low ABI values represent supplemental information regarding patients who are at increased risk of subsequent strokes. Fan et al. (2013) and Xuan et al. (2015) found that both BaPWV and ABI were suitable and complementary tools to accompany transcranial Doppler ultrasonography in the early diagnosis of intracranial arterial stenosis/occlusion in patients with acute ischemic stroke. In addition, Saji et al.(2015) studied 1,380 patients with acute ischemic stroke and found that high BaPWV and low ABI values were predictive of acute ischemic stroke. Severe cerebral arterial disease and a high incidence of subsequent vascular events have been associated with ABI values < 0.8 in patients with ischemic stroke; however, this association was not present for patients with mild ABI values (0.8–0.89) (Manzano et al., 2012). Furthermore, Tziomalos et al. (2014) demonstrated that there is no relationship between ABI values ≤ 0.90 or > 1.40 and increased stroke severity or worse in-hospital outcomes in patients with acute ischemic stroke.
A number of studies have found that ABI values in patients with diabetes predict clinical symptoms (Bouchi et al., 2012; Hoshino et al., 2013). In addition, the incidence of ischemic stroke is approximately 23–53% higher in patients with diabetes compared with patients with ischemic stroke without diabetes (Fonville et al., 2014). Chang et al. (2014)found that the rates of composite events and mortality from all causes were significantly higher in patients with diabetes,low ABIs, and high BaPWVs compared with those with low ABI and low BaPWV levels.
The present study builds upon existing Chinese and foreign studies on the relationship between ABI values, BaPWVs, and ischemic stroke by investigating the relationships between ABI, BaPWV, and ischemic stroke in patients with type 2 diabetes while controlling for intracranial and extracranial vascular conditions. The results demonstrate that BaPWV and ABI are independent predictors of ischemic stroke in patients with type 2 diabetes.
We observed statistically significant differences in BaPWV,ABI, upper extremity UT, upper limb systolic blood pressure,upper limb mean pressure, and upper and lower limb pulse pressure between the diabetes-only group and the diabetes and ischemic stroke group. Multivariate logistic regression analysis demonstrated that BaPWV and ABI were independent risk factors for ischemic stroke in patients with type 2 diabetes. Our results were with consistent with those from both Chinese and international studies.
ABI measurement is simple, convenient, and rapid, and has therefore been used to diagnose peripheral arterial disease. ABI is increasingly being used to detect chronic kidney disease, screen for cardiovascular disease, and prevent ischemic stroke in clinical practice. Use of ABI as a diagnostic tool may enable prevention and early treatment of cardiovascular and cerebrovascular diseases.
Compared with similar studies conducted within and out-side of China, we collected data regarding a large number of variables including clinical data, ABI, BaPWV, and head MRI, which contributes to the diagnosis of cerebral infarction. We then used transcranial Doppler ultrasound and carotid ultrasound to further clarify cerebrovascular changes.We found no differences in clinical data or cerebrovascular condition between the two groups. We thus determined that BaPWV and ABI are independent predictors in patients with type 2 diabetes and ischemic stroke.

Table 3 Results of Logistic regression analysis
There are two major limitations of this study. First, the sample size of this study was relatively small. A large-scale study is required to further confirm our conclusions. Second, we did not compare the diagnostic efficacy of ABI and BaPWV with that of other tests (e.g. computed tomography angiography and digital subtraction angiography) for both lower limb arteries.
In summary, BaPWV and ABI appear to be independent predictors of ischemic stroke in patients with type 2 diabetes and may be useful clinical tools in a variety of clinical settings.
Author contributions:TL, YQX, and KDL designed the study. TL,XMC, and SBW performed experiments and analyzed data. TL and XJW wrote the paper. All aurthors approved the final version of this paper.
Conflicts of interest:None declared.
Research ethics:The study protocol was approved by the Ethics Committee of the First Hospital of Jilin University (approval No. 2015-241). The study followed the Declaration of Helsinki and relevant ethical principles.Patients and/or their family members volunteered to participate in the study. All patients (or guardians) provided written informed consent for publication of associated data and accompanying images.
Declaration of patient consent:The authors certify that they have obtained all appropriate patient consent forms. In the form, the patients have given their consent for their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Data sharing statement:Datasets analyzed during the current study are available from the corresponding author on reasonable request.
Plagiarism check:Checked twice by iThenticate.
Peer review:Externally peer reviewed.
Open access statement:This is an open access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under identical terms.
Open peer review reports:
Reviewer 1:Shan Ping Yu, Emory University School of Medicine Anesthesiology, USA.
Comments to authors:The paper reports a clinical study to evaluate the relationship between ABI, BaPWV values and the incidence of ischemic stroke among patients with type 2 diabetes. The study confirmed that the ABI value in the diabetic stroke patients was significantly lower than that of the diabetes-only group. The BaPWV in diabetic stroke patients was significantly higher than that of the diabetes-only group. The paper is well written and the study was reasonably designed and executed. The statistical method appears appropriate for the data collected in this study. Please see additional file for more details.
Additional file:Open peer review report 1.
Reviewer 2:Jigar Pravinchandra Modi, Complex Systems and brain sciences, Florida Atlantic University, USA.
Comments to authors:This is an interesting paper that accurately dissects a role of the ankle-brachial index and brachial-ankle pulse wavevelocity as predictors for ischemic stroke. The data support the hypothesis;however, as authors mentioned about MRI results that he uses to determine and divide patients into groups. Authors must provide some figures to represent ischemic stroke for readers. As mentioned in Similar paper Xuan et al. 2015, authors provide sensitivity and specificity data on ABI and BaPWV which help to distinguish between stroke patients with type 2 diabetes and type 2 diabetes patients only. Authors should comment on below paper in Discussion. Chang et al. 2014 “The combination of the ankle brachial index and brachial ankle pulse wave velocity exhibits a supe-rior association with outcomes in diabetic patients”. Please see additional file for more details.
Additional file:Open peer review report 2.
Aboyans V, Criqui MH, Abraham P, Allison MA, Creager MA, Diehm C,Fowkes FGR, Hiatt WR, Jönsson B, Lacroix P, Marin B, McDermott MM, Norgren L, Pande RL, Preux PM, Stoffers HE, Treat-Jacobson D(2012) Measurement and interpretation of the ankle-brachial index:a scientific statement from the American Heart Association. Circulation 126:2890-2909.
Aigner A, Grittner U, Rolfs A, Norrving B, Siegerink B, Busch MA(2017) Contribution of established stroke risk factors to the burden of stroke in young adults. Stroke doi: 10.1161/STROKEAHA.117.016599.
Alvarez-Sabín J, Quintana M, Santamarina E, Maisterraa O, Gil-Nu A(2014) Low ankle-brachial index predicts new vascular events and functional outcome after 1 year in patients with non-cardioembolic stroke: our experience and review. Eur J Neurol 21:100-106.
Béjot Y, Bailly H, Durier J, Giroud M (2016) Epidemiology of stroke in europe and trends for the 21st century. Presse Med 45:391-398.
Bouchi R, Babazono T, Takagi M ,Yoshida N, Nyumura I, Toya K, Hanai K, Tanaka N, Uchigata Y (2012) Non-linear association between ankle-brachial pressure index and prevalence of silent cerebral infarction in Japanese patients with type 2 diabetes. Atherosclerosis 222:490-494.
Chang LH, Lin HD, Kwok CF, Won JG, Chen HS, Chu CH, Hwu CM,Kuo CS, Jap TS, Shih KC, Lin LY (2014) The combination of the ankle brachial index and brachial ankle pulse wave velocity exhibits a superior association with outcomes in diabetic patients. Intern Med 53:2425-2431.
Cheng YB, Li Y, Sheng CS, Huang QF, Wang JG (2016) Quantification of the interrelationship between brachial-ankle and carotid-femoral pulse wave velocity in a workplace population. Pulse (Basel) 3:253–262.
Ultrasound Branch of the Chinese Medical Doctor Association (2011)Guidelines for vascular and superficial organ ultrasound examination. Beijing: People’s Military Doctor Press.
Chotik-anuchit S, Nilanont Y, Poungvarin N (2011) Relationship between ankle brachial index (ABI), high sensitivity C-reactive protein(hs-CRP) and initial disability level in acute ischemic stroke. J Med Assoc Thai 94:S94-98.
Chung CM, Tseng YH, Lin YS, Hsu JT, Wang PC (2015) Association of brachial-ankle pulse wave velocity with atherosclerosis and presence of coronary artery disease in older patients. Clin Interv Aging 10:1369-1375.
Chung PW, Kim DH, Kim HY, Park KY, Park TH, Hong JM, Kim GM,Bang OY, Oh K, Lee SJ (2013) Differences of ankle-brachial index according to ischemic stroke subtypes: the peripheral artery disease in Korean patients with ischemic stroke (PIPE) study. Eur Neurol 69:179-184.
Collaboration ABI, Fowkes FG, Murray GD, Butcher I, Heald CL, Lee RJ, Chambless LE, Folsom AR, Hirsch AT, Dramaix M, deBacker G,Wautrecht JC, Kornitzer M, Newman AB, Cushman M, Sutton-Tyrrell K, Fowkes FG, Lee AJ, Price JF, d’Agostino RB, et al. (2008) Ankle brachial index combined with Framingham Risk Score to predict cardiovascular events and mortality: a meta-analysis. JAMA 300:197-208.
Cortez-Cooper MY, Supak JA, Tanaka H (2003) A new device for automatic measurements of arterial stiffness and ankle-brachial index.Am J Cardiol 91:1519-1522.
Davies JH, Kenkre J, Williams EM (2014) Current utility of the ankle-brachial index (ABI) in general practice: implications for its use in cardiovascular disease screening. BMC Family Practice 15:69.
Diehm C, Allenberg JR, Pittrow D, Mahn M, Tepohl G, Haberl RL,Darius H, Burghaus I, Trampisch HJ (2009) Mortality and vascular morbidity in older adults with asymptomatic versus symptomatic peripheral artery disease. Circulation 120:2053-2061.
Fan H, Hub X, Yu W, Cao H, Wang J, Li J, Liu B, Yang J, Zhang Q (2013)ankle-brachial index and risk of stroke. Atherosclerosis 229:317-323.
Fonville S, Zandbergen AA, Koudstaal PJ, Hertog HM (2014) Prediabetes in patients with stroke or transient ischemic attack: prevalence,risk and clinical management. Cerebrovasc Dis 37:393-400.
Forbang NI, McDermott MM, Liao Y, Ix JH, MA, MD, Liu K, Tian L,Evans N, Criqui MH (2014) Associations of diabetes mellitus and other cardiovascular disease risk factors with decline in the ankle brachial index. Vasc Med 19:465-472.
Gómez-Marcos MA, Recio-Rodríguez JI, Patino-Alonso MC, Gómez-Sánchez L, Agudo-Conde C, Gómez-Sánchez M, Rodríguez-Sánchez E, García-Ortiz L (2012) Ambulatory arterial stiffness indices and target organ damage in hypertension. BMC Cardiovasc Disord 12:1-9.
Grant EG, Benson CB, Moneta GL, Alexandrov AV, Baker JD, Bluth EI,Carroll BA, Eliasziw M, Gocke J, Hertzberg BS, Katanick S, Needleman L, Pellerito J,Polak JF, Rholl KS, Wooster DL, Zierler RE (2003)Carotid artery stenosis: gray-scale and doppler us diagnosis-society of radiologists in ultrasound consensus conference. Radiology 229:340-346.
Gronewold J, Hermann DM, Lehmann N, Kröger K, Lauterbach K, Berger K, Weimar C, Kälsch HI, Moebus S, Jöckel KH, Bauer M, Erbel R(2014) Ankle-brachial index predicts stroke in the general population in addition to classical risk factors. Atherosclerosis 233:545-550.
Herráiz-Adillo A, Martínez-Vizcaíno V, Cavero-Redondo I, Álvarez-Bueno C, Garrido-Miguel M, Notario-Pacheco B (2016) Diagnostic accuracy study of an oscillometric ankle-brachial index in peripheral arterial disease: the influence of oscillometric errors and calcified legs. PLoS One 11:11.
Hong JB, Leonards CO, Endres M, Siegerink B, Liman TG (2016) Ankle-brachial index and recurrent stroke risk: meta-analysis. Stroke 47:317-322.
Hoshino H, Itoh Y, Yamada S, Suzuki N (2013) Prevalence and clinical features of asymptomatic peripheral artery disease in Japanese stroke patients. J Stroke Cerebrovasc Dis 22:255-259.
Ishizuka K, Hoshino T, Uchiyama S (2014) Ankle-brachial index and neurologic deterioration in acute ischemic stroke. J Stroke Cerebrovasc Dis 23:2506-2510.
Kim J, Lee DH, Cha MJ, Song TJ, Park JH, Lee HS, Nam CM, Nam HS,Kim YD, Heo JH (2012) Low ankle-brachial index is an independent predictor of poor functional outcome in acute cerebral infarction.Atherosclerosis 224:113-117.
Kim J, Song TJ, Kim EH, Lee KJ, Lee HS, Nam CM, Song D, Nam HS,Kim YD, Heo JH (2014) Brachial-ankle pulse wave velocity for predicting functional outcome in acute stroke. Stroke 45:2305-2310.
Kissela BM, Khoury JC, Alwell K, Moomaw CJ, Woo D, Adeoye O, Flaherty ML, Khatri P, Ferioli S, DeLosRiosLaRosaF, BroderickJP, Kleindorfer DO (2012) Age at stroke: temporal trends in stroke incidence in a large, biracial population. Neurology 79:1781-1787.
Lee JY, Ryu S, Lee SH, Kim BJ, Kim BS, Kang JH, Cheong ES, Kim JY,Park JB, Sung KC (2015) Association between brachial-ankle pulse wave velocity and progression of coronary artery calcium: a prospective cohort study. Cardiovasc Diabetol 14:147.
Manzano JJ, Silva DA, Pascual JL, Chang HM, Wong MC, Chen CP(2012) Associations of ankle-brachial index (ABI) with cerebral arterial disease and vascular events following ischemic stroke. Atherosclerosis 223:219-222.
McDermott MM, Greenland P, Liu K, Guralnik JM, Celic L, Criqui MH, Chan C, Martin GJ, Schneider J, Pearce WH, Taylor LM, Clark E (2002) The ankle brachial index is associated with leg function and physical activity: the walking and leg circulation study. Ann Intern Med 136:873-883.
Munakata M (2016) Brachial-ankle pulse wave velocity: background,method, and clinical evidence. Pulse (Basel) 3:195-204.
Murabito JM, Evans JC, Larson MG, Nieto K, Levy D, Wilsom PW(2003) The ankle-brachial index in the elderly and risk of stroke, coronary disease, and death: the framingham study. Arch Intern Med 163:1939-1942.
Murakami T, Nakamura H, Nishida T, Ozaki T, Asai K, Kidani T,Kadono Y, Sakaguchi M, Yoshimine T, Kishima H (2017) Brachial-ankle pulse wave velocity as a predictor of silent cerebral embolism after carotid artery stenting. J Stroke Cerebrovas Dis doi:10.1016/j.jstrokecerebrovasdis.2017.05.021.
Nakano T, Ohkuma H, Suzuki S (2004) Measurement of ankle brachial index for assessment of atherosclerosis in patients with stroke. Cerebrovasc Dis 17:212-217.
O’Hare AM, Rodriguez RA, Bacchetti P (2005) Low ankle-brachial index associated with rise in creatinine level over time: results from the atherosclerosis risk in communities study. Arch Intern Med165:1481-1485.
Ovbiagele B (2009) Association of ankle-brachial index level with stroke. J Neurol Sci 276:14-17.
Pan Y, Jing J, Li H, Wang Y, Wang Y, He Y (2016) Abnormal glucose regulation increases stroke risk in minor ischemic stroke or TIA.Neurology 87:1551-1556.
Park KY, Kim YB, Moon HS, Suh BC, Chung PW (2009) Association between cerebral arterial calcification and brachial-ankle pulse wave velocity in patients with acute ischemic stroke. Eur Neurol 61:364-370.
Ratanakorn D, Keandoungchun J, Tegeler CH (2012) Prevalence and association between risk factors, stroke subtypes, and abnormal ankle brachial index in acute ischemic stroke. J Stroke Cerebrovasc Dis 21:498-503.
Sacco RL, Kargman DE, Gu Q, Zamanillo MC (1995) Race-ethnicity and determinants of intracranial atherosclerotic cerebral infarction.The northern manhattan stroke study. Stroke 26:14-20.
Saji N, Kimura K, Yagita Y, Kawarai T, Shimizu H, Kita Y (2015)Comparison of arteriosclerotic indicators in patients with ischemic stroke: ankle-brachial index, brachial-ankle pulse wave velocity and cardio-ankle vascular index. Hypertens Res 38:323-328.
Tsai AW, Folsom AR, Rosamond WD, Jones DW (2001) Ankle-brachial index and7-year ischemic stroke incidence: the ARIC study. Stroke 32:1721-1724.
Tsivgoulis G, Bogiatzi C, Heliopoulos I, Vadikolias K, Boutati E,Tsakaldimi S, Al-Attas OS, Charalampidis P, Piperidou C, Maltezos E, Papanas N (2012) Low Ankle-Brachial Index predicts early risk of recurrent stroke in patients with acute cerebral ischemia. Atherosclerosis 222:407-412.
Tziomalos K, Giampatzis V, Bouziana S, Pavlidis A, Spanou M, Papadopoulou M, Kagelidis G, Boutari C, Savopoulos C, Hatzitolios A(2014) Predictive value of the ankle brachial index in patients with acute ischemic stroke. Vasa 43:55-66.
Vinuesa SG, Ortega M, Martinez P, Goicoechea M, Campdera FG,Luño J (2005) Subclinical peripheral arterial disease in patients with chronic kidney disease: prevalence and related risk factors. Kidney Int Suppl 93:S44-47.
Wang JW, Zhou ZQ, Hu DY (2012) Prevalence of arterial stiffness in North China, and associations with risk factors of cardiovascular disease: a community-based study. BMC Cardiovasc Disord 12:119.
Wang XR, Pei Y, Li QM, Zhang F, Zhang LY, Wu YD, Chen YM, Zhu YQ, Zhan ZW, Shao WQ (2008) Correlation between ankle brachial index and the incidence of great blood vessel pathological changes in patients with type 2 diabetes mellitus: Evaluation using Doppler detector. Zhongguo Zuzhi Gongcheng Yanjiu 12:659-662.
World Health Organisation (1999) WHO Definition, Diagnosis and Classification of Diabetes Mellitus and its Complications.
Xuan Z, Zhou J, Yi L, Zhang Q, Li L (2015) Brachial-ankle pulse wave velocity and ankle-brachial index are complementary tools for transcranial Doppler ultrasonography in early diagnosis of intracranial arterial stenosis/occlusion in patients with acute ischemic stroke. J Neurol Sci 359:328-334.
Yamashina A, Tomiyama H, Takeda K, Tsuda H, Arai T, Hirose K, Koji Y, Hori S, Yamamoto Y (2002) Validity, reproducibility, and clinical significance of noninvasive brachial-ankle pulse wave velocity measurement. Hypertens Res 25:359-364.
- 中国神经再生研究(英文版)的其它文章
- The role of general anesthetics and the mechanisms of hippocampal and extra-hippocampal dysfunctions in the genesis of postoperative cognitive dysfunction
- Saponins from Panax japonicus attenuate age-related neuroinflammation via regulation of the mitogenactivated protein kinase and nuclear factor kappa B signaling pathways
- Taking out the garbage: cathepsin D and calcineurin in neurodegeneration
- MicroRNAs as diagnostic markers and therapeutic targets for traumatic brain injury
- Interferon regulatory factor 2 binding protein 2: a new player of the innate immune response for stroke recovery
- Endogenous retinal neural stem cell reprogramming for neuronal regeneration

