Robot-assisted gallbladder-preserving hepatectomy for treating S5 hepatoblastoma in a child:A case report and review of the literature
Di-Xiang Chen,Shan-Jie Wang,Ya-Nan Jiang,Mu-Chuan Yu,Jun-Zhen Fan,Xian-Qiang Wang
Abstract
Key words: Hepatectomy;Robotic surgery;Pediatrics;Hepatoblastoma;Case report
INTRODUCTION
Hepatoblastoma (HB) is the most common hepatic malignant tumour in children,accounting for approximately 50%-60% of primary hepatic malignant tumours in children,mostly in children under 3 years old[1].In Western countries,the incidence of hepatoblastoma is approximately 1-2/100000[2-4].In Asian children,the incidence of hepatoblastoma is higher relative to that in other countries and regions[4,5].Hepatoblastoma has a high degree of malignancy and a short postoperative survival.
The development of paediatric surgical robotic surgery in China is in its infancy,and the therapeutic effects of paediatric surgery are influenced by various factors,such as the child’s age,disease status,anatomical positions of the lesions,posture,and surgical complexity,which also enable robotic surgery to give full play to its advantages in the field of paediatric surgical treatment[12-16].
Herein,we report on the application of the Da Vinci surgical system for the treatment of a child’s 5thsegment liver tumour and the preservation of the gallbladder,with the aim to explore the feasibility of using the full robotic surgery to treat a child’s liver tumour and to summarize the application points of the technology.
CASE PRESENTATION
Chief complaints
A 3-year-old boy was admitted to the hospital for a liver mass for 20 d.
Physical examination
The abdomen was soft,without tender,rebound pain,or obvious mass.The liver and spleen were untouchable,Murphy's sign was negative,and the bowel sounds were normal.
Laboratory examinations
Alpha fetoprotein (AFP) was 339 μg/L,alanine aminotransferase was 11.9 U/L,and aspartate aminotransferase was 22.4 U/L.International normalized ratio was 0.97,and total bilirubin was 5.6 μmol/L.
Imaging examination
Ultrasonography revealed a low-echo mass measuring 46 mm × 26 mm × 58 mm in the liver right lobe.Enhanced computed tomography showed continuous enhancement of iso-low-density lesions of different sizes and nodules,unclear boundaries,no dilation of the intrahepatic bile duct,no enlargement of the gallbladder,and uniform thickness of the wall (Figure 1).
普洱市享有“南方丝绸”美誉的“茶马古道”起点,还因其独特的地理位置“一市连三国”,具有独具风情的口岸文化,在国家“一带一路”的国家战略驱动下,普洱市处于合作区域的中心节点位置,是国家桥头堡建设的“堡中堡”。
FINAL DIAGNOSIS
The preoperative diagnosis was hepatoblastoma.
TREATMENT
The preoperative examination was completed,and the robotic S5 liver tumour resection was performed.
Operation
After successful anaesthesia,urethral catheterization was performed.The anaesthesiologist placed an internal jugular vein catheter,and the Trendelenburg position was adopted,after which the lower chest was raised with a mattress.The Direct Trocar Entry method was used to puncture suprapubic area to establish the pneumoperitoneum (Figures 2 and 3).The pressure was 10 cm H2O,and a 12-mm trocar and the robot lens were inserted.On the left and right sides of the lens,the arm 1 and arm 2 trocars with a diameter of 8 mm were inserted.Arm 3 was placed in the midline of the left upper quadrant axilla.A 12-mm auxiliary hole was placed between arm 2 and the lens.The robot arm was placed at the head end.After the mechanical arm was connected and pulled,the abdominal pressure was reduced to 8 mmHg.
A 5thsegment right hepatic tumour could be seen through exploration.The tumour and gallbladder were isolated first,and the gallbladder could be completely separated from the tumour surface without obvious infiltration;therefore,the gallbladder was preserved (Figure 4).
The incisal edge was marked with an electrical hook at the junction between the tumour and normal liver tissue at approximately 1 cm,and the hepatic duodenal ligament was blocked with a urethral catheter using the Pringle method.The tumour and part of the normal liver tissue were completely resected with an ultrasonic knife along the incision,and the blood vessel was ligated with a 5-0 prolene line for haemostasis.The first hepatic portal block time was approximately 25 min.
The liver was cogulated with an argon knife to stop bleeding.A liver needle was used to suture the broken edge.An abdominal drainage tube was inserted from the right lower abdomenviaarm 2.The auxiliary hole was connected to the lens hole,and the specimen was removed (Figure 5).
The abdominal wall muscle at the trocar was sutured intermittently with 3-0 absorbable suture,the subcutaneous tissue was sutured discontinuously with 4-0 absorbable suture,and the skin was glued with bioprotein.The membranes of all incised skin were pulled tight and covered.
The operation was smooth,with 200 mL of bleeding,and the patient was returned to the ward after surgery.
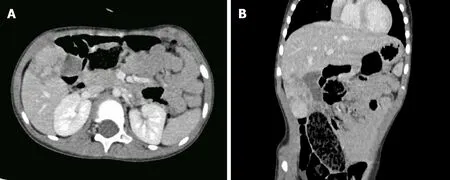
Figure 1 Contrast-enhanced computed tomography images revealing that the tumour was located in the 5th segment of the liver and was closely related to the gallbladder.
OUTCOME AND FOLLOW-UP
The operation went well.The total time was 166 min,of which the robot operation time was 115 min,and there was a blood loss of approximately 200 mL,with the provision of 300 mL of red blood cell suspension and 200 mL of plasma.The gastric tube was pulled out two days after the operation,and the patient was gradually given liquid food and semi-liquid food.Two combination antibiotics were administered for 5 d.The abdominal drainage tube was removed 6 d after the operation,and the patient was discharged 12 d after the operation.No serious complications occurred.The immunohistochemical results were as follows:hepatocytes (+),GPC-3 (+),AFP(focal +),ki-67 (+20%),Arg-1 (+),and CD99 (local) (Figure 6).The gallbladder contraction test conducted two weeks after the operation showed that the gallbladder size was approximately 5.3 cm × 2.0 cm,and the wall was not thick and smooth.Forty minutes after a meal,the gallbladder size was 5.4 cm × 1.8 cm.Ninety minutes after a meal,the gallbladder size was 2.9 cm × 1.2 cm.
DISCUSSION
Hepatoblastoma is the most common type of liver tumour for children in recent years.A number of scholars have studied the aetiology,pathogenesis,and possible course of hepatoblastoma in children from different perspectives,suggesting that it may be related to chromosomal abnormality,genetic factors,low birth weight,and various external adverse factors involving maternal exposure during pregnancy[17].According to the American paediatric oncology group,higher preoperative clinical stage is associated with worse prognosis for hepatoblastoma in children.Multiple domestic and foreign studies have shown that the survival rate of hepatoblastoma can be significantly improved by combining surgery with chemotherapy,and the complete resection of the tumour is a prerequisite for the treatment of hepatoblastoma[18,19].
The Da Vinci surgery system (Intuitive Surgical,Inc.,Mountain View,CA,USA) is the most widely used robotic system.The Da Vinci surgery robot system has a unique 3-dimensional HD magnification (10×) imaging system,and the separation process is more accurate,effectively avoiding secondary damage[20-22].The robot’s artificial wrist arm with flutter filtration function has better dexterity and a larger range than traditional laparoscopic instruments,making the anastomosis process easier and capable of more delicacy.
Over the last decade,robot-assisted laparoscopy has been included in the surgical armamentarium to manage complex abdominal scenarios,including those encountered in liver surgery[23-25].
From a technical point of view,the use of a robotic surgical system can improve certain steps of minimally invasive right liver resection.Magnified 3-dimensional vision allows for better definition of the vascular anatomy and improved recognition of the fine branches that originate from the right portal trunk and are directed toward segment 1.Furthermore,by taking advantage of the wristed instruments,it is possible to use simple ligatures to control major vessels instead of the stapler,which can be cumbersome in small spaces[26].
Characterized by its precision and minimally invasive nature,hepatobiliary and pancreatic surgery is further developed on the basis of traditional laparoscopic surgery,which expands the advantages of laparoscopic surgery[27]and the application scope of minimally invasive technology represented by laparoscopy in some fields and overcomes some deficiencies of traditional laparoscopy.It also represents the developmental direction of surgery.

Figure 2 Preoperative 3-dimensional reconstruction images.
The first report of robotic liver resection dates back to 2003,when an initial study of robotic anatomic liver resection was published by Giulianottiet al[28],10 years after the report of the first laparoscopic liver resection (LLR).Giulianottiet al[26]have proved through research that partial hepatectomy by robot offered the patient decreased abdominal wall morbidity,shorter postoperative hospital length of stay,and minimal need for blood transfusion.
Several studies have reported the efficacy and safety of robotic surgeries for various diseases,which have outcomes comparable to those of conventional or laparoscopic surgeries[22,29].Laiet al[30]compared the perioperative indicators and long-term tumour outcomes of partial hepatectomy by robot (n= 100) and laparoscopic (n= 35)methods.Compared to the laparoscopic group,the robotic group had significantly higher mass liver resection rate (27%vs2.9%) and upper posterior segment location rate (29%vs0%).The mean operative time of the robot group was longer,and there were no statistically significant differences between the two groups in blood loss,complications and mortality,R0 resection rate,5-year total survival,or 5-year diseasefree survival.
Compared with laparoscopic hepatectomy,robot-assisted surgery has shown better safety and effectiveness in the treatment of liver tumours,and the system has greatly expanded the surgical indications for hepatectomy.Regarding safety considerations,compared with LLR,robotic-assisted liver resection (RALR) has the advantages of reducing total postoperative complications,postoperative bleeding,and postoperative biliary fistula,with no significant difference in the amount of intraoperative blood loss between the two surgical methods.Regarding effectiveness,RALR improved the rate of R1 excision compared with LLR,and there were no significant differences between the two groups in terms of postoperative hospitalization time,or rate of conversion to open surgery[30-34].With improvements and upgrades of equipment and technology,the advantages of robot-assisted laparoscopic hepatectomy will become increasingly more obvious[35-37].
There are still some defects in robotic surgery.For example,the high cost of surgical robots limits the popularity of robotic surgery.Although special instruments for surgical robots have been developed,they are still not perfect,and some surgical instruments are urgently needed.The lack of a tactile feedback system with the surgical robot cannot fully play the characteristics of surgical robot.At present,training for robot operators can only be carried out in a few centres,which limits its further promotion.In addition,as robotic surgery is relatively new in the field of open surgery,its temporary high cost makes it less popular than laparoscopy,resulting in a lack of high quality,large prospective studies of robotic surgery.However,these shortcomings are improving over time.
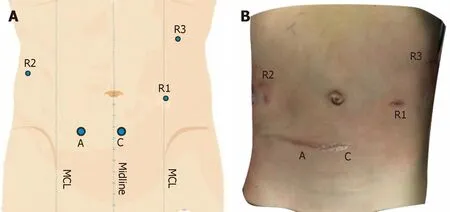
Figure 3 Schematic diagram (A) and actual picture (B) of trocar placement.
In a study by Donget al[38],the gallbladders were retained in 28 patients undergoing living donor liver transplantation (15 cases of right lobe liver and 13 cases of left lobe liver).The postoperative gallbladder function was good,and it was safe and feasible to retain the gallbladder when liver transplantation was performed.It has been proved that retaining the gallbladder can avoid post-cholecystectomy syndrome,reduce the incidence of biliary diseases,such as gallstones and Oddi sphincter dysfunction,reduce the occurrence of postoperative adipose diarrhoea,improve the quality of life of children,and reduce the incidence of possible colon cancer.
The main gallbladder changes after surgery included gallbladder enlargement and gallbladder wall thickening,and the main complications included biliary sludge,gallstone formation,and polypoid lesion of the gallbladder[39].Suet al[39]’s results demonstrated that the rate of postoperative complications of the gallbladder in donors was relative low,thus preserving the gallbladder in liver transplantation donors during liver graft procurement is feasible and safe.
CONCLUSION
For patients who are children,the complete preservation of the gallbladder and its normal function on the basis of complete tumour resection is of great significance for improving quality of life and long-term prognosis.
In summary,robot-assisted hepatectomy with gallbladder preservation is safe and feasible.Preliminary experience showed that the surgical method is clearer and more flexible than conventional endoscopy,with more accurate surgery and less resulting damage.With continued technological development and the accumulation of surgeons’ experience,robotic surgery may become a new trend in surgery.
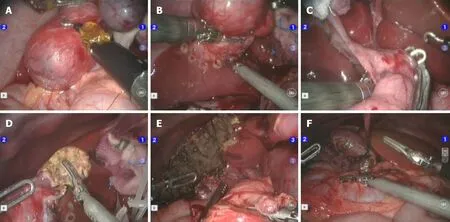
Figure 4 Surgery-related images.

Figure 5 Excised specimen.
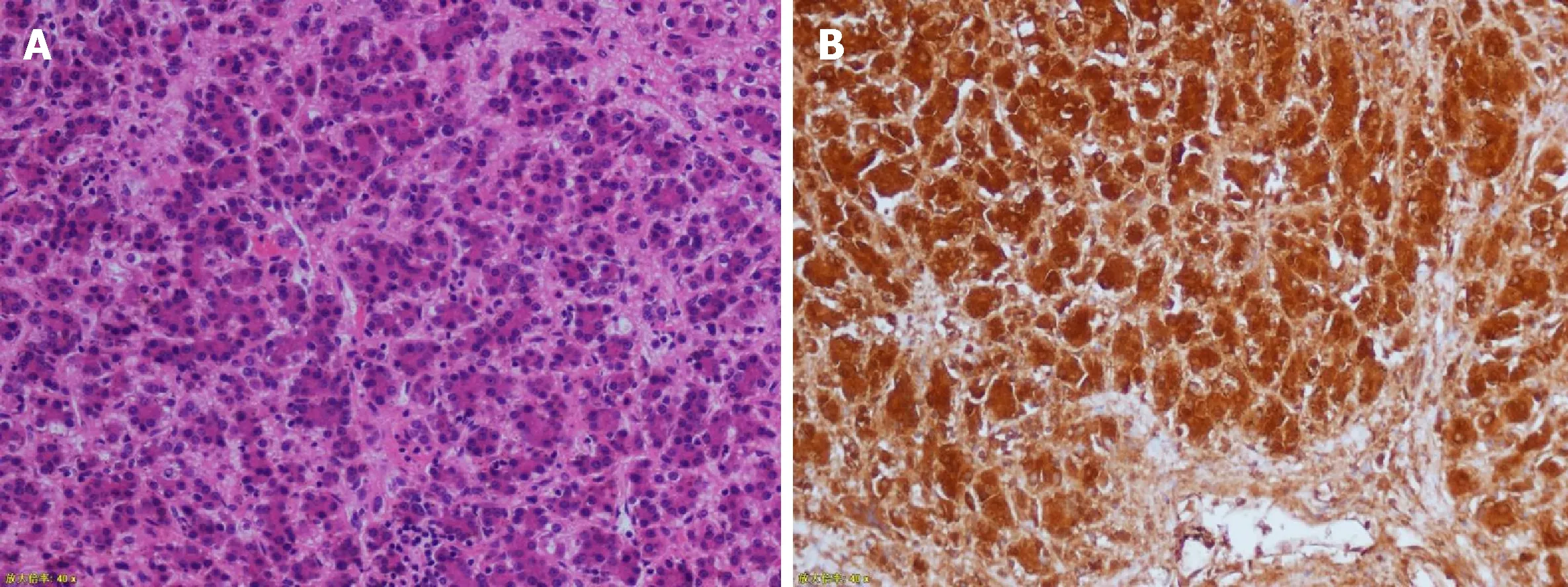
Figure 6 Pathological images (magnification 200×).
 World Journal of Clinical Cases2019年7期
World Journal of Clinical Cases2019年7期
- World Journal of Clinical Cases的其它文章
- Ultrasound imaging of abdominal sarcoidosis:State of the art
- Porphyromonas gingivalis and digestive system cancers
- Clinical evaluation of endoscopic resection for treatment of large gastric stromal tumors
- Value of superb micro-vascular imaging in predicting ischemic stroke in patients with carotid atherosclerotic plaques
- Open anterior glenohumeral dislocation with associated supraspinatus avulsion:A case report
- Vein of Galen aneurismal malformations - clinical characteristics,treatment and presentation:Three cases report
