Gastric partitioning for the treatment of malignant gastric outlet obstruction
Marcus Fernando Kodama Pertille Ramos,Leandro Cardoso Barchi,Rodrigo Jose de Oliveira,Marina Alessandra Pereira,Donato Roberto Mucerino,Ulysses Ribeiro Jr,Bruno Zilberstein,Ivan Cecconello
Abstract
Key words: Stomach neoplasms; Gastric outlet obstruction; Palliative surgery;Gastrojejunostomy; Gastric cancer
INTRODUCTION
Gastric cancer (GC) is the fifth most common cancer and third leading cause of cancer-related deaths worldwide[1].Surgical resection of the tumor with D2 lymphadenectomy is the indicated standard curative treatment[2].Unfortunately,many patients initially present with advanced disease at the time of diagnosis without the possibility of curative resection.The frequency of patients with clinical stage IV varies according to each country and may reach up to 40% of cases[3-5].
Despite the dismal prognosis,many stage IV GC patients develop complications during the course of disease that require palliative procedures.Among these complications,the following stand out: Tumor bleeding,refractory ascites,intestinal obstruction,and gastric outlet obstruction (GOO).
The incidence of GOO ranges between 5% and 14.9% in patients with distal GC.Palliative resection of the tumor is the procedure of choice in cases of resectable lesions and limited metastatic disease,and in patients with favorable clinical conditions[6].
However,many of these tumors are considered unresectable due to local invasion of adjacent structures or due to patients' unfavorable clinical conditions.Surgical bypass or endoscopic stents are options to restore the gastrointestinal continuity.Endoscopic stents are less invasive and can be deployed out of the operating room.However,concerns regarding its long-term effectiveness still grants an important role for surgery[7,8].
The most traditional surgery performed is gastrojejunostomy (GJ).The procedure is simple and can be accomplished by laparoscopy with low morbidity.However,delayed gastric emptying (DGE) is one of the main postoperative complications,with an incidence that varies between 10% and 26%[9].
In this context,gastric partitioning (GP) associated with GJ,also known as GP,has been considered an option for the treatment of malignant GOO.Initially,it was described in 1925 for complex gastroduodenal ulcers[10].Currently,is considered a palliative surgery for GOO by the Japanese Gastric Cancer Association guidelines[2].
Our institution has used GP for the past 10 years in such cases.Therefore,the aim of this study was to compare the outcomes of patients who underwent GP and GJ for malignant GOO.
MATERIALS AND METHODS
Patients
A retrospective review of all gastric adenocarcinoma patients who underwent any palliative surgical bypass from 2009 to 2018 was performed from a prospectively collected database.
Inclusion criteria were: Irresectable distal gastric tumor; the presence of obstructive symptoms; and life expectancy superior to 2 mo.Patients with proximal gastric tumors,tumors amenable to palliative resection and associated with small bowel obstruction were excluded.
Clinicopathological characteristics were evaluated as well as laboratory tests to assess nutritional status.Karnofsky performance score (KPS) and Eastern Cooperative Oncology Group (ECOG) scale were used to assign performance status.Tumor spread was evaluated by the presence of distant metastasis and carcinomatosis.Obstructive symptoms were graded according to the GOO score (GOOS) as follows: 0 = no oral intake,1 = liquids only,2 = soft solids,3 = low residue or full diet[11].Patient's weight in kilograms and body mass index (BMI) were measured prior to surgery and after 30 and 90 d.Maximum weight after surgery and last weight recorded before death were also evaluated.
Postoperative complications were graded according to Clavien-Dindo's classification[12].Major complications were considered Clavien III-IV-V.Surgical mortality was defined as death within 30 d after surgery or during hospital stay.Survival was evaluated after 30 and 90 d and during follow-up.
Due to limited life expectancy and fragility of the patients,there was no standard postoperative follow-up schedule.An absence in consultations for more than 12 mo was considered loss of follow-up.
Surgical technique
Briefly,GP was performed as follows.Upon confirmation that the tumor was unresectable,the lesser sac was accessed,and the posterior gastric wall was inspected to confirm that there was a tumor-free area for anastomosis.For GP,a point located at least 5 cm proximal to the tumor along the gastric curvatures was chosen.Faucher's tube (32Fr) was positioned along the lesser curvature to ensure a small conduit between the two gastric chambers created by partitioning.It enabled subsequent endoscopic observation of the bypassed tumor.The stomach was partitioned through mechanical linear stapler from the greater curvature towards the Faucher's tube along the lesser curvature.A side to side GJ,30 cm from the ligament of Treitz,was performed in the proximal part of the stomach (Figure 1).In some cases,Roux-en-Y reconstruction was also performed.Conventional GJ was performed along the posterior gastric curvature hand-sewn or with stapler device,viaan antecolic or retrocolic route.Deciding which procedure should be performed was not controlled and defined by the surgeon responsible for each case.
Statistical analysis
Descriptive statistics included frequencies by percent for nominal variables and means with standard deviation for continuous variables.Chi-square tests were used for categorical data to evaluate the differences between variables,and thet-test was used for continuous data.Overall survival (OS) was estimated using the Kaplan-Meier method,and differences in survival were examined using the log-rank test.The survival period was calculated from the date of surgery until the date of death.Living patients were censored at the date of last personal contact.All tests were two-sided and statistical significance was defined asP <0.05.Analysis was performed using SPSS software,version 18.0 (SPSS Inc,Chicago,IL,United States).
RESULTS
A total of 60 GC patients underwent gastric bypass due to irresectable distal GC.GP was performed in 30 patients and conventional GJ in the other 30 patients.Initial nutritional variables including hemoglobin,albumin,weight and BMI did not differ between groups (Table 1).KPS and ECOG were worse in GP patients.The presence of distant and peritoneal metastasis was also similar between groups.The complete impossibility of oral ingestion or ingestion of only liquids (GOOS 0-1) were present in 60% of patients in both groups.
Operative outcomes are demonstrated in Table 2.The mean operative time was higher in the partitioning group (161.2vs85.2 min,P <0.001).Roux-en-Y reconstruction was performed in 16 patients (57.1%) in the GP group and in none of the GJ group.Manual anastomosis was more common in the partitioning group(42.9%vs6.7%,P =0.001).There were no differences regarding postoperative complications and surgical mortality between groups.The mean time in days for ingestion of liquids (GOOS 1),soft diet (GOOS 2),and length of hospital stay was similar between groups.GOOS 2 and 3 were reached by 28 GP patients (93.3%) and 22 GJ patients (75.9%) (P =0.080).
基于模糊综合评价法的PPP项目绩效评价体系研究——以广西壮族自治区那考河流域治理项目为例梁素萍 李钦琳23-55
The evolutionary control of weight gain after the procedure evidenced that,after 30 and 90 d,there was no difference between groups (Table 3).Maximum mean weight recorded after surgery was similar between GP and GJ groups (56.6vs56.8 Kg,P =0.966).A second additional procedure was necessary in four patients in each group to establish nutritional enteral access,which included an enteral feeding tube.
The mean follow-up was 9.2 mo (median of 6.6 mo,standard deviation [SD] ± 9.7)Forty-nine (81.6%) patients died during that period.The median OS of the entire sample was 8 mo (range 0.1-50.5).Regarding the type of surgery,there was no difference in survival between the groups.The median OS was 7 and 8.4 mo for the GP and GJ groups,respectively (P =0.610) (Figure 2).
The multivariate analysis of clinicopathological characteristics and operative outcomes associated with OS demonstrated that only GOOS 2-3 after surgery were statistically significant in improving survival (hazard ratio [HR]: 8.90; 95% confidence interval [CI]: 3.38-23.43,P <0.001) (Table 4).The type of surgery (GJvsGP) was not associated with improvement in OS (HR: 1.16,95%CI: 0.65-2.07,P= 0.612).

Figure 1 GP and GJ for malignant gastric cancer.
DISCUSSION
GP proved to be as effective as GJ for the treatment of GOO.Both procedures had similar results regarding postoperative complications and no difference in survival was found.Nevertheless,there was a trend for GP in promoting better acceptance of soft solids,low residue,and full diets (GOOS 2-3) by the patients (P= 0.08).These results reinforce GP as a valid option to be added to GJ in the treatment of GOO.
Recently,endoscopic stents have gained popularity to treat such a condition[13].It is less invasive and can be performed outside the operating room.The return of oral intake is faster with a shorter length of hospital stay.As a disadvantage,the method presents an acute risk of bleeding,perforation,and stent migration.In the long-term,tumor growth may lead to stent obstruction with the necessity of reinterventions[14].According to the multicenter randomized trial SUSTENT,endoscopic stents are mostly indicated for patients with poor status performance,high surgical risk,and life expectancy less than 2 mo[8].Patients with better clinical conditions and with the possibility of receiving palliative chemotherapy have a potential benefit of definitive surgical gastric derivation[15].

Table 1 Clinicopathological characteristics of all patients
The first report of GP was made by Devineet al[10]in 1925,in a patient with obstruction caused by a complex duodenal ulcer.Maingotet al[16]in 1936 first reported its use in gastric cancer.In both cases,partitioning of the stomach was complete.This fact led to closed loop syndrome of the distal gastric stump with the risk of a blowout as a consequence of inadequate drainage of the gastric fluids from the excluded stomach.Yet,bleeding from the tumor may occur.
After those initial reports,there were no further publications regarding that method.Nevertheless,its employment gained prominence after Kaminishi's report in 1997.In that original series,31 unresectable GC patients with GOO underwent either GP or GJ.The rates of acceptance of a regular meal at 2 wk after the operation were 88% in the partitioning group and 31% in the GJ group (P <0.05).Still,the mean survival times for GP and GJ were 13.4 and 5.8 mo,respectively (P <0.05)[17].The authors presented a modification in the technique,maintaining a small communication between the two gastric chambers created after the partitioning.This communication avoids closed loop syndrome and the risk of a blowout.It also allows the endoscopic access to the tumor and the biliary tree in case of the necessity of biliary drainage.Still,gastric acid entry into the antrum is also maintained,decreasing the stimulation of gastrin and consequent risk of ulcer formation[18].Regarding GE,the proximal gastric chamber created by partitioning has smaller dimensions in relation to the entire stomach,which is also dilated in many cases.The reduction in organ dimensions decreases the formation of recesses distal to the anastomosis and in the proximal body and gastric fundus.Thus,it may decrease the recirculation of the ingested food inside the stomach,facilitating its flow to the anastomosis and decreasing the GE time.

Table 2 Surgical outcomes
Advantages attributed to partitioning include improving GE and reducing tumor bleeding due to less contact of ingested food.Still,it reduces the necessity of blood transfusion.Besides that,improving food intake and reducing bleeding help patients to better tolerate the effects of palliative chemotherapy,which may improve survival[19-21].Another interesting aspect of such a procedure is the fact that the tumor is isolated in the distal gastric chamber.Subsequently,the possibility of obstruction of the GJ by tumor growth is minimized.In addition,this technique has also been applied for tumors of the biliopancreatoduodenal confluence[9,18].
As a disadvantage,the addition of a stapling line creates new potential sites for postoperative fistula.The operative time may also increase,as shown in the present study.However,the persistent attempt to accomplish tumor resection and the greater proportion of cases with Roux-en-Y reconstruction may have influenced this result.Thus,we believe that after the technique becomes routine,this increment in operative time due to the addition of the partitioning is minimal.There is no consensus regarding the need for Roux-en-Y reconstruction.The presence of biliary flow to the stomach due to the GJ is something that theoretically can impair GE.Moreover,reflux alkaline gastritis and afferent loop syndrome may impair acceptance of diet.The use of a Roux-en-Y reconstruction or the addition of Braun enteroenterostomy may prevent these complications[22].However,as patients have limited life expectancy,the alleged short and long-term complications of biliary reflux were not observed in our study.Thus,Roux-en-Y reconstruction may not be justified.
Both procedures can be safely performed by laparoscopy[23-25].They may also be performed during a staging laparoscopy with palliative intent or even to improve nutritional status in a patient with neoadjuvant or conversion therapy indication[26].
支气管哮喘(简称哮喘)是一种以慢性气道炎症为特征的异质性疾病,主要特征改变包括气道慢性炎症、气道高反应性(AHR)、可逆性气流受限及气道结构的改变,即气道重构[1-2]。哮喘的病理机制不仅是Thl/Th2免疫失衡,可能是对变应原的免疫耐受异常和免疫缺陷。益气固本胶囊系根据国医大师王烈教授验方制成,用于哮喘病缓解期的治疗,具有益气养阴、补肺脾肾的功效,本方临床运用多年,可有效降低哮喘复发率[3]。因此,本研究从分子、细胞水平观察,益气固本胶囊对卵白蛋白致敏的哮喘小鼠IL-33、TNF-α水平及CD4+CD25+Foxp3+调节性T细胞数量的影响,从体外实验观察益气固本胶囊对哮喘免疫失衡的影响。
When comparing the techniques,the outcomes analyzed vary in literature.Regarding early postoperative results,DGE is widely used but the way of classifying is not standardized and is somewhat subjective.The International Study Group of Pancreatic Surgery definition has been employed[27].It conceptually defines DGE when a nasogastric tube is required for 8 d or limited oral intake cannot be tolerated by postoperative day 14.This criterion may be too strict,causing lack of documentation of cases with mild DGE.Ernberget al[9]reported a significantly lower incidence of DGE in GP patients (0%) compared with the GJ (42.9%,P =0.024).Additionally,oral nutrition alone was recorded more often at follow-up in the partitioning group (9/9,100%) than in the GJ group (4/13,30.8%) (P =0.002).Thus,in the present study,we decided to evaluate the time to reach GOOS scores 2 and 3.Both groups took the same average of days for diet acceptance and progression.However,the partitioning group had a trend to present higher final values of GOOS.The length of hospital stay is another early outcome commonly used.It indirectly reflects the ability of oral ingestion acceptance.In addition,it is influenced by other factors of interest such as postoperative complications.
Kumagaiet al[28]published a meta-analysis comparing GP with GJ.Seven studies containing 207 patients were included.GP had a significantly lower risk of DGE(relative risk: 0.32; 95%CI 0.17 to 0.60;P <0.001) and shorter postoperative hospital stay (mean of 6.1 d;P <0.001).Conversely,no significant differences were observed in operative time,blood loss,postoperative complications and anastomotic leak[28].
The main long-term goals of GP are the maintenance of oral intake capacity and survival.What can be verified is that once the GOO is successfully solved,either with GP or GJ,patients maintain the capacity to eat until near death.Only 13.3% of patients did require additional procedures to maintain the alimentary route.When that happened,it was doubtful whether the failure was exclusively due to the initial procedure causing GOO recurrence or due to disease progression.The weight regain was also similar between the two groups,confirming the equal long-term effectiveness of both procedures to maintain oral intake.
Improved OS has been reported with GP[19-21].The fact that the tumor is excluded in the distal gastric chamber leads to a lower occurrence of tumoral bleeding.Less bleeding associated with improvement in oral intake allows better use of palliative chemotherapy with a beneficial effect on OS.However,we did not verify this result in our study (P =0.08).It could be speculated that,with more patients in the analysis,perhaps some differences among the two techniques would appear.Yet,the GP group had lower values of KPS and ECOG.The selection bias of patients with worse performance and consequently worse OS may have influenced this result.Lastly,multivariate analysis showed that the main prognostic factor in patients with GOO was the ability to eat better after the procedure regardless of the technique used (HR:8.90,95%CI: 3.38-23.43,P< 0.001).

Table 3 Control of weight after the procedure
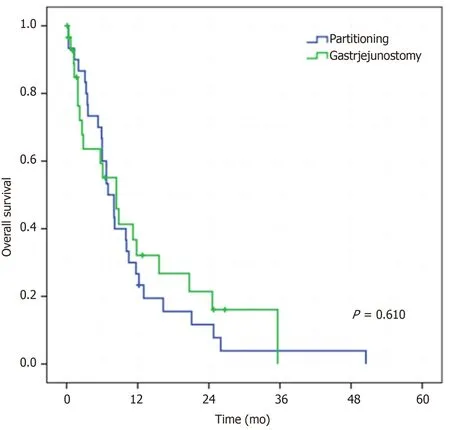
Figure 2 Overall survival for GP and GJ (P = 0.610).
Retrospective studies have limitations inherent to their design.The selection of patients for both techniques was not done in an equivalent manner.In the past 10 years,GP has been the procedure of choice for GOO cases in our institution.The decision to perform conventional GJ still takes place as an option,especially in urgent cases or when the surgeon is not familiar with the partitioning technique.This situation allowed us to create a control group.Fortunately,exactly 30 patients were included in the control group in the same period.In order to increase group sampling,it was thoughtful to include patients from previous periods when partitioning was not performed.However,this would bring the disadvantage of not including recent advances in palliative treatment in GC,which would have an impact on survival.Surprisingly,clinicopathological characteristics of patients in both groups were almost similar,with the exception of KPS and ECOG scores,not making the comparison so unequal.
To overcome these limitations,a prospective randomized study comparing GP with GJ was initiated at our institution.Thus,currently,no patient is submitted to any procedure for the treatment of GOO outside the prospective protocol.The study is ongoing recruiting patients and is expected to be completed within the next year(ClinicalTrials.gov: NCT02064803).
In summary,GP proved to be a safe and effective procedure for the treatment of GOO.Compared to conventional GJ,GP has similar early and late outcomes with a trend to better solid diet acceptance by the patients.
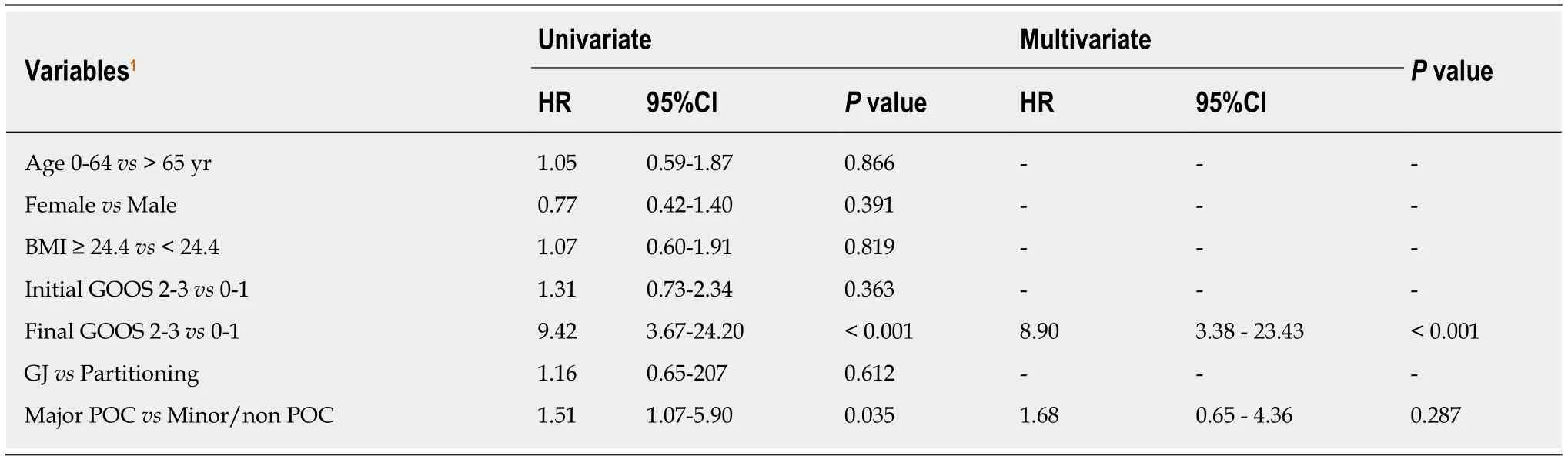
Table 4 Univariate and multivariate analyses for survival - Cox regression
ARTICLE HIGHLIGHTS
Research background
Gastric outlet obstruction (GOO) is a common complication during gastric cancer treatment.Different treatment modalities have been employed including endoscopic stent placement,surgical resection,and surgical bypass procedures.Surgical bypass may have better results when life expectancy is larger than 2 mo.It may be performed with a simple gastrojejunostomy (GJ) or with the addition of partial gastric partitioning (GP).
Research motivation
GJ has been traditionally performed as bypass procedure for GOO.However,delayed gastric emptying with impaired food ingestion may occur in up to 26% of cases.To overcome this setback,GP has been employed.The partitioning creates two separated gastric chambers that may improve gastric emptying,decrease tumor bleeding,and improve survival.
Research objectives
We compared the surgical results of GJ and GP for the treatment of GOO in patients with unresectable distal gastric cancer.
Research methods
We performed a retrospective analysis of 60 patients submitted to GJ and GP between 2009 and 2018.Clinicopathological characteristics and surgical outcomes were compared.
Research results
GP was performed in 30 patients and conventional GJ in the other 30 patients.Baseline clinicopathological characteristics were similar between groups,with the exception of worse performance status in GP patients.Surgical results related to postoperative complications and surgical mortality did not differ between groups.The median OS was 7 and 8.4 mo for GP and GJ groups,respectively (P = 0.610).The oral acceptance of soft solids (GOOS 2) and low residue or full diet (GOOS 3) were reached by 28 (93.3%) GP patients and 22 (75.9%) GJ patients (P =0.080).After multivariate analysis,acceptance of soft solids and low residue or full diet was the main prognostic factors for survival despite the surgical procedure performed (HR: 8.90,95%CI:3.38-23.43,P < 0.001).
Research conclusions
GP is a safe and effective procedure to treat GOO.Compared to GJ,it provides similar early and late outcomes with a trend to better solid diet acceptance by the patients.
Research perspectives
After this initial experience using GP,a prospective trial was initiated and currently no patient has been submitted to any procedure for the treatment of GOO outside the protocol.The study is ongoing,recruiting patients,and is expected to be completed within the next year(ClinicalTrials.gov: NCT02064803).
ACKNOWLEDGEMENTS
The authors thank other members of the service involved in gastric cancer treatment:Andre R Dias,Claudio JC Bresciani,Marcelo Mester,Osmar K Yagi,Amir Z Charruf,and Fabio P Lopasso.
 World Journal of Gastrointestinal Oncology2019年12期
World Journal of Gastrointestinal Oncology2019年12期
- World Journal of Gastrointestinal Oncology的其它文章
- Observation or resection of pancreatic intraductal papillary mucinous neoplasm: An ongoing tug of war
- Improved method for inducing chronic atrophic gastritis in mice
- Relationship between cachexia and perineural invasion in pancreatic adenocarcinoma
- Protein expression trends of DNMT1 in gastrointestinal diseases: From benign to precancerous lesions to cancer
- Asian Americans have better outcomes of non-metastatic gastric cancer compared to other United States racial groups: A secondary analysis from a randomized study
- Difference in failure patterns of pT3-4N0-3M0 esophageal cancer treated by surgery vs surgery plus radiotherapy
