Piperacillin enhances the inhibitory effect of tazobactam on β-lactamase through inhibition of organic anion transporter 1/3 in rats
aDepartment of Clinical Pharmacology,College of Pharmacy,Dalian Medical University,Dalian 116044,China
bProvincial Key Laboratory for Pharmacokinetics and Transport,Dalian Medical University,Dalian 116044,China
cDepartment of pharmacy,First Affiliated Hospital of Dalian Medical University,Dalian 116044,China
dWuya College of Innovation,Shenyang Pharmaceutical University,Shenyang 110016,China
eCollege(Institute)of Integrative Medicine,Dalian Medical University,Dalian 116044,China
ABSTRACT To assess the mechanism of the pharmacokinetic interaction between piperacillin and tazobactam,renal excretion and pharmacokinetic studies of piperacillin/tazobactam were investigated in normal and bacteremia rats.A bacteremia model was established to investigate the pharmacokinetic properties of piperacillin and tazobactam under different conditions.Renal slices were taken to examine the uptake of piperacillin and tazobactam.Pharmacokinetic studies of β-lactamase in rats were performed to study the contribution of rOat1/3 to the inhibition of tazobactam on β-lactamase.The AUC(from 2.93±0.58 to 6.52±1.44 mg·min/ml)and the plasma clearance(CLP)(from 2.41±1.20 to 0.961±0.212 ml/min/kg)of tazobactam were both altered after the intravenous coadministration of piperacillin and tazobactam in the bacteremia rats.The renal clearance(CLR)of tazobactam decreased from 1.30±0.50 to 0.361±0.043 ml/min/kg.In summary,there was a beneficial interaction between piperacillin and tazobactam mediated by rOat1 and rOat3.Piperacillin enhances the inhibitory effect of tazobactam on β-lactamase through the inhibition of rOat1 and rOat3 in rats.The contribution rate of rOat1/3 for the synergistic effect was 20%when the two drugs were coadministered.
Keywords:Organic anion transporter Piperacillin Tazobactam Drug-drug interaction
1.Introduction
Piperacillin/tazobactam is an effective antibacterial drug against clinical common gram-negative and gram-positive bacteria,including many bacteria that produceβ-lactamases[1].Piperacillin/tazobactam is helpful in treating respiratory infections,soft tissue infections,intra-abdominal infections,urinary infections,gynecologic infections and bacteremia[2].With the prevalence ofβ-lactamase-producing bacteria,the clinical challenge posed byβ-lactamase is complex[3].Compound formulations of tazobactam and piperacillin have successfully protected and expanded the activity of piperacillin againstβ-lactamase-producing bacteria,thus enhancing its potential clinical applications.
Previous studies have shown that piperacillin significantly reduces the clearance ratio(Cr)and renal clearance(CLR)of tazobactam in dogs[4].Probenecid can also significantly inhibit the renal excretion of piperacillin and tazobactam.Piperacillin and tazobactam are excreted mainly through the kidneys(50%-60%),with very little bile excretion(<2%)[5].The metabolite of tazobactam,which is formed by the cleavage of theβ-lactamase ring and further breakdown to a butanoic acid derivative,has noβ-lactamase inhibitory activity.The two metabolites formed by theβ-lactamase ring cleavage contribute insignificantly to the elimination of piperacillin[6].Furthermore,tazobactam and piperacillin are secreted mainly through the renal tubular anion transporters[4],and a longer half-life of tazobactam and a stronger antibacterial activity of piperacillin were noted in the PK-PD model[7].These studies suggested that in addition to traditional theories,in which tazobactam inhibitsβ-lactamase to reduce the hydrolysis of piperacillin,piperacillin might also enhance the efficacy of tazobactam by inhibiting the excretion of tazobactam.On the one hand,piperacillin may increase the plasma exposure of tazobactam by inhibiting the renal excretion of tazobactam.On the other hand,increasing the plasma exposure of tazobactam may further enhance the ability of tazobactam to inhibitβ-lactamase.To summarize,there might be a beneficial interaction between piperacillin and tazobactam,possibly through their renal excretory process,which enhances the efficacy of tazobactam.
It is generally known that mostβ-lactamase antibiotics are excreted into the urine through OATs located on the basolateral membranes of proximal tubules[8].According to the report,piperacillin could inhibit the renal excretion of variousβ-lactamase antibiotics[9].These findings showed that OATs played an important role in the renal excretion ofβlactamase antibiotics.However,it is unclear whether OATs are involved in piperacillin and if this involvement enhances the inhibitory effects of tazobactam onβ-lactamase.Thus,we speculated that there might be a beneficial interaction between piperacillin and tazobactam and that piperacillin might interfere with the renal transport of tazobactam via OAT1/3,thus slowing the renal clearance of tazobactam and further enhancing the inhibitory effect of tazobactam onβ-lactamase.
To elucidate the mechanism of the drug interaction between piperacillin and tazobactam in the infective state,the pharmacokinetic interactions were investigated byin vivopharmacokinetic study andin vitrokidney slices.This work was carried out in a rat model of bacteremia induced byKlebsiella pneumoniainfection.Moreover,we investigated the activity ofβ-lactamase in the plasma after intravenously administratingβ-lactamase with piperacillin and/or tazobactam in rats.TheAUC0-∞ofβ-lactamase was assessed as an indicator ofβ-lactamase activity to evaluate the contribution of rOat1/3 to the inhibition ofβ-lactamases.
2.Materials and methods
2.1.Materials
Sodium salts of piperacillin,tazobactam,sulbactam and avibactam were all purchased from Dalian Meilun Biotech Co.,Ltd.(Dalian,China).p-Aminohippuric acid(PAH),penicillin G(PCG)and probenecid were purchased from Sigma(USA).The strain ofK.pneumoniaproducing extended spectrumβlactamases(ESBLs)was a clinical isolate and was obtained from the first affiliated hospital of Dalian medical university.β-lactamase production was confirmed using polymerase chain reaction(PCR)and isoelectric focusing.Bacterial strains were stored at-70 °C as glycerol stocks.TEM-1β-lactamase was purchased from Shanghai Aladdin Biochemical Technology Co.LTD.(Shanghai,China).All other chemical reagents were of analytical grade.
2.2.Animals
Male Wistar rats weighing 220-250 g were purchased from the SPF Experimental Animal Center of Dalian Medical University(SCXK 2013-0003).Rats were housed in an animal room with an alternating 12-h light/dark cycle at 20°C and 60%relative humidity.They were acclimated for 1 week.Rats were fasted for 12 h before the experiment.All rat experiments were conducted in accordance with the UK Animals(Scientific Procedures)Act,1986 and associated guidelines,EU Directive 2010/63/EU for animal experiments.Every effort was made to ensure the welfare of the animals.
2.3.Rat model of bacteremia
Rat models of bacteremia were based on a method described in the previous literature[10].In short,the strain ofK.pneumoniawas inoculated in liquid Luria-Bertani broth at 37 °C(shaken at 120 rpm)and harvested by centrifugation at 4000×gfor 10 min.The precipitate was washed three times with sterile 20 mM phosphate buffered saline(pH 7.4).The precipitate was suspended in sterile saline solution and adjusted to the desired concentration.The bacterial concentration and duration of infection were optimized in the preliminary experiment.A total of 0.3 ml of 4×109CFU/mlK.pneumoniawas the maximum concentration that could be intravenously injected without causing mortality.Rats were injected with 0.3 ml ofK.pneumonia(4×109CFU/ml)via the tail vein.A total of 0.2 ml of whole blood was collected from the orbital venous plexus at 1,5,10,24,48 and 72 h after administration for a white blood cell count.The levels of C-reactive protein and procalcitonin were also assayed.
2.4.Pharmacokinetic interactions in rats
Rats were divided randomly into four groups:(1)tazobactam administration in normal rats;(2)tazobactam+piperacillin administration in normal rats;(3)tazobactam administration in the rat model of bacteremia;(4)tazobactam+piperacillin administration in the rat model of bacteremia.The doses of piperacillin and tazobactam were 210 mg/kg and 26.25 mg/kg,respectively.The tested drugs were dissolved in 0.9% saline.The rats received an intravenous injection in the caudal vein of a suspension ofK.pneumonia5 h before the intravenous administration of the tested drugs in groups 3 and 4.Rats were fixed on the operating table after being anesthetized with pentobarbital(60 mg/kg,ip).Their bladders were intubated with tubing for urine collection.Blood samples(~200 μl)were collected from the jugular vein at 2,5,15,30,60,120,180,240,300 and 360 min after intravenous administration.Blood samples were collected in heparin centrifuge tubes and immediately centrifuged at 4000×gfor 5 min to obtain the plasma samples.Urine samples were collected from the bladder cannula at 1,2,4,6,8,12 and 24 h after administration.Samples were stored at-20 °C.The concentration of tazobactam and piperacillin were measured by LC-MS/MS.
2.5.In vitro uptake in kidney slices
Normal rats and bacteremia rats were fixed on the operating table after anesthetizing with pentobarbital(60 mg/kg,ip).Rats in the bacteremia group received an intravenous injection in the caudal vein of a suspension ofK.pneumonia5 h before the operation.After anesthesia,the rat kidneys were removed quickly and immediately placed into an oxygenated buffer at 4 °C[11,12].The collected kidneys were sectioned to a thickness of 300 μm using a tissue slicer(ZQP-86).After preincubation for 5 min in buffer at 37 °C,kidney slices were put into 1 ml of buffer containing piperacillin(250 μM),tazobactam(50.0 μM)and piperacillin(250 μM)+tazobactam(50.0 μM),respectively.Piperacillin and tazobactam were dissolved in the transport buffer.After incubation,the kidney slices were removed from the buffer at 1,5,10,15,20 and 30 min,respectively.The kidney slices were rinsed with ice-cold water three times,then dried with filter paper and homogenized(IKA-T10)with 300 μl of normal saline solution.The inhibitory effects of PAH(0.100 mM),PCG(0.100 mM)and probenecid(0.100 mM)on the uptake of tazobactam were also investigated.The accumulated concentrations of piperacillin and tazobactam in the kidney slices were determined by LC-MS/MS.The transport buffer consisted of 120 mM NaCl,16.2 mM KCl,1.00 mM CaCl2,1.20 mM MgSO4and 10.0 mM NaH2PO4/Na2HPO4,adjusted to pH 7.4.
2.6.Sample preparation
Plasma sample preparation was based on a method referred to in the previous literature[13].In short,200 μl of acetonitrile and 50.0 μl of sulbactam(IS of tazobactam,acetonitrile)or avibactam(IS of piperacillin,acetonitrile)was added to 50.0 μl of plasma sample.The mixed liquid was vortex-mixed and centrifuged at 11 000×gfor 10 min.The preparation of kidney slices and urine was the same as that of the plasma samples.Then,10 μl of supernatant was injected into the LC-MS/MS system for analysis.
2.7.Pharmacokinetic study of β-lactamase in rats
The normal rats were divided randomly into four groups:(1)β-lactamase administration;(2)β-lactamase+tazobactam administration;(3)β-lactamase+piperacillin administration;(4)β-lactamase+tazobactam+piperacillin administration.The doses of piperacillin and tazobactam were the same as before.β-lactamase,prepared with 0.9% saline and stored at-20°C,was intravenously administered to groups 1,2,3 and 4 at doses of 25.0 mU/kg(2 min before the intravenous administration of other test drugs).The sampling time and processing method of plasma samples were consistent with previous descriptions.
To determine theβ-lactamase activity in the plasma,PCG was used as a probe drug.An LC-MS/MS method was established to measure the amount of PCG remaining in samples after incubation.The samples were processed as previously described[14],with some modifications.To 100 μl of plasma,20.0 μl of PCG solution(500 μg/ml,PBS)and 100 μl of PBS(pH 7.4)were added.The incubating system was then incubated at 37°C for 1 h.Each sample was analyzed in duplicate.The reaction was stopped by 200 μl of acetonitrile containing IS(penicillin V,100 μg/ml).Then,the mixture was vortex-mixed and centrifuged at 11 000×gfor 10 min.Then,10 μl of supernatant was injected for LC-MS/MS analysis.The activity levels ofβlactamase were calculated by linear regression analysis of the percentage of PCG remainingversusstandards ofβ-lactamase activity.
2.8.LC-MS/MS equipment and conditions
An Agilent HP1200 liquid chromatography system(Agilent Technology Inc.,USA)was used.Mass spectrometric detection was performed on an API 3200 triple-quadrupole mass spectrometer(Applied Biosystems,USA).The analysis condition was described separately as follows:
2.8.1.Analysis condition for piperacillin and tazobactam
Chromatographic separation was achieved on a Venusil ASBC18column(150 mm×4.6 mm,5 μm).The mobile phase system consisted of 80%(v/v)5 mM ammonium acetate solution with 0.1% formic acid and 20%(v/v)acetonitrile for tazobactam and sulbactam(IS);50%(v/v)5 mM ammonium acetate solution with 0.1% formic acid and 50%(v/v)acetonitrile for piperacillin and avibactam(IS).The flow rate was set at 0.7 ml/min.
The mass spectrometer was operated in negative ion mode using an electrospray ionization source(ESI).Optimized ion spray voltage and temperature were set at-4500 V and 500°C.The multiple reaction monitoring(MRM)mode was utilized to detect the fragmentation transitions:m/z298.7→138.3 for tazobactam,andm/z231.8→140.1 for sulbactam(IS).DP and CE were set at 60 V and 30 eV,respectively,withm/z516.1→233.4 for piperacillin,andm/z263.7→95.8 for avibactam(IS).The DP and CE levels were 80 V and 40 eV,respectively.PAH,PCG and probenecid were measured as described previously[15].
2.8.2.Analysis conditions for β-lactamase activity
Chromatographic separation was achieved on a Venusil ASBC18column(150 mm×4.6 mm,5 μm).The mobile phase system consisted of 75%(v/v)water with 0.1% formic acid and 25%(v/v)acetonitrile for PCG and penicillin V(IS)at a flow rate of 0.8 ml/min.
The electrospray ionization source was chosen for MS detection.Optimized ion spray voltage and temperature were set at 4500 V and 450°C.The scanning mode was set as MRM,and the related parameters were as follows:m/z335.1→217.2 for PCG,andm/z351.2→257.0 for penicillin V(IS).The DP and CE were set at 50 V and 35 eV,respectively.
2.9.Data analysis
The Analyst software(version1.4.1)was used for the data acquisition and analysis.The pharmacokinetic parameters of piperacillin and tazobactam were calculated using DAS2.0 software.
CLpwas calculated using Eq.(1);CLRof tazobactam was calculated using Eq.(2):

whereAUCivwas the area under the plasma concentrationtime profile after intravenous injection;Atotalwas the total cumulative amount of tazobactam excreted in the urine over a 24 h period.
The contribution of interaction between piperacillin and tazobactam was mediated by rOat1/3 by enhancing the inhibitory effects of tazobactam onβ-lactamase.This was calculated using Eqs.(3)-(6).
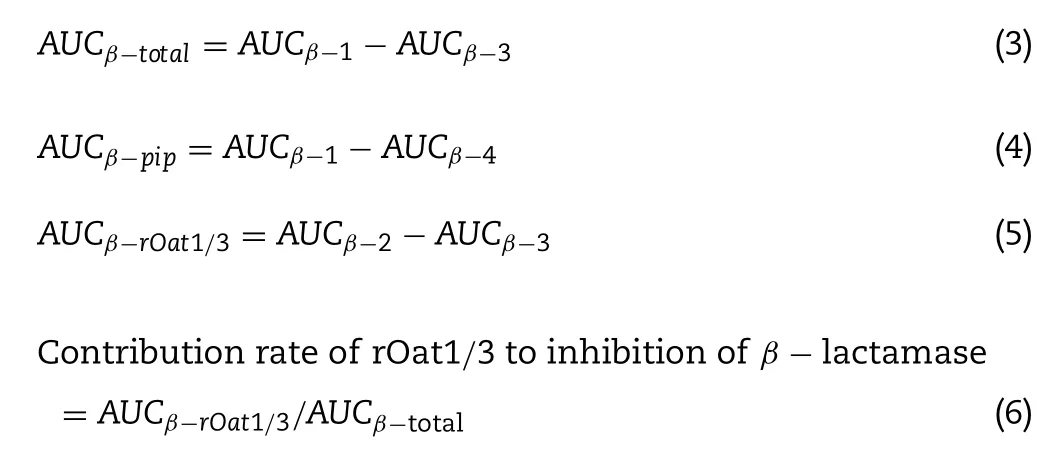
whereAUCβ-1was the area under the plasma concentration of theβ-lactamase-time profile after the intravenous administration ofβ-lactamase;AUCβ-2was the area under the plasma concentration of theβ-lactamase-time profile after the intravenous coadministration ofβ-lactamase and tazobactam.AUCβ-3was the area under the plasma concentration ofβ-lactamase-time profile after the intravenous coadministration ofβ-lactamase,piperacillin and tazobactam;AUCβ-4was the area under the plasma concentration of theβ-lactamase-time profile after the intravenous coadministration ofβ-lactamase and piperacillin.AUCβ-totalwas the decrease in the area under the plasma concentration of theβlactamase-time profile after the intravenous coadministration ofβ-lactamase,piperacillin and tazobactam compared with intravenous administration ofβ-lactamase alone;AUCβ-rOat1/3was the decrease in the area under the plasma concentration ofβ-lactamase-time profile after intravenous coadministration ofβ-lactamase,piperacillin and tazobactam compared with intravenous coadministration ofβ-lactamase and tazobactam.
2.10.Statistical analysis
Statistical analyses were conducted using SPSS version 20.0(SPSS Inc.,Chicago,IL,USA).Values are represented as the means±SD.Significant differences in the data between the study groups were assessed usingt-tests or one-way ANOVA followed by Dunnett’s test for multiple treatments.Values ofP<0.05 were considered to be statistically significant.A power calculation was performed using G∗power software(3.1.9.2)to ensure that there was enough power(1-β>0.8)to detect significant differences in the data.
3.Results and discussion
3.1.Bacteremia and clinical biochemistry
Because piperacillin and tazobactam are used clinically in patients suffering from bacterial infections,we established a model of infection to investigate possible drug interactions.Rats were the most suitable animals for pharmacokinetic studies,and they could also serve as good models for wound and endocarditis infections[16,17].Female animals can have various physiological states that can affect drug disposition[18].The physiologic fluctuation in hormonal levels during the menstrual cycle may further modulate gender differences in drug disposition[19].Thus,we chose male rats as the experimental animals for this study to reduce individual differences among the rats.To elucidate the drug interactions between piperacillin and tazobactam associated with bacteremia,we established a rat model induced byK.pneumoniainfection to investigate the drug interactions.
To evaluate the model of bacteremia,the white blood cell count,procalcitonin and C-reactive protein levels were measured.As shown in Fig.1,the white blood cell count was significantly reduced 5 h postinfection and increased at 72 h postinfection.Although the level of C-reactive protein followed a similar trend as the white blood cell count,the level of Creactive protein was the highest at 10 h.The level of procalcitonin was increased at 72 h postinfection.Changes in the index of infection indicators illustrated relocations between 2 h and 72 h with maximum deviations at 5 h.For this reason,we started the pharmacokinetic experiment at 5 h postinfection.
3.2.The effects of bacteremia on the pharmacokinetics of tazobactam
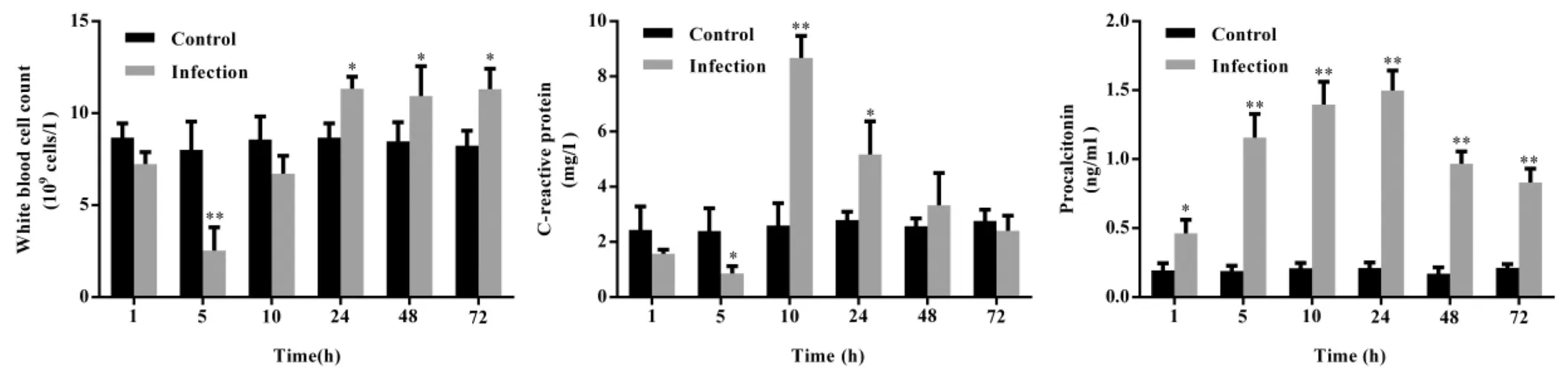
Fig.1-White blood cell count,C-reactive protein and procalcitonin levels in the bloodstream as obtained from K.pneumonia-infected rats compared to the control animals.The data are expressed as the mean±S.D.(∗P<0.05;∗∗P<0.01 vs.control;n=6).
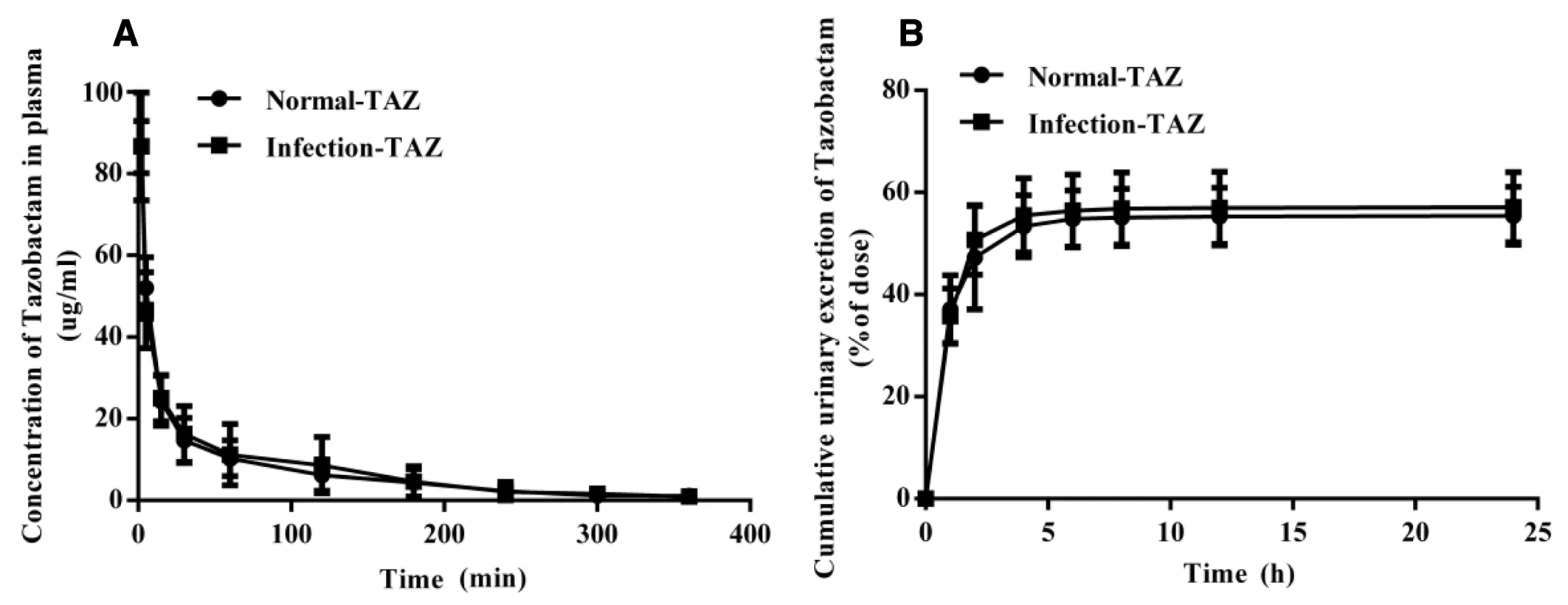
Fig.2-(A)Mean plasma concentration-time curves and(B)accumulative urine excretion curves of tazobactam after the intravenous administration of tazobactam in normal or bacteremia rats.Data are expressed as the mean±SD.(n=6).
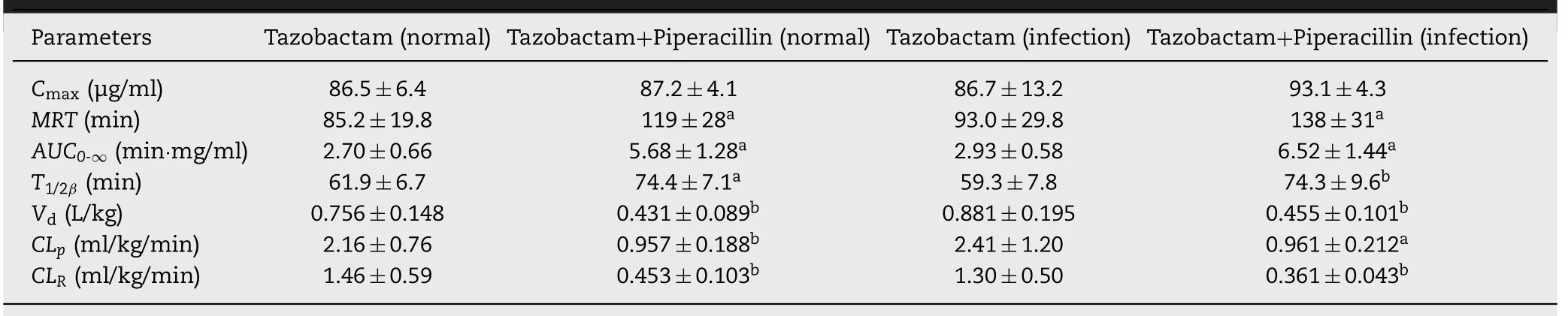
Table 1-Pharmacokinetic parameters of tazobactam following iv administration.
To evaluate whether bacteremia changed the exposure of tazobactam in rats,the pharmacokinetics of tazobactam were investigated in rats.As shown in Fig.2,the plasma concentrations and cumulative urinary excretion of tazobactam did not change between the normal and bacteremia rats.Furthermore,the pharmacokinetic parameters of tazobactam were not significantly changed between the two groups.The results are presented in Table 1.These results indicate that the infection did not change the plasma concentration or renal excretion of tazobactam.Because of the presence ofβ-lactamase in the rat model of bacteremia,it also showed thatβ-lactamase did not affect the pharmacokinetic characteristics of tazobactam in this model.
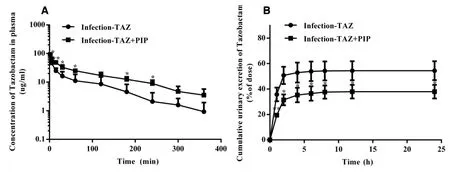
Fig.3-(A)Mean plasma concentration-time curves and(B)accumulative urine excretion curves of tazobactam after the intravenous administration of piperacillin and tazobactam in bacteremia rats.Data are expressed as the mean±SD.(∗P<0.05;∗∗P<0.01 vs.control;n=6).
3.3.The effects of piperacillin on the pharmacokinetics of tazobactam in bacteremia rats
To determine whether piperacillin changed the exposure of tazobactam,piperacillin and tazobactam were coadministered intravenously to evaluate the changes in the tazobactam plasma concentrations.Fig.3A shows that the plasma exposure of tazobactam was increased significantly compared with that in the tazobactam alone group.The results showed that theAUC(from 2.93±0.58 mg·min/ml to 6.52±1.44 mg·min/ml)andCLP(from 2.40±1.20 to 0.961±0.212 ml/min/kg)of tazobactam were both changed.The pharmacokinetic parameters of tazobactam are shown in Table 1.To reveal the target organ of drug interaction between piperacillin and tazobactam,the cumulative urinary excretion of tazobactam was measured during the 24 h after the intravenous coadministration of piperacillin and tazobactam.Fig.3B shows that the renal excretion rate of tazobactam was 54.4% of the dose in the case of tazobactam alone.When piperacillin and tazobactam were coadministered,the renal excretion rate of tazobactam decreased to 37.9%.As shown in Table 1,theCLRof tazobactam decreased from 1.30±0.50 ml/min/kg to 0.361±0.043 ml/min/kg.The results suggested that piperacillin inhibited the renal excretion of tazobactam in the bacteremia model rats.Therefore,we suggested that changes in the pharmacokinetics of tazobactam were not caused by bacteremia but by the interaction between piperacillin and tazobactam.
3.4.The effects of bacteremia on the interaction between piperacillin and tazobactam
To determine whether infection has an impact on the interaction between piperacillin and tazobactam,piperacillin and tazobactam were coadministered intravenously in normal rats and bacteremia rats.As shown in Fig.4A and 4B,there was also no change in the pharmacokinetics of tazobactam between the normal rats and bacteremia rats.The results illustrated that infection did not affect the interaction between the two drugs.
3.5.The effects of bacteremia on the pharmacokinetics of piperacillin
To determine if bacteremia changed the disposition of piperacillin in rats,the pharmacokinetic parameters of piperacillin were investigated.Based on our understanding of the traditional theory of piperacillin/tazobactam,the plasma exposure of piperacillin in bacteremia rats was expected to be significantly lower than that in normal rats administered with intravenous piperacillin alone(Fig.5A).However,as shown in Fig.5B and 5C,it was noted that there was no significant difference in the disposition of piperacillin in normal rats and bacteremia rats administered with intravenous piperacillin and tazobactam.These results suggest that the plasma concentration of piperacillin was not affected byβ-lactamase due to the protective effect of tazobactam in the rat model of bacteremia,which did not affect the drug interaction between piperacillin and tazobactam.
3.6.The uptake of tazobactam in kidney slices in normal rats and bacteremia rats
OAT1 and OAT3 are mainly distributed in the basolateral membrane of the proximal tubules of the kidney and mediate the renal excretion of various antibacterial agents.To demonstrate whether rOat1/3 mediated the interaction between piperacillin and tazobactam in rats,kidney slices were used to clarify this mechanism.As shown in Fig.6A and 6B,the uptake of tazobactam reduced in the coadministered group,suggesting that piperacillin inhibited the uptake of tazobactam.However,when the kidney slices were treated with tazobactam alone,there was no change in the uptake of tazobactam between the normal rats and the bacteremia rats(Fig.6C).The results illustrated that bacteremia did not change the uptake of tazobactam in kidney slices and the interaction between piperacillin and tazobactam occurred in both the normal and infected cases.
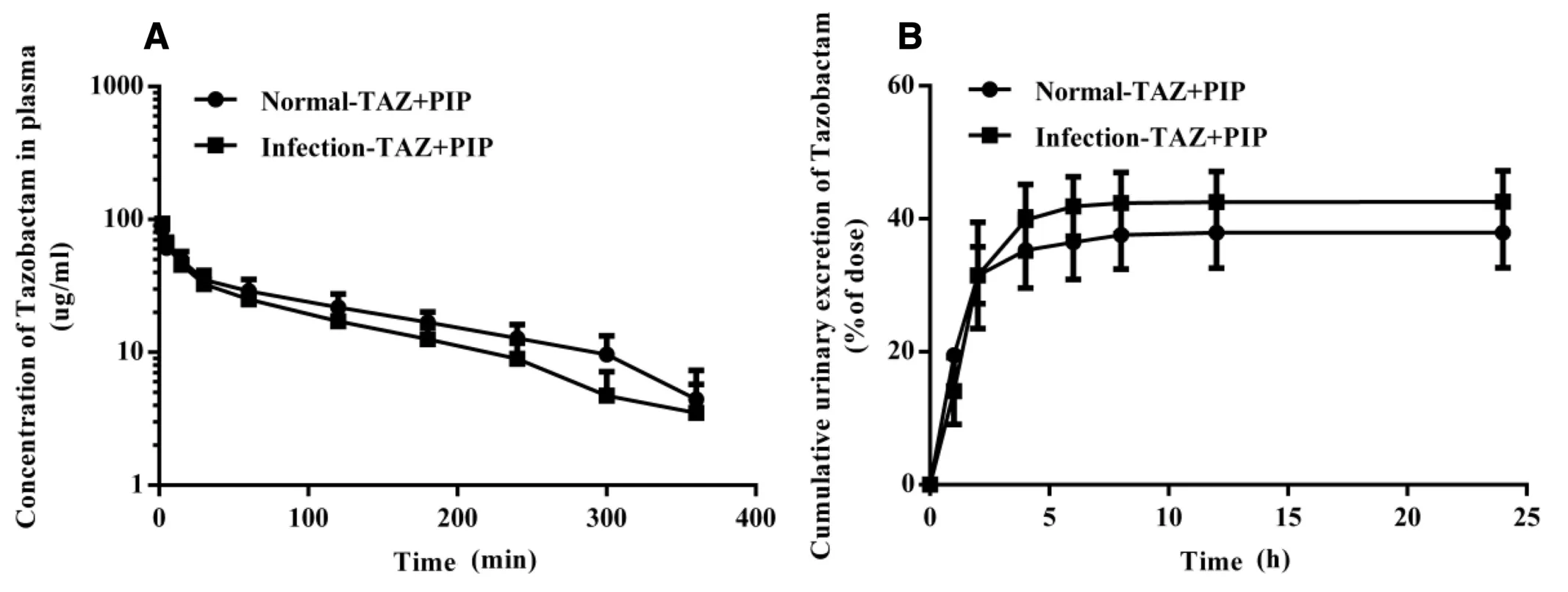
Fig.4-(A)Mean plasma concentration-time curves and(B)accumulative urine excretion curves of tazobactam after the intravenous administration of piperacillin and tazobactam in normal or bacteremia rats.Data are expressed as the mean±SD.(n=6).
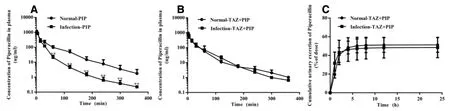
Fig.5-(A)Mean plasma concentration-time curves of piperacillin after the intravenous administration of piperacillin in the normal or bacteremia rats.(B)The mean plasma concentration-time curves and(C)the accumulative urine excretion curves of piperacillin after the intravenous administration of piperacillin and tazobactam in normal or bacteremia rats.Data are expressed as the mean±SD.(n=6).
3.7.The effects of bacteremia on the uptake of piperacillin and tazobactam in kidney slices
To elucidate whether bacteremia affects the uptake of two drugs in kidney slices in the coadministered group,the uptake of piperacillin and tazobactam in kidney slices was investigated.After treatment with the coadministered piperacillin and tazobactam,the uptake of tazobactam in the kidney slices from bacteremia rats was higher than that in normal rats,but no change was seen in the uptake of piperacillin(Fig.7A and 7B).To determine if piperacillin was hydrolyzed byβlactamase,theβ-lactamase activity was detected in kidney slices of bacteremia rats.The results suggest that the kidney slices containedβ-lactamase in bacteremia rats(Fig.8).On the other hand,the uptake of piperacillin in the bacteremia group was significantly lower than that in the normal group(Fig.7C).These findings showed thatβ-lactamase may influence the uptake of piperacillin and tazobactam in the kidney slices.
To determine the mechanism of piperacillin inhibiting the renal excretion of tazobactam,we investigated the timedependent inhibitory effects of PAH,PCG and probenecid on tazobactam uptake in the kidney slices.The findings showed that probenecid(0.100 mM),PCG(0.100 mM)and PAH(0.100 mM)inhibited the uptake of tazobactam.The uptake of tazobactam was reduced by 57.4%,46.2% and 72.0%,respectively(Fig.7D).These findings suggested that rOat1/3 mediated drug interactions between piperacillin and tazobactam in renal excretion.In addition,our research group used hOAT1-/hOAT3-transfected HEK293 cells to reveal the mechanism.We found that tazobactam was a substrate of OAT1 and OAT3 and the uptake of tazobactam in transfected cells was inhibited in the presence of piperacillin.The details of the uptake experiments in transfected cells are provided in another paper that was previously published[20].In this article,the beneficial clinical significance of the interaction of piperacillin and tazobactam mediated by rOat1/3 is further described in the use of the animal model of infection.
Fig.6-The inhibition effects of piperacillin on tazobactam uptake in kidney slices:(A)normal rats;(B)bacteremia rats;(C)the uptake of tazobactam by kidney slices in the normal and bacteremia rats.Data are expressed as the mean±SD.(∗∗P<0.01 vs.control;n=3).
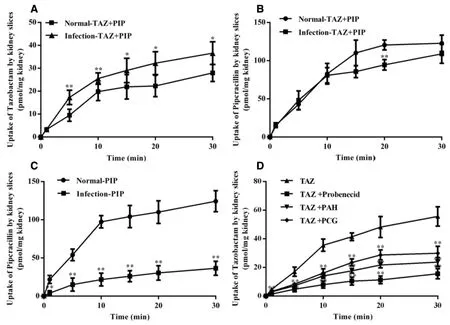
Fig.7-(A)The uptake of tazobactam by kidney slices treated with coadministered piperacillin and tazobactam in normal or bacteremia rats;(B)the uptake of piperacillin by kidney slices treated with coadministered piperacillin and tazobactam in normal or bacteremia rats;(C)the uptake of piperacillin by kidney slices treated with piperacillin in normal or bacteremia rats;(D)the inhibition effects of PAH,PCG and probenecid on tazobactam uptake in kidney slices.Data are expressed as the mean±SD.(∗P<0.05;∗∗P<0.01 vs.control;n=3).
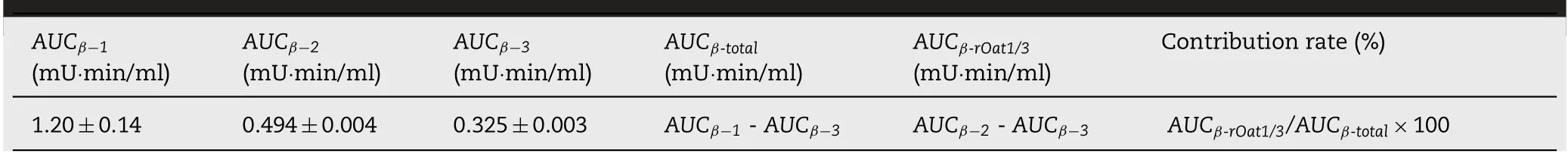
Table 2-Various AUC0-∞of β-lactamase under different administration conditions.
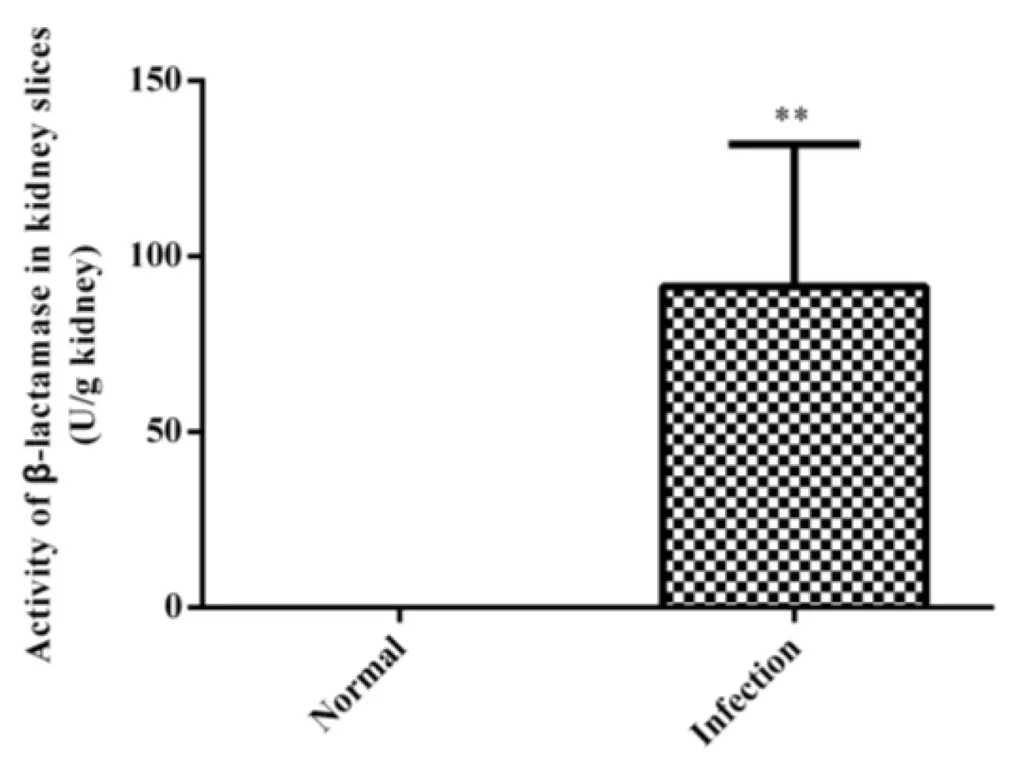
Fig.8-Activity of β-lactamase in kidney slices.Data are expressed as the mean±SD.(∗∗P<0.01 vs.control;n=6).
3.8.Contribution rate of rOat1/3 to the inhibitory effects of tazobactam on β-lactamase
To determine if the inhibition of rOat1/3 by piperacillin could enhance the inhibitory effects of tazobactam onβ-lactamase,the determination ofβ-lactamase in the plasma was investigated after the intravenous administration ofβ-lactamase with piperacillin and/or tazobactam in rats.We then used theAUC0-∞ofβ-lactamase as an indicator of exposure toβlactamasein vivo.The variousAUC0-∞values ofβ-lactamase were calculated under different administration conditions.AUCβ-1was calculated following the administration ofβlactamase alone.AUCβ-2was calculated following the coadministration ofβ-lactamase and tazobactam.AUCβ-3was calculated under coadministration ofβ-lactamase,tazobactam and piperacillin.AUCβ-totaldenoted the full decrease in theβ-lactamase activity after the intravenous coadministration ofβ-lactamase.AUCβ-rOat1/3showed theβ-lactamase activity after the intravenous coadministration ofβ-lactamase.As shown in Table 2,AUCβ-totalequalsAUCβ-1minusAUCβ-3.AUCβ-rOat1/3equalsAUCβ-2minusAUCβ-3.TheAUC0-∞ofβlactamase was 1.20±0.14 mU·min/ml following the single administration ofβ-lactamase(AUCβ-1).TheAUC0-∞ofβlactamase was 0.494±0.004 mU·min/ml following the coadministration ofβ-lactamase and tazobactam(AUCβ-2),and theAUC0-∞ofβ-lactamase was 0.325±0.003 mU·min/ml following the coadministration ofβ-lactamase,tazobactam and piperacillin(AUCβ-3).According to formula(3-6),the results showed that following the coadministration ofβ-lactamase and tazobactam,approximately 20%of the inhibitory effect of tazobactam onβ-lactamase was mediated by rOat1/3(Fig.9).Our experimental data showed that the change in plasma exposure of tazobactam was not proportional to the inhibition of tazobactam onβ-lactamase in the presence of piperacillin.Systemic exposure and renal clearance of tazobactam were changed by 2-fold.However,the change ratio of the inhibition of tazobactam onβ-lactamase was only 20% with the piperacillin combination.The reason might be thatβlactamase could degrade itselfin vivo.In clinical situations,there might be two processes ofβ-lactamase,the generation and degradation in bacterial infection patients.However,we only assessed the degradation ofβ-lactamase in our experiments,andβ-lactamase was only used once in the rats.Therefore,we inferred that the contribution rate of rOat1/3 to the inhibition ofβ-lactamase was higher than the results of our experiment.Based on the above results,we suggested that there was an important clinical implication of synergistic drug interaction between piperacillin and tazobactam.Therefore,we proposed that doctors should focus on the importance of drug interactions mediated by transporters when piperacillin and tazobactam were coadministered.In addition,we should be aware of the significance of transporter-mediated drug interactions in clinical applications and in the development of new drugs.The study of transporter-mediated drug interaction provides a strong theoretical basis for the adjustment of clinical treatment bringing new ideas for the development of new compound preparations.
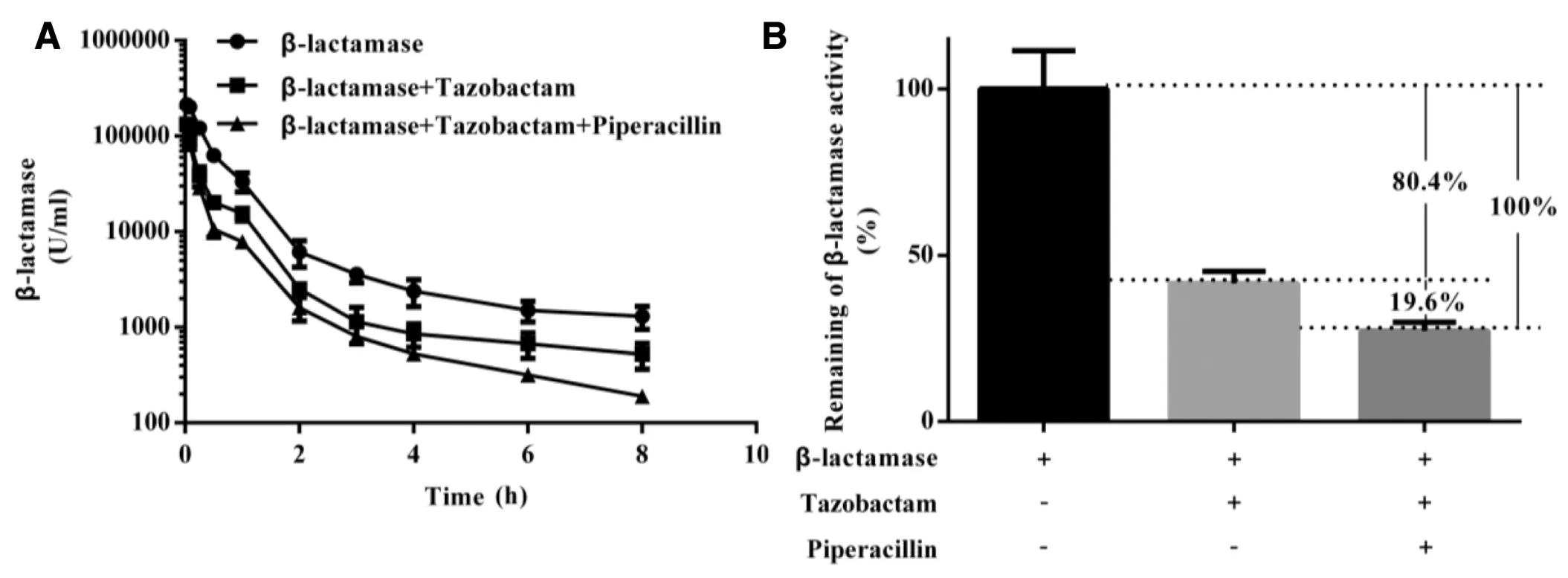
Fig.9-(A)Mean activity-time curves of β-lactamase after intravenous administration of β-lactamase with piperacillin and/or tazobactam.(B)Contribution rates of rOat1/3 to the inhibitory effect of tazobactam on β-lactamase(n=6).
4.Conclusions
Our results provide novel information for demonstrating that the transporters rOat1/3 also mediated the drug interaction between piperacillin and tazobactam.The target organ of DDI mediated by rOat1/3 between piperacillin and tazobactam was the kidney.Piperacillin could enhance the inhibitory effects of tazobactam onβlactamases by inhibiting rOat1/3.The contribution rate of rOat1/3 for the synergistic effect was 20%based on our results.
Conflicts of interest
The authors report no conflicts of interest.The authors alone are responsible for the content and writing of this article.
Funding
This work was supported by the National Natural Science Foundation of China(Nos.81874324,81473280,U1608283,81603186).
 Asian Journal of Pharmacentical Sciences2019年6期
Asian Journal of Pharmacentical Sciences2019年6期
- Asian Journal of Pharmacentical Sciences的其它文章
- Cancer nanotechnology:Enhancing tumor cell response to chemotherapy for hepatocellular carcinoma therapy
- The functions and applications of A7R in anti-angiogenic therapy,imaging and drug delivery systems
- Investigation of molecular aggregation mechanism of glipizide/cyclodextrin complexation by combined experimental and molecular modeling approaches
- Evaluation of the Mrp2-mediated flavonoid-drug interaction potential of quercetin in rats and in vitro models
- A novel oral prodrug-targeting transporter MCT 1:5-fluorouracil-dicarboxylate monoester conjugates
- Synthesis,characterization and in vivo evaluation of honokiol bisphosphate prodrugs protects against rats’brain ischemia-reperfusion injury
