What factors influence patient experience in orthopedic oncology office visits?
Alan T Blank, Sara Shaw, Connor J Wakefield, Yue Zhang, Wei J Liu, Kevin B Jones, R Lor Randall
Abstract
Key words: Press Ganey® survey; Orthopedic oncology; Outpatient clinic; Patient experience; Patient satisfaction; Patient reported outcomes
INTRODUCTION
Patient satisfaction and patient reported outcomes are becoming increasingly important in determining the efficacy of clinical care. For decades in the orthopedic oncology literature, overall survival, metastasis and local recurrence statistics have been well published[1-4]. Using these metrics, patients were determined to be doing well if they were alive, free of local or metastatic disease at various time points.Assessment of patient functional outcomes has been evaluated using scoring systems such as the musculoskeletal tumor society score and Toronto extremity salvage score.However, not until more recently have physicians begun to evaluate various functional, pain related, and psychological outcomes[5-8]. Since this recent interest, the literature has shown that using these metrics can provide valuable information regarding how patients are functioning on a physical and psychological level while being treated as well as during surveillance.
Overall patient satisfaction scores and patient reported outcomes are challenging measurements to understand[9-11]. Each patient has a unique personality as well as pathology and these can both affect patient satisfaction scores. There has been some conflicting data published studying the subject of how patient satisfaction correlates to efficacy of clinical care. Some studies have found positive correlations to efficacy of care and others have found the opposite[9,12]. Understanding the patient perspective certainly provides the care team insight regarding the patients' perceived strengths and weaknesses of care. Furthermore, patient satisfaction scores may in part determine the future of hospital and physician reimbursements[13]. Press Ganey®medical practice outpatient and ambulatory surgery patient experience of care survey(“Press Ganey survey”) is a questionnaire used to evaluate patient satisfaction in the outpatient clinic setting. The number of cancer patients and cancer related costs in the United States is significant and rises every year, hence we feel this is an important demographic to further investigate[14]. In this study, our group evaluated prospectively collected survey information to determine what factors contributed to patients’ likelihood to recommend our practice as well as our providers in our orthopedic oncology outpatient clinic. The study also aimed to identify areas of our clinical practice that were rated highly and those that needed improvement from the patient perspective.
Patient satisfaction surveys have the capacity to provide the orthopedic care team with a window into the perspective of the patient. Although it is unclear whether patient satisfaction scores are directly or indirectly related to efficacy of care this information provides insight to the care team and can help to implement reasonable and necessary changes. The Press Ganey survey is a questionnaire used in the outpatient setting to gather this information from the patient perspective. No study to date has evaluated which factors within the Press Ganey survey are most valued by orthopedic oncology patients. Further, no study to date has reviewed Press Ganey survey results from an orthopedic oncology practice outpatient setting in order to determine practice strengths and weaknesses. We feel the results of this study can provide valuable information about the patient perspective in a clinic setting which can be useful for not just orthopedic oncology clinics but all orthopedic outpatient clinics.
MATERIALS AND METHODS
Patients and methods
We performed an IRB approved retrospective review of prospectively collected Press Ganey survey data from our orthopedic oncology outpatient clinic. The Press Ganey survey was distributed electronically to all patients seen in the outpatient orthopedic oncology clinic. The Press Ganey survey consists of 37 questions involving the clinical check-in process, facility quality, ease of communication with clinic staff, surgical educational information, and overall patient experience. The full survey takes approximately 15 min to complete. Computer adaptive versions are available which shorten the survey to 5-10 questions and allow for completion in as little as 5 min.Patients have 30 d from their clinic encounter to complete the questionnaire. Data was collected during the 2015 and 2016 calendar year. One hundred sixty-two completed the Press Ganey surveys from the outpatient orthopedic oncology clinic and responses were prospectively collected in order to retrospectively review. Basic demographic data along with survey category responses were collected.
Statistical analysis
Data was recorded electronically and obtained in accordance with the medical center’s IRB protocol. The data was then submitted to the University Study Design and Biostatistics Center for statistical evaluation. Frequency and percent were presented for all categorical variables as well as for outcome variables "likelihood to recommend the physician" and "likelihood to recommend the practice". Analysis of variance was applied continuous variables andχ2-test/Fisher’s exact test was applied to assess between categorical variables. All bivariate analyses were two-tailed and the statistical significance was set asP< 0.05. Firth logistic regression analyses were performed using least absolute shrinkage and selection operator (LASSO) to identify predictive factors for each outcome of interest.
Due to the low frequencies of some answers in the survey all original variables with results-0, 25, 50, 75, 100 and N/A were re-categorized as not completely satisfied(0/25/50/75), completely satisfied (100) and N/A.
Descriptive and bivariate analyses were based on the analysis data set composed by every patient’s first record. Mean, standard deviation, median, minimum and maximum were presented for numeric variables. Frequency and percent were presented for categorical variables in overall, and by outcome variables "likelihood to recommend the physician" and "likelihood to recommend the practice". Analysis of variance was applied to assess the possible difference in mean of continuous variable with approximately normal distribution among groups specified by outcome variable.χ2-test or Fisher’s exact test was applied to assess the possible association between two categorical variables. All bivariate analyses were two-tailed and the statistical significance was set asP< 0.05.
Based on results from previous steps and nature of the data (e.g., rare events and quasi-complete separation), Firth logistic regression analyses were performed using LASSO to identify predictive factors truly informative for each outcome of interest,and the final model for each outcome was determined based on the optimal tuning parameter adopting 10 fold cross-validation criteria. The final models were unpenalized; odds ratios and 95% confidence intervals were reported.
Statistical software was SAS 9.4 (SAS Institute Inc., Cary, NC, United States) and R(www.r-project.org). All LASSO analyses were conducted using the “glmnet” package in R. All statistical methods were reviewed by Yue Zhang and Wei J Liu from the University of Utah.
RESULTS
Among the 162 participants, regarding patient’s characteristics, the average age was 54.4 years (standard deviation = 16.2 years, median = 56 years, range = 17 to 95 years);83 (51.2%) participants were female; 104 (64.2%) participants were from in-state; 89(54.9%) participants had malignant diagnosis.
Regarding the outcomes “likelihood to recommend the physician/likelihood to recommend the practice” and patient’s characteristics, it was statistically significant on bivariate analysis that participants who lived out of state were more likely to have complete satisfaction of “likelihood to recommend the physician/likelihood to recommend the practice” compared to participants who lived in state (91.4%vs73.1%,P= 0.027; 86.2%vs69.2%,P= 0.029,χ2-test); among other patient characteristics, there were no statistically significant relationships observed (P> 0.02,P> 0.05 in all instances, ANOVA,χ2-test or Fisher’s exact test).
Regarding outcomes “likelihood to recommend the physician/likelihood to recommend the practice” and individual question responses, it was statistically significant on bivariate analysis that, for each item participants reported “Completely satisfied” they were more likely to have complete satisfaction of “likelihood to recommend the physician” compared to participants who reported “Not completely satisfied” (P< 0.004,P< 0.001 in all instances,χ2-test or Fisher’s exact test). The outcome “likelihood to recommend the physician/likelihood to recommend the practice” was statistically associated with each individual survey question answered on bivariate analysis (P< 0.01,P< 0.001 in all instances, Fisher’s exact test).
Regarding the model of “likelihood to recommend the physician”, Firth logistic regression analysis (with LASSO regulation) results suggested that complete satisfaction of “likelihood to recommend the physician” was positively associated with complete satisfaction of factors including MD friendliness/courtesy (OR = 14.4,95%CI: 2.5-84.3), MD confidence (OR = 48.2, 95%CI: 6.2-376.5), MD instructions follow up care (OR = 2.5, 95%CI: 0.4-7.4), sensitivity to needs (OR = 16.1 , 95%CI: 1-62.5)(Table 1).
Regarding model of “likelihood to recommend the practice”, Firth logistic regression analysis (with LASSO regulation) results suggested that complete satisfaction of “likelihood to recommend the practice” was positively associated with complete satisfaction of factors including MD confidence (OR = 11.6, 95%CI: 2.1-63.4),sensitivity to needs (OR = 5.8, 95%CI: 1.3-26.7), staff work together (OR = 36.1, 95%CI:7.9-165.1) (Table 1).
DISCUSSION
Disease related outcomes have been the gold standard in outcomes measures when discussing oncology patients for many years. Indeed, knowing local recurrence,metastasis and overall survival rates are crucial in understanding the efficacy of treatments. However, functional outcomes and patient reported outcomes also have critical roles in better describing how patients are living after their diagnosis is made and treatment undertaken.
In the orthopedic oncology literature functional outcomes have adapted over time starting with general evaluations such as the SF-36. Functional outcomes then became somewhat more orthopedic based and included tests such as the Harris hip, Oxford knee and DASH scores. From that point, functional evaluations have been developed specifically for orthopedic oncology and include the musculoskeletal tumor society score and Toronto extremity salvage scoring system[1-3]. A relatively new development in patient reported outcomes is the utilization of Patient Reported Outcomes Measurement Information System, which is a simple, computer adaptive test that has been utilized in the oncology literature recently[15-17].
The next progression in evaluating care from the patient perspective comes in the form of patient satisfaction surveys. These surveys, such as Press Ganey, focus on the purely subjective aspect of which aspects of their care they found to be acceptable,and which needed improvement[8,18-20]. There is some debate in the literature as to whether patient satisfaction is positively or negatively correlated with efficacy of care[21,22]. Fentonet al[9]in 2012 published results of a large prospective series and found that higher patient satisfaction was associated with more admissions, more prescription drugs, more overall expenditures and a higher mortality rate. Changet al[7]in 2006 published their results that among a geriatric cohort of 236 patients,assessments of quality of care was not related to global ratings of care. The group recommended against using global ratings of care to be used as a marker of technical quality of care[7]. In the orthopedic literature, Chughtaiet al[18]published their results of a retrospective study involving 736 knee replacement patients and found there was no statistically significant relationship between Press Ganey survey scores and standard arthroplasty outcomes measures.
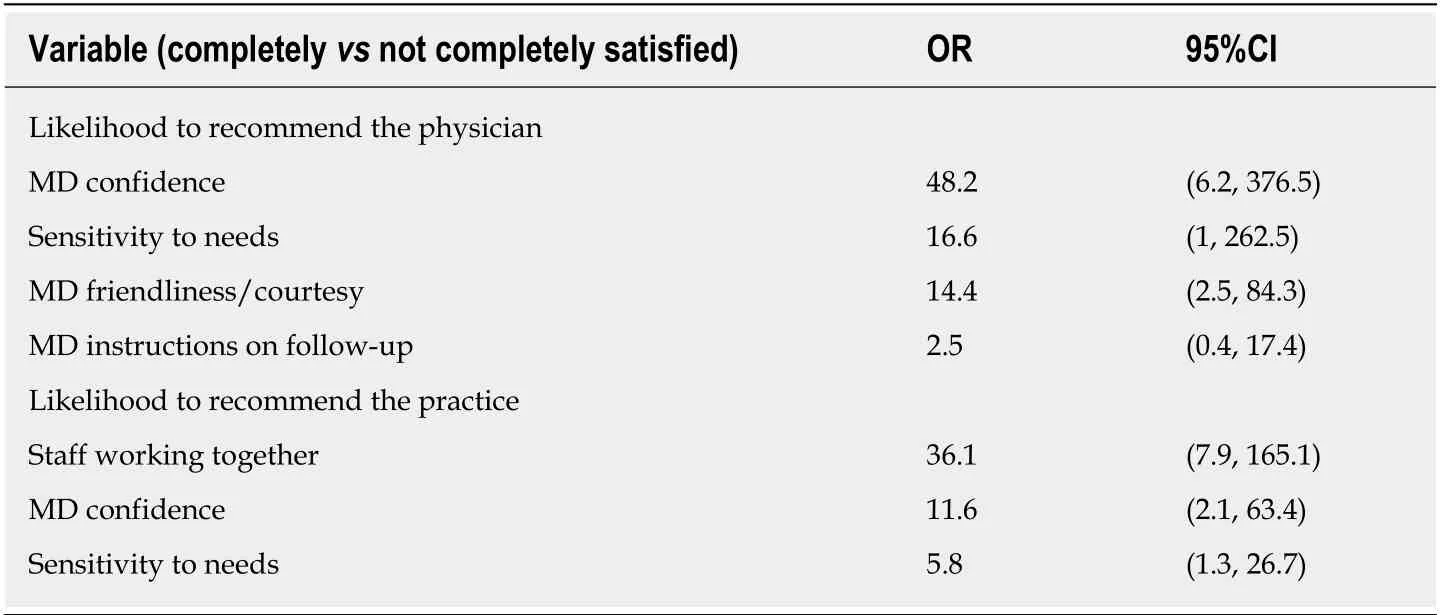
Table 1 Factors for likelihood to recommend physician and practice
Conversely Tsaiet al[12]published in 2015 that among a large cohort of surgical patients, hospitals with higher patient satisfaction provided more efficient care with fewer readmissions and lower mortality rates. Similarly, Sackset al[23]in 2015 published results of a retrospective study of over 100,000 patients and found that patients treated in hospitals which ranked in the highest satisfaction quartile had significantly lower risk of death and minor complications compared to those in the lowest satisfaction quartile.
Regardless of the correlation, important information can be gathered from the survey data collected in this study. In the oncology patient population, we believe that elucidating which factors of the clinic experience are perceived positively and which negatively can help the care team to improve the overall patient experience while not compromising clinical care.
Our study certainly has several limitations including the response rate of 17%overall. Other limitations include the ability of patients to complete surveys up to 30 d after the clinical encounter which may affect patient recall ability. Our clinical practice is quite diverse, with some patients presenting for general orthopedic complaints and a distant history of cancer, and some currently undergoing treatment for sarcoma. We believe that this is in fact the typical patient population for an orthopedic oncology clinic and the heterogeneity increases our external validity. Finally, there is no consensus as to whether patient satisfaction scores are positively or negatively correlated with clinical outcomes. Because of this it is quite difficult to determine if implementing changes based on the outcomes of the satisfaction scores is appropriate in all settings.
The results of this study demonstrate that out-of-state patients may be more likely to be satisfied with their care than inpatients. The group had a difficult time explaining this finding but believes may be related to the fact that our clinical practice has a very wide catchment area and often patients will travel more than 500 miles for care. Those traveling very far are from more rural areas and often have a difficult time finding appropriate physicians for treatment in their hometown, which contributes to their unique perspective.
The data demonstrated that patients perceived our clinic to perform well in the categories of confidence in MD (81%), MD concern about worries/questions (75%),courtesy of staff (76%), MD friendliness/courtesy (79%), cleanliness (75%), MD including you in decision making (72%) and MD explained condition (75%). The clinic showed room for improvement in the categories of ease of getting on the phone (49%),information about delays (36%), wait time (37%) and MD speaking about medications(45%). Our outpatient clinic found this information useful in regards to areas which were satisfactory and which needed improvement and simple measures will be taken to address those insufficiencies while not compromising clinical care.
The data demonstrated that the patients' likelihood to recommend the practice was positively associated with confidence in the physician, sensitivity to their needs and the staff working together. The data also demonstrated that the patients' likelihood to recommend the physician was positively associated with the courtesy of the physician, confidence in the physician, physician instructions on follow up care, and sensitivity to the patients’ needs. These findings are also reasonable categories which patients would find most important and should be considered during every patient interaction.
We believe that by understanding which aspects of patient care are important to the patient, we can continue to improve the patient experience without compromising clinical care. The literature has shown that in some circumstance’s patient reported outcomes may be negatively correlated to clinical outcomes while at other times they are positively associated[9,12]. In both situations, useful information can be obtained from better understanding the patient perspective. The outpatient clinic of study was able to determine which areas of their care were perceived as sufficient and which were insufficient and thus was able to make reasonable and appropriate changes without changing the overall care algorithm. This information may be very useful to orthopedic oncology clinics in addition to the various surgical oncology clinics in the quest to improve on patient experiences in a clinic setting.
ARTICLE HIGHLIGHTS
Research background
Patient satisfaction and reported outcomes play an important role in determining efficacy of clinical care. Little is known about the patient experience in an orthopedic oncology outpatient clinic.
风筝被树丫只是轻轻地缠住,树很高,爬上去弄是不现实的,而如果手用力,只会让风筝扯破。我建议,要不把线剪断吧。
Research motivation
This study aims to evaluate the potential factors that impact the patient experience within an outpatient orthopedic oncology clinic. Identification of these factors will allow us and others to improve the patient experience.
Research objectives
The primary objective of this study was to identify potentially modifiable factors that impact the patient reported experience. With this knowledge one can implement strategies to improve the outpatient experience.
Research methods
This study was a retrospective review of prospectively collected data obtained through routine medical care at a single orthopedic oncology outpatient clinic.
Research results
This study identified that most patients within the practice were from out of state. Likelihood to recommend the attending physician was associated with MD friendliness/courtesy, MD confidence, MD instructions follow-up care, and sensitivity to needs. Although the clinic operation performed well in the categories of courtesy of staff and cleanliness there is room for improvement in ease of getting on the phone, information about delays, and wait time.
Research conclusions
Orthopedic specialties can greatly benefit with the knowledge obtained from this study by understanding which factors are associated the patient experience in an outpatient clinic. Future studies can be aimed at improving areas of care identified from this study.
Research perspectives
The patient experience and reported satisfaction is becoming an important measure of clinical efficacy through various surgical and medical specialties. Little is known on the patient experience within an orthopedic oncology outpatient clinic. Future research is required to investigate strategies at improving areas within the outpatient clinic identified from this study.
 World Journal of Clinical Oncology2020年3期
World Journal of Clinical Oncology2020年3期
- World Journal of Clinical Oncology的其它文章
- Roles of cell fusion, hybridization and polyploid cell formation in cancer metastasis
- Thrombocytopenia with multiple splenic lesions - histiocytic sarcoma of the spleen without splenomegaly: A case report
- Efficacy, patterns of use and cost of Pertuzumab in the treatment of HER2+ metastatic breast cancer in Singapore: The National Cancer Centre Singapore experience
- Assessment methods and services for older people with cancer in the United Kingdom
- Glycoconjugation: An approach to cancer therapeutics
