Effects of intradermal needle therapy plus pinaverium bromide on gastrointestinal hormone levels in irritable bowel syndrome-diarrhea patients
Zhang Xiao-lei(张晓蕾),Gu Hai-yan (谷海燕),Shi Zhi-min (石志敏),Li Xue-qing (李雪青)
1 Tangshan Hospital of Traditional Chinese Medicine,Hebei Province,Tangshan 063000,China
2 Traditional Chinese Medical College,North China University of Science and Technology,Tangshan 063000,China
Abstract
Keywords: Embedding Therapy;Intradermal Needle Therapy; Pinaverium Bromide;Irritable Bowel Syndrome;Diarrhea;Liver-qi Stagnation and Spleen Deficiency;Gastrointestinal Hormones
Irritable bowel syndrome-diarrhea(IBS-D)is a functional intestinal disease, with abdominal pain and loose/watery stool as main symptoms, but in absence of organic alterations.Visceral hypersensitivity,abnormal gastrointestinal motility,brain-gut axis dysfunction and enteric dysbacteriosis are considered as the major causes[1]. Currently, medications used to treat IBS-D mainly include intestinal Ca2+antagonists,intestinal motility regulators, intestinal probiotics and small-dose antidepressants[2]. According to traditional Chinese medicine (TCM), although intestine seems like the only organ affected in IBS-D, the spleen and liver are deeply involved in this condition, and liver-qi stagnation and spleen deficiency is predominant talking about the pathogenesis of IBS-D[3]. Oral Chinese herbal medicine produces certain treatment effect for IBS-D, but people often have problem sticking with it for a long term. As a type of embedding therapy, intradermal needle therapy treats diseases through mild lasting stimulation to acupoints.
In this study,gastrointestinal hormones were observed before and after treatment with intradermal needle therapy plus pinaverium bromide for IBS-D of liver-qi stagnation and spleen deficiency pattern. The report is given as follows.
1 Clinical Materials
1.1 Diagnostic criteria
1.1.1 Diagnostic criteria in Western medicine
RomeⅢ:New Standard for Functional Gastrointestinal Disorders was referred to diagnose IBS-D in the Western medicine model[4].Recurrent abdominal pain or discomforts in the recent three months,at least 3 d in one month;concurrently presented two of the following conditions:① bowel movement >3 times a day;② loose or watery stool;③ felt urgent to go to bathroom or had the sensation of incomplete bowel evacuation; duration ≥6 months.
1.1.2 Diagnostic criteria in TCM
The diagnostic criteria for diarrhea of liver-qi stagnation and spleen-deficiency pattern in theGuiding Principles for Clinical Study of New Chinese Medicines[5]were referred.Primary symptoms:diarrhea with abdominal pain, triggered or worsened by emotional factors, released after bowel movement, with pale red tongue body covered by thin white coating, and wiry pulse; secondary symptoms: chest tightness, belching,and poor appetite.
1.2 Inclusion criteria
Conformed to the above diagnostic criteria in both Western medicine and TCM; 20-65 years old; not on any oral medicine in the previous two weeks, nor received acupuncture treatment; informed consent.
1.3 Exclusion criteria
Functional diarrhea,abdominal pain or bloating;pancreatic diarrhea, infectious diarrhea or hyperthyroid diarrhea; pregnant women or women during lactation;coupled with dysfunction of cardiac or kidney, failure of intestinal, liver or respiratory.
1.4 Statistical methods
The SPSS version 17.0 was adopted for data processing.Measurement data in line with normal distribution and homogeneity of variance were expressed as mean ± standard deviation (±s), with paired samplest-test used for intra-group comparisons,analysis of variance for between-group comparisons,and least significant difference method for pair-wise comparisons. Enumeration data were expressed as rate and examined using Chi-square test.P<0.05 indicated statistical significance.
1.5 General data
This study had been approved by the Ethics Committee of Tangshan Hospital of Traditional Chinese Medicine (No.:TSZYLL2016005).A total of 123 hospitalized patients in Tangshan Hospital of Traditional Chinese Medicine were recruited between August 2017 and May 2019, and allocated to an observation group, a Western medication group and an integrated Western and Chinese medication group by the random number table method, with 41 cases in each group.The basic data were statistically equal acrossthe three groups (allP>0.05),(Table 1).
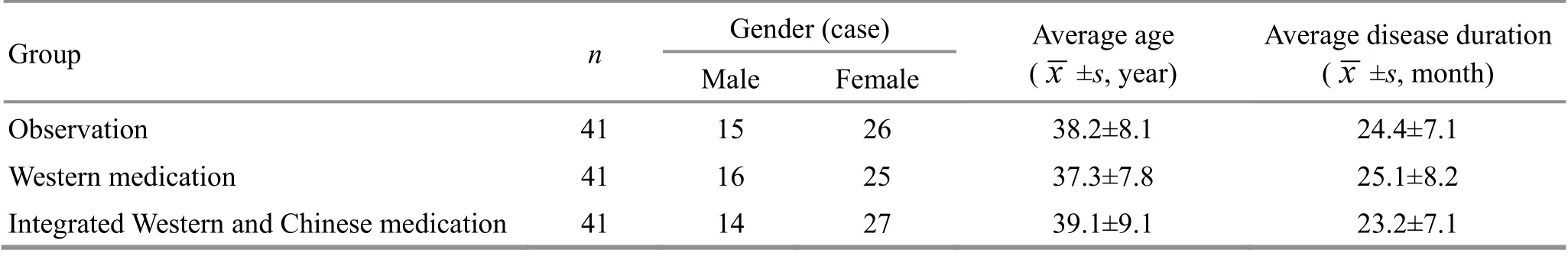
Table 1.Comparison of thegeneral data
2 Treatment Methods
2.1 Observation group
Patients in the observation group received intradermal needle therapy and Western medication.2.1.1 Intradermal needle therapy
Acupoints: Zhongwan (CV 12), Qihai (CV 6), Zusanli(ST 36), Kunlun (BL 60), Taixi (KI 3), Yingu (KI 10), Xiangu(ST 43), Yinlingquan(SP 9),Fuliu(KI 7)and Xingjian(LR 2).
Method: The selected acupoints were firstly sterilized using 75% alcohol before embedded with Seirin intradermal needles (0.20 mm in diameter and 1.2 mm in length). Gently pressed the adhesives to make sure they were fixed well. Pressed and kneaded the needles every 3 h, 1 min each time, and replaced them with new ones every 24 h. For twin acupoints, the two sides were treated alternately;regarding the singleton acupoints, they were treated once every other day. This intervention lasted for 6 weeks.
2.1.2 Western medication
Oral pinaverium bromide tablets(State Food and Drug Administration Approval No.: H20133036, Beijing Wansheng Pharmaceutical Co., Ltd., China), 50 mg/time,3 times a day, before meals. The drug was taken for 6 weeks.
2.2 Western medication group
Patients in the Western medication group received oral pinaverium bromide tablets produced by the same company of the same specification, following the same dosage,administration and duration as in the observation group.
2.3 Integrated Western and Chinese medication group
Patients in the integrated Western and Chinese medication group took Tong Xie Yao Fang decoction in addition to the drug used in the Western medication group. The decoction prescription consisted ofFang Feng(Radix Saposhnikoviae) 10 g,Chen Pi(Pericarpium Citri Reticulatae)15 g,processedBai Shao(Radix Paeoniae Alba) 20 g, and processedBai Zhu(Rhizoma Atractylodis Macrocephalae) 30 g. The herbal decoction was made by the medicine-cooking room of Tangshan Hospital of Traditional Chinese Medicine, 300 mL each dose, one dose a day, which was evenly split into two serves and respectively taken in the morning and at night before mealtime. The Chinese herbal decoction was also taken for 6 weeks.
3 Observation of Therapeutic Efficacy
3.1 Outcome measures
3.1.1 TCM symptoms scores
The TCM symptom grading scale in theGuiding Principles for Clinical Study of New Chinese Medicines[5]was referred to evaluate the severity of the relevant symptoms like diarrhea, abdominal pain, bloating, poor appetite and chest tightness: 0 point, no symptom; 2 points, mild; 4 points, moderate; 6 points, severe.3.1.2 Evaluation of gastrointestinal symptoms
The gastrointestinal symptom (GIS) score was used to score the symptoms such as abdominal pain, bloating,bowel movement frequency, stool form and abnormal bowel movement[6].
Based on the severity, the symptoms were evaluated as no,mild,moderate, severe and extremely severe,and correspondingly scored 1, 2,3, 4, and 5 points.
Based on the frequency,the symptoms were evaluated as no, <1 d per month, 1 d per month, 2-3 d per month, 1 d per week, >1 d per week and every day,and correspondingly scored 0, 1, 2, 3, 4, 5 and 6 points.
GIS score = Mean symptom severity score + Mean symptom frequency score.
3.1.3 IBS symptom severity scale (IBS-SSS)
IBS-SSS estimated five domains including abdominal pain severity, onset time of abdominal pain in 14 d,abdominal pain-associated discomforts,bowel movement satisfaction and quality of life(QOL)influence[7].Each section was scored 0-100 points. A higher score indicated a more severe condition.
3.1.4 QOL
IBS-QOL questionnaire was adopted to evaluate the QOL from the perspectives of dysphoria, health worry,body image, interference with activity, food avoidance,social reaction,sexual and relationship[8].The score ranged from 0 point (worst) to 100 points (best).3.1.5 Serum levels of 5-hydroxytryptamine(5-HT),substance P(SP)and vasoactive intestinal peptide(VIP)
Before and after treatment,5 mL venous blood was collected on empty stomach and then centrifuged to separate the serum.Enzyme-linked immunosorbent assay was used for detection.The kits were purchased from Shanghai Fusheng Industrial Co.,Ltd.,and the detection wasperformed by the laboratory of Tangshan Hospital of Traditional Chinese Medicine.
3.2 Criteria for therapeutic efficacy
The criteria for evaluating the efficacy in treatment of diarrhea in theGuiding Principles for Clinical Study of New Chinese Medicineswere referred[5]. The sum of the scores of TCM symptoms,GIS,IBS-SSS and IBS-QOL was calculated first, based on which the therapeutic efficacy index was then calculated.
Therapeutic efficacy index =(Pre-treatment total score- Post-treatment total score)÷ Pre-treatment totalscore ×100%.
Recovered: Therapeutic efficacy index ≥90%.
Markedly effective:Therapeutic efficacy index ≥60% but <90%.
Effective:Therapeutic efficacy index ≥30% but <60%.
Invalid: Therapeutic efficacy index <30%.
3.3 Results
3.3.1 Comparison of the clinical efficacy
The total effective rate was 92.7% in the observation group,68.3%in the Western medication group and 78.1% in the integrated Western and Chinese medication group.The total effective rate was higher in the observation group than in the other two groups,and higher in the integrated Western medication group than in the Western medication group,and the between-group differences were statistically significant(allP<0.05), (Table 2).
3.3.2 Comparison of the scores of TCM symptoms,GIS and IBS-SSS
Before treatment,there were no significant differences in the scores of TCM symptoms,GIS and IBS-SSSacross the three groups (allP>0.05), suggesting the comparability.After treatment,the scores of TCM symptoms,GIS and IBS-SSS decreased in the three groups(allP<0.05);the three scores were significantly lower in the observation group than in the other two groups (allP<0.05),and lower in the integrated Western and Chinese medication group than in the Western medication group(allP<0.05),(Table 3).
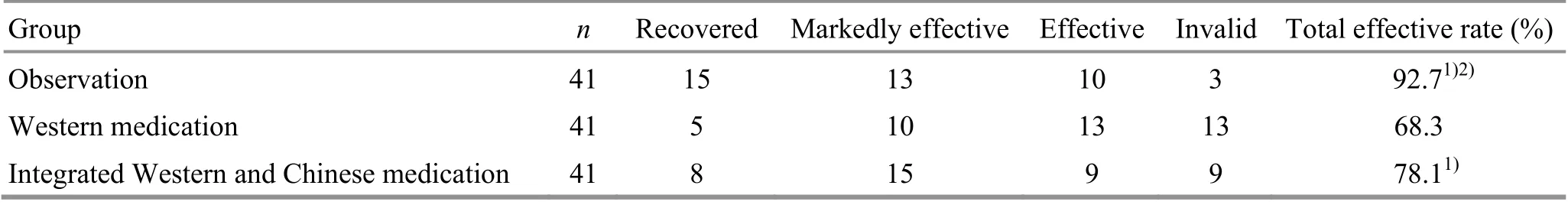
Table 2.Comparison of the clinical efficacy (case)
Table 3.Comparison of the scores of TCM symptoms,GISand IBS-SSS( ±s, point)
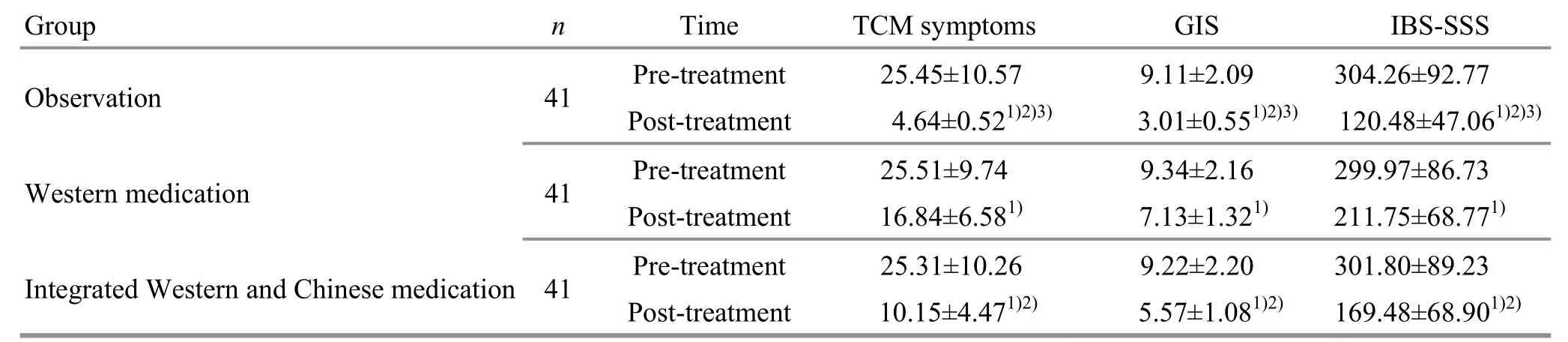
Table 3.Comparison of the scores of TCM symptoms,GISand IBS-SSS( ±s, point)
Note:Compared with the same group before treatment,1) P<0.05;compared with the Western medication group after treatment,2) P<0.05;compared with the integrated Western and Chinese medication group after treatment,3) P<0.05
Group n Time TCM symptoms GIS IBS-SSS Observation 41 Pre-treatment 25.45±10.57 9.11±2.09 304.26±92.77 Post-treatment 4.64±0.521)2)3)3.01±0.551)2)3)120.48±47.061)2)3)Western medication 41 Pre-treatment 25.51±9.74 9.34±2.16 299.97±86.73 Post-treatment 16.84±6.581) 7.13±1.321) 211.75±68.771)Integrated Western and Chinesemedication 41 Pre-treatment 25.31±10.26 9.22±2.20 301.80±89.23 Post-treatment 10.15±4.471)2) 5.57±1.081)2) 169.48±68.901)2)
3.3.3 Comparison of the IBS-QOL score
Before treatment,there were no significant differences in the eight component scores of IBS-QOL across the three groups (allP>0.05),indicating the comparability.After treatment,the eight component scores of IBS-QOL increased significantly in the three groups (allP<0.05);the eight component scores were significantly higher in the observation group than in the other two groups (allP<0.05),and higher in the integrated Western and Chinese medication group than in the Western medication group(allP<0.05), (Table 4).SPand VIP decreased markedly in the three groups (allP<0.05);the serum levels of 5-HT,SP and VIP were significantly lower in the observation group than in the other two groups(allP<0.05),and lower in the integrated Western and Chinese medication group than in the Western medication group(allP<0.05), (Table 5).
3.3.4 Comparisons of the serum levels of 5-HT, SP and VIP
Before treatment,there were no significant differences in the serum levels of 5-HT,SP and VIP across the three groups(allP>0.05),suggesting the comparability.After treatment,the serum levels of 5-HT,
Table 4.Comparison of the IBS-QOL score( ±s,point)
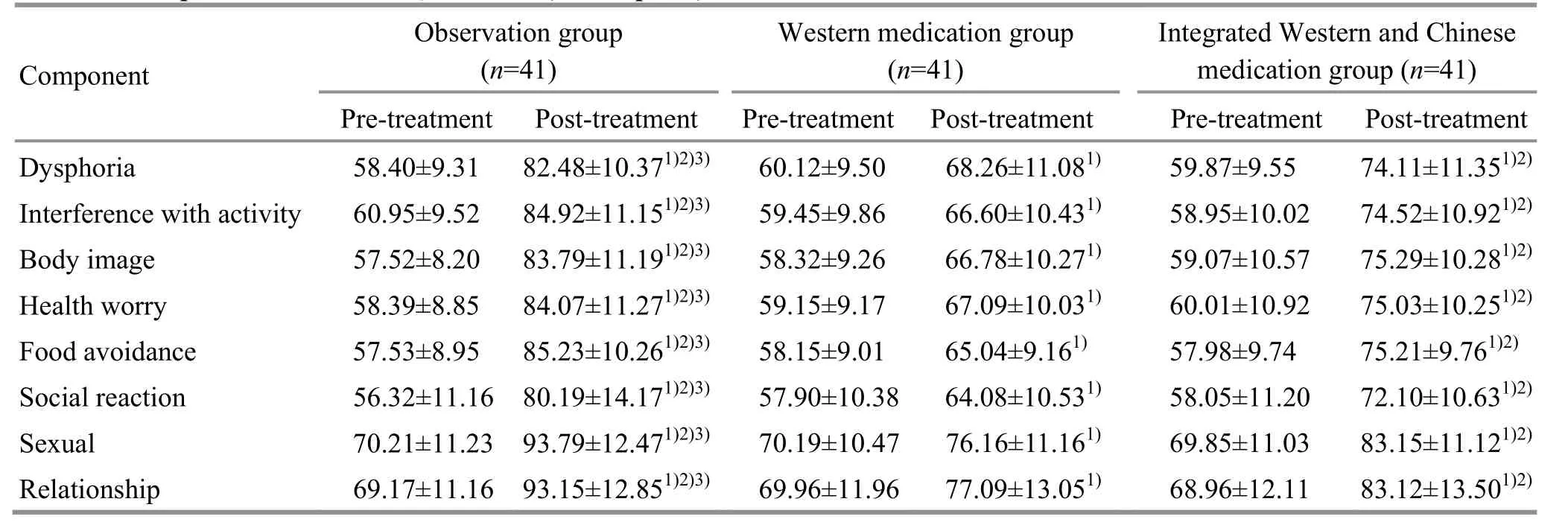
Table 4.Comparison of the IBS-QOL score( ±s,point)
Note:Compared with the same group before treatment,1) P<0.05;compared with the Western medication group after treatment,2) P<0.05;compared with the integrated Western and Chinese medication group after treatment,3) P<0.05
Integrated Western and Chinese medication group(n=41)Pre-treatment Post-treatment 59.87±9.55 74.11±11.351)2) 58.95±10.02 74.52±10.921)2) 59.07±10.57 75.29±10.281)2) 60.01±10.92 75.03±10.251)2) 57.98±9.74 75.21±9.761)2) 58.05±11.20 72.10±10.631)2) 69.85±11.03 83.15±11.121)2) 68.96±12.11 83.12±13.501)2)
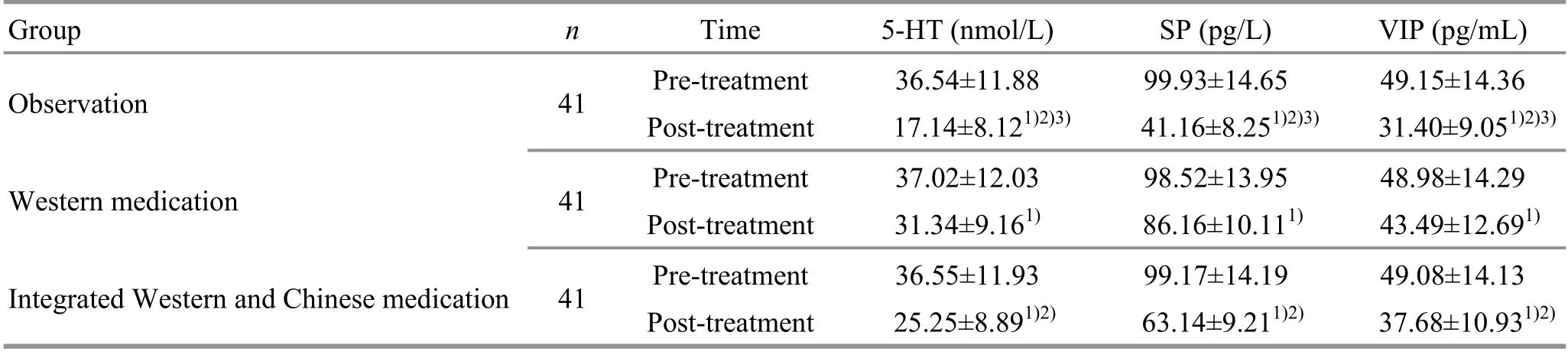
Table 5.Comparison of the serum levels of 5-HT, SP and VIP
4 Discussion
Gastrointestinal symptoms are typical manifestation in a functional gastrointestinal disorder like IBS-D[9].Therefore, this study took gastrointestinal symptoms,TCM symptoms and QOL as the target items to evaluate the clinical efficacy.
In the observation group,patients were provided with intradermal needle therapy plus pinaverium bromide tablets,with the sole use of pinaverium bromide and the combined use of pinaverium bromide and Tong Xie Yao Fang as the controls. After 6-week treatment,the total effective rate was estimated at 92.7% in the observation group,significantly higher than that in the other two groups, while the integrated Western and Chinese medication group was superior to the Western medication group.Moreover,the observation group also presented notable advantages regarding the improvements in the gastrointestinal symptoms, TCM symptoms, QOL and serum levels of 5-HT, SP and VIP compared with the other two groups.Besides,the integrated Western and Chinese medication group won out the Western medication group comparing the above items.
Pinaverium bromide has been primarily used to treat IBS-D in the Western medicine model. Although this drug can release abdominal pain and diarrhea caused by intestinal dysfunction[10], it misses the root cause of IBS-D and doesn’t perform well in improving the non-intestinal symptoms and QOL.IBS-D belongs to ‘diarrhea’ or ‘painful diarrhea’ in TCM, manifesting both abdominal pain and diarrhea.Liver-qi stagnation,spleen deficiency and excessive dampness are believed to be the major pathogenic factors. Oral administration of Tong Xie Yao Fang has been proved effective in mitigating the typical symptoms of IBS-D, i.e. abdominal pain coming with strong need to run to bathroom and immediate release of the abdominal pain afterwards[11],thus it can produce certain positive effects on the clinicalsymptomsand QOL in IBS-Dpatients.
Shen Ying Jing(Miraculous Effective Classic of Acupuncture)is a TCM classic created in Ming Dynasty.It records 15 acupoints specifically for abdominal pain.Ten out of the 15 acupoints were selected in this study,i.e.Zhongwan(CV 12),Qihai(CV 6),Zusanli(ST 36),Kunlun(BL 60),Taixi(KI3),Yingu(KI 10),Xiangu (ST 43),Yinlingquan(SP 9),Fuliu(KI 7)and Xingjian(LR 2).Kunlun(BL 60)acts to reinforce the spleen and kidney.Fuliu(KI7)is the Jing-River point of the Kidney Meridian,Taixi(KI 3)is the Yuan-Primary point of the Kidney Meridian,and Yingu (KI 10)is the He-Sea point of the Kidney Meridian.These three points were used together to warm yang and promote diuresis[12].A study showed that acupuncture at Taixi(KI 3),Yingu(KI 10)and Fuliu(KI 7)can improve the bowel movement frequency and stool form in chronic diarrhea patients[13].Yinlingquan(SP 9)is the He-Sea point of the Spleen Meridian and acts to fortify the spleen and percolate dampness. It showed that acupuncture at Yinlingquan(SP 9)can regulate intestinal peristalsis and help manage the chronic diarrhea symptoms[14].Zhongwan(CV 12)and Qihai(CV 6)work to fortify the spleen and supplement qi,strengthen the body resistance and eliminate pathogenic factors[15].Xiangu(ST 43),the Shu-Stream point of the Stomach Meridian,and Zusanli(ST 36),the He-Sea point of the Stomach Meridian, can tonify the spleen and regulate qi movement[16].Applying moxibustion to Xiangu(ST 43)and Zusanli(ST 36)has been found effective in releasing abdominal pain[17].As the Ying-Spring point of the Liver Meridian,Xingjian(LR 2)functions to relieve the stagnated liver qi.Acupuncture at Xingjian(LR 2)can regulate qi and soothe the stomach to mitigate abdominal pain[18].The ten points together made a joint effort to fortify the spleen,supplement qi and regulate qimovement, and eliminate dampness.The sustained stimulation produced by intradermal needles causes both physical and chemical changes at the acupoints;meanwhile,the meridian system passes the information of these changes into the body to treat diseases[19].Intradermal needle therapy only causes mild pain and thus can be well accepted by patients,and its persistent stimulation is supposed to better trigger the function of the acupoints[20].
To sum up, the combined use of intradermal needle therapy and pinaverium bromide can significantly improve the gastrointestinal symptoms and QOL in IBS-D patients,producing satisfying clinical efficacy,which may be associated with its regulation effect on gastrointestinalhormones.
Conflict of Interest
The authors declare that there is no potential conflict of interest in thisarticle.
Acknowledgments
This work was sponsored by 2016 Medical Alliance Clinical Research Project of Dongzhimen Hospital,Beijing University of Chinese Medicine (2016年度北京中医药大学东直门医院医疗联盟临床研究专项资助项目,No.2016YLLM01).
Statement of Informed Consent
Informed consent was obtained from all individual participantsin thisstudy.
Received:15 November 2019/Accepted:24 February 2020
 Journal of Acupuncture and Tuina Science2020年6期
Journal of Acupuncture and Tuina Science2020年6期
- Journal of Acupuncture and Tuina Science的其它文章
- The role of microglia in thalamic reticular nucleus in acupuncture regulating cognitive deficits in insomnia rats
- Study on the acupoints belonging to the three yin meridians of foot reflecting the variation pattern of uterine qi and blood in women with moderate constitution
- Effects of electroacupuncture on uterine prostaglandin F2α, cyclooxygenase 2 and nuclear factor κB in rats with primary dysmenorrhea
- Effect of moxibustion at sensitized-acupoints on quality of life in patients with chronic superficial gastritis
- Research advances in the brain mechanisms of acupuncture effects based on the BOLD-fMRI technology
- Clinical observation on acupoint massage plus Vitalstim electrical stimulation for deglutition disorder after stroke
