血液灌流联合不同血液透析模式改善尿毒症患者严重皮肤瘙痒的疗效对比
薛甜甜 屈花便
【摘要】 目的 對比血液灌流联合不同血液透析模式改善尿毒症患者严重皮肤瘙痒的疗效。
方法 依据随机数表,将2019年3月~2020年2月收治的95例尿毒症患者分为A组(47例)和B组(48例)。两组均采取同型号血透机、灌流器,A组予以血液灌流联合血液透析治疗,B组予以血液灌流联合血液透析滤过治疗,均治疗3个月。于治疗前及治疗3个月时对比两组Ribaha评分、生化指标、炎症指标及血常规指标的变化,并对比两组第一次开始透析时的血压、血清白蛋白、水电解质水平以及尿素清除指数(KT/V)。
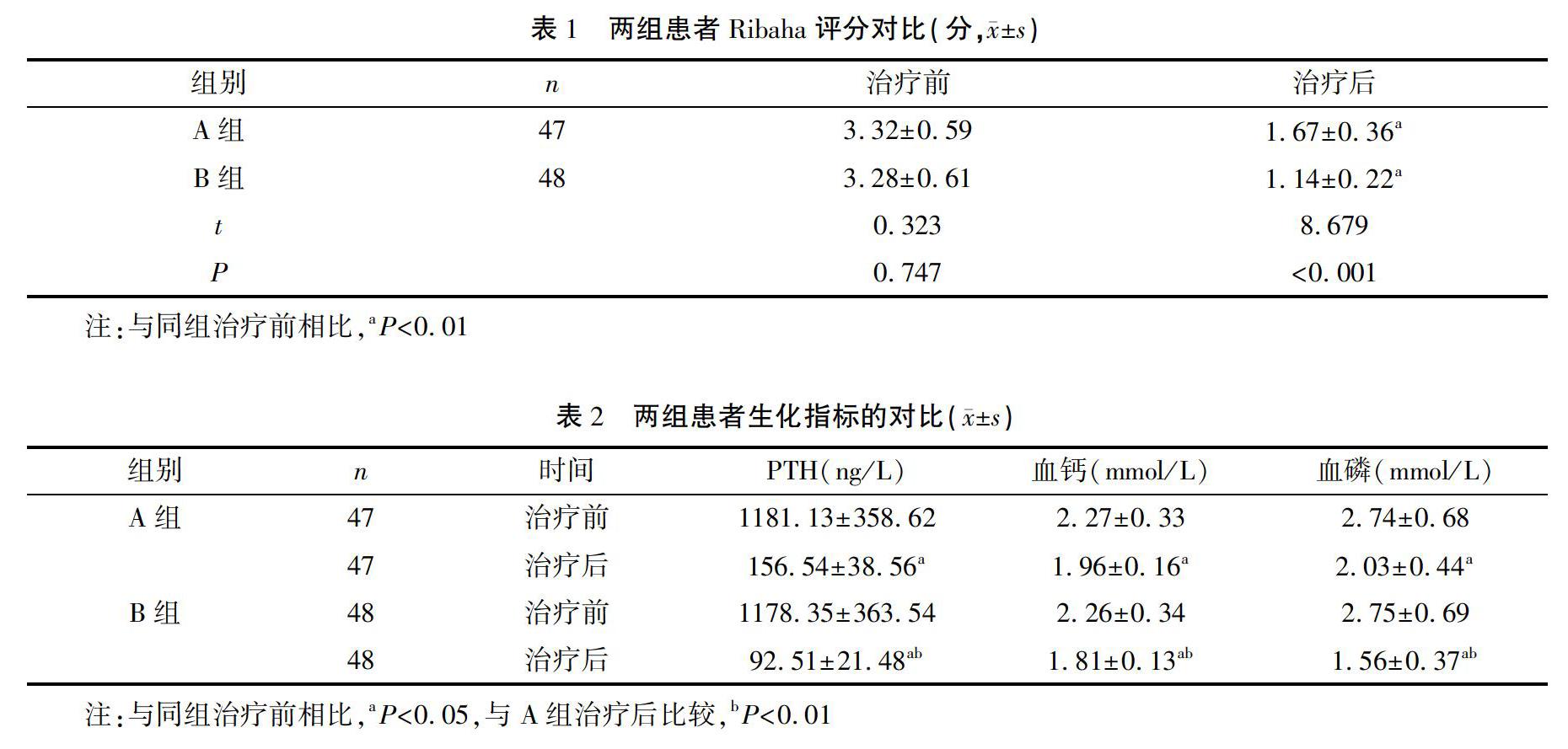
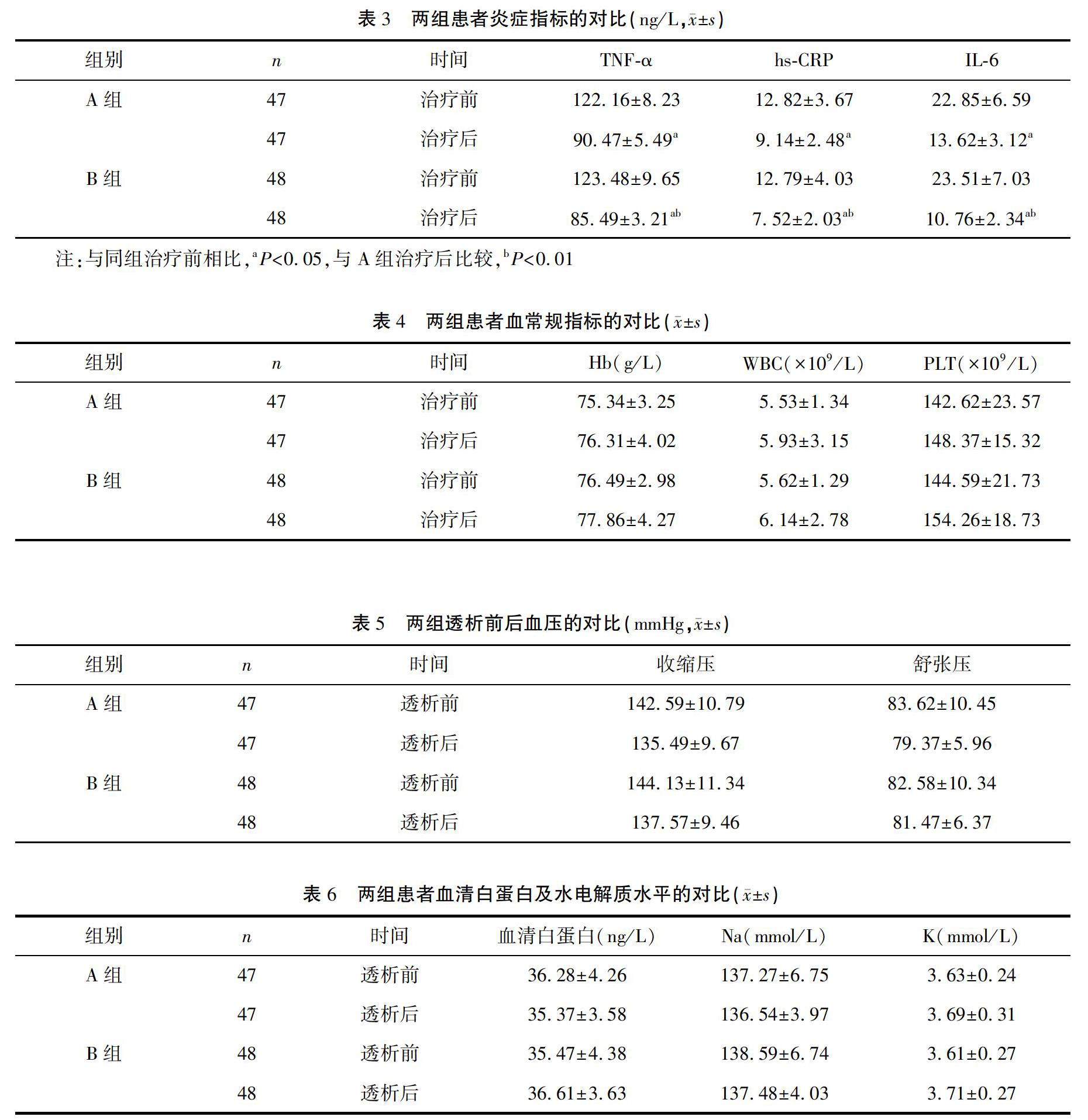
结果 治疗后,B组Ribaha评分低于A组,差异有统计学意义(P<0.001);B组甲状旁腺激素(PTH)、血钙及血磷水平均低于A组,差异有统计学意义(P<0.01);两组血清肿瘤坏死因子-α(TNF-α)、超敏C反应蛋白(hs-CRP)和白介素-6(IL-6)水平均较治疗前低,且B组上述指标均低于A组,差异有统计学意义(P<0.01);两组血红蛋白(Hb)、白细胞计数(WBC)及血小板(PLT)与治疗前比较,以及治疗后B组Hb、WBC和PLT与A组比较,差异均无统计学意义(P>0.05);透析后,两组收缩压、舒张压水平与透析前比较,以及透析后B组收缩压、舒张压水平与A组比较,差异均无统计学意义(P>0.05);两组血清白蛋白、钠(Na)和钾(K)水平与治疗前比较,以及B组血清白蛋白、Na和K水平与A组比较,差异均无统计学意义(P>0.05);A组KT/V值为(1.32±0.54),低于B组的(1.61±0.26),差异有统计学意义(t=3.346,P=0.001)。
结论 血液灌流联合血液透析滤过治疗尿毒症患者的效果较好,可有效改善生化指标、炎症反应和皮肤瘙痒情况,且安全性较高。
【关键词】 尿毒症;血液灌流;血液透析;血液透析滤过
中图分类号:R692.5 文献标志码:A DOI:10.3969/j.issn.1003-1383.2020.11.006
【Abstract】 Objective To compare the efficacy of hemoperfusion combined with different hemodialysis models on improving severe skin itching in patients with uremia.
Methods According to random number table, 95 cases of uremic patients treated in our hospital from March 2019 to February 2020 were divided into group A (47 cases) and group B (48 cases). Both groups were treated with the same model of hemodialysis machine and perfusion device. The group A were treated with hemoperfusion combined with hemodialysis, and the group B were treated with hemoperfusion combined with hemodiafiltration. Both groups were treated for 3 months. The changes of Ribaha score, biochemical indexes, inflammation indexes and blood routine indexes of the two groups were compared before treatment and at 3 months of treatment, and the blood pressure, serum albumin, water electrolyte levels, and urea clearance indexes (KT/V) were compared between the two groups at their first time of dialysis.
Results After treatment, the Ribaha score of the group B was lower than that of the group A, difference was statistically significant (P<0.001); the levels of parathyroid hormone (PTH), blood calcium and blood phosphorus in the group B were all lower than those of the group A, and difference was statistically significant (P<0.01); the levels of serum tumor necrosis factor-α (TNF-α), high-sensitivity C-reactive protein (hs-CRP) and interleukin-6 (IL-6) in the two groups were lower than those before treatment, and the above-mentioned indicators in the group B were all lower than those of the group A, and the difference was statistically significant (P<0.01); there was no statistically significant difference in hemoglobin (Hb), white blood cell count (WBC) and platelet (PLT) between the two groups before and after treatment, and between the group B and the group A after treatment (P>0.05). After dialysis, there was no statistically significant difference in systolic blood pressure and diastolic blood pressure between the two groups before and after dialysis, and between the group B and the group A after dialysis (P>0.05); there was no statistically significant difference in serum albumin, Na and K levels between the two groups and before treatment, and between the group B and the group A after dialysis (P>0.05); the KT/V value of the group A was (1.32±0.54), which was lower than that of the group B (1.61±0.26), and the difference was statistically significant (t=3.346, P=0.001).
2.3 两组炎症指标的比较
治疗前,两组血清TNF-α、hs-CRP和IL-6水平相比,差异无统计学意义(P>0.05);治疗后,两组血清TNF-α、hs-CRP和IL-6水平均较治疗前低,且B组上述指标均低于A组,差异有统计学意义(P<0.01)。见表3。
2.4 两组血常规指标的比较
治疗前,两组Hb、WBC和PLT比较,差异无统计学意义(P>0.05);治疗后,两组Hb、WBC和PLT与治疗前比较,差异无统计学意义(P>0.05),B组Hb、WBC和PLT与A组比较,差异无统计学意义(P>0.05)。见表4。
2.5 两组血压的比较
透析前,两组收缩压、舒张压水平比较,差异无统计学意义(P>0.05);透析后,两组收缩压、舒张压水平与透析前比较,差异无统计学意义(P>0.05),B组收缩压、舒张压水平与A组比较,差异无统计学意义(P>0.05)。见表5。
2.6 两组血清白蛋白及水电解质水平比较
透析前,两组血清白蛋白、Na和K水平相比,差异无统计学意义(P>0.05);透析后,两组血清白蛋白、Na和K水平与治疗前比较,差异无统计学意义(P>0.05),B组血清白蛋白、Na和K水平与A组比较,差异无统计学意义(P>0.05)。见表6。
2.7 两组尿素清除率的比较
A组KT/V值为(1.32±0.54),低于B组的(1.61±0.26),差异有统计学意义(t=3.346,P=0.001)。
3 讨 论
尿毒症是慢性肾衰竭终末期的综合征,在此阶段肾脏的排泄功能下降,人体代谢的酸性产物无法正常排出,体内会出现血钙、血磷偏高,从而刺激PTH分泌急剧增加,血钙和血磷代谢废物异常增多,产生大量的毒性物质,淤积在身体各个部位[5~6]。同时,毒物沉积在刺激神经末梢的外周血管中会引起神经细胞变性,引发皮肤瘙痒,严重会使患者难以忍受[7]。临床常采取血液灌流治疗尿毒症患者,将血流引入灌流器中,通过固态吸附剂发挥吸附作用,清除内源性或外源性大分子毒性物质和产生的代谢物质,具有吸附率高、无脱落、无外源更安全的特点[8~9]。但该治疗方式对小分子物质清除不足,且不能调节水、电解质、酸碱平衡,故临床常以血液灌流联合血流透析对毒性物质进行彻底清除,但哪种血液透析方式联合血液灌流治疗该病疗效更好成为临床关注重点。
PTH为中大分子毒素,其水平升高可导致甲状旁腺功能亢进性骨病,形成骨营养不良,加重尿毒症患者病情[10]。本研究结果显示,治疗后,两组Ribaha评分均低于治疗前,且B组Ribaha评分低于A组;两组PTH、血钙和血磷水平均较治疗前低,且B组上述指标均低于A组;两组血清TNF-α、hs-CRP和IL-6水平均较治疗前低,且B组上述指标均低于A组,提示血液灌流联合血液透析滤过治疗尿毒症患者的疗效确切,可有效降低生化指标,改善皮肤瘙痒症状。分析原因在于,血液透析是一种血液净化技术,能把血液从体内引出体外,通过对流、吸附及超滤等原理将体内代谢废物和多余水分去除,并在治疗期间保持酸碱和电解质平衡[11~12]。同时该治疗方式对小分子的毒素清除效果较好,且对毒素和水分清除也较快,但对中分子毒素清除不足,并会诱导新的毒素生成和造成血流动力学异常,容易引起心血管并发症,增加患者病死的风险[13]。而血液透析滤过则是将血液透析和血液滤过的优点结合,能有效清除中小分子尿毒症毒素,且在治疗过程中能够稳定患者的血流动力学状态,并有效清除中分子PTH,有利于骨病的控制,还能促进PTH调节血钙和血磷代谢[14]。同时,与血液灌流联合使用可有效清除大分子毒素和代谢废物,减少毒性物质淤积,改善患者皮肤瘙痒症状[15]。此外,本研究还发现,两组血常规指标、血压、血清白蛋白及水电解质水平均与治疗前无明显变化,而B组KT/V值高于A组,说明两种透析方案均不会对血细胞、血小板的产生造成破坏,同时也不会引起低血压、水解质失衡,具有较高的安全性,且以血液灌流联合血液透析滤过的透析治疗效率较好。
综上所述,尿毒症患者采用血液灌流联合血液透析滤过治疗的效果确切,可有效降低生化指标及炎症指标各项水平,改善皮肤瘙痒,且治疗期间不会引起血常规、血压及水电解质异常,具有较高的安全性。
参 考 文 献
[1] 聂艳芳,万晓晴,陈媛,等.不同透析频率及方式治疗慢性肾功能衰竭尿毒症的临床效果比较[J].中国基层医药,2019,26(18):2252-2256.
[2] 吴艳,李永超,钟杰.不同血液净化方式对尿毒症患者瘙痒症状改善及中、大分子毒素清除的影响[J].实用医院临床杂志,2018,15(6):211-213.
[3] 王蔚文,湖南省医院协会.临床疾病诊断与疗效判断标准[M].北京:科学技术文献出版社,2010:261-262.
[4] LJOSAA T M,STUBHAUG A,MORK C,et al.Improvement in Psoriasis Area and Severity Index score predicts improvement in skin pain over time in patients with psoriasis[J].Acta Derm Venereol,2013,93(3):330-334.
[5] 陳宗英,谢席胜.尿毒症性皮肤瘙痒研究现状[J].中国中西医结合肾病杂志,2017,18(9):841-843.
[6] 刘秀需.血液透析联合血液灌流治疗尿毒症皮肤瘙痒的疗效观察[J].浙江临床医学,2016,18(9):1661-1662.
[7] 钟广芝,邢天柱.不同血液净化模式对尿毒症患者皮肤瘙痒及生活质量的影响[J].临床肾脏病杂志,2016,16(4):236-239.
[8] 宋培.血液灌流联合血液透析对尿毒症患者肾功能 及T淋巴细胞水平的影响[J].河北医学,2019,25(8):1253-1257.
[9] 陈昕,张莹.血液透析联合血液灌流对尿毒症患者毒素清除率、炎性因子、钙磷代谢及免疫功能的影响[J].陕西医学杂志,2019,48(6):770-773.
[10] 陈璐.血液灌流联合血液透析治疗对尿毒症患者血清β2-MG、PTH水平及预后的影响[J].热带医学杂志,2018,18(2):225-228.
[11] 陈璐,李新华,王莎莎.尿毒症维持性血液透析患者短期生存影响因素分析[J].中国中西医结合肾病杂志,2019,20(10):885-887.
[12] 郭博慧,李向东,李毅,等.每日血液透析对尿毒症患者透析诱导期、血液生化指标及SCL-90评分的影响[J].中国输血杂志,2019,32(3):260-263.
[13] 焦占峰,张宜明,马小芬,等.血液透析滤过对改善尿毒症患者周围神经病变的临床疗效观察[J].中国血液净化,2019,18(7):491-494.
[14] 郑海瑞,贾卫国,王国强,等.不同透析方法对尿毒症患者钙磷代谢及PTH水平的影响[J].西南国防医药,2019,29(5):608-610.
[15] 崔益鸿,黄路路.血液灌流联合血液透析滤过对尿毒症患者不良症状及生化指标的影响[J].中国临床研究,2017,30(9):1204-1206.
(收稿日期:2020-06-30 修回日期:2020-09-07)
(编辑:梁明佩)

