MicroRNAs in laser-induced choroidal neovascularization in mice and rats: their expression and potential therapeutic targets
Bridget Martinez , Philip V. Peplow
Abstract Choroidal neovascularization characterizes wet age-related macular degeneration.Choroidal neovascularization formation involves a primarily angiogenic process that is combined with both inflammation and proteolysis. A primary cause of choroidal neovascularization pathogenesis is alterations in pro- and anti-angiogenic factors derived from the retinal pigment epithelium, with vascular endothelium growth factor being mainly responsible for both clinical and experimental choroidal neovascularization. MicroRNAs(miRNAs) which are short, non-coding, endogenous RNA molecules have a major role in regulating various pathological processes, including inflammation and angiogenesis.A review of recent studies with the mouse laser-induced choroidal neovascularization model has shown alterations in miRNA expression in choroidal neovascularization tissues and could be potential therapeutic targets for wet age-related macular degeneration.Upregulation of miR-505 (days 1 and 3 post-laser), miR-155 (day 14) occurred in retina;miR-342-5p (days 3 and 7), miR-126-3p (day 14) in choroid; miR-23a, miR-24, miR-27a(day 7) in retina/choroid; miR-505 (days 1 and 3) in retinal pigment epithelium/choroid;downregulation of miR-155 (days 1 and 3), miR-29a, miR-29b, miR-29c (day 5), miR-93 (day 14), miR-126 (day 14) occurred in retinal pigment epithelium/choroid. Therapies using miRNA mimics or inhibitors were found to decrease choroidal neovascularization lesions.Choroidal neovascularization development was reduced by overexpression of miR-155,miR-188-5p, miR-(5,B,7), miR-126-3p, miR-342-5p, miR-93, miR-126, miR-195a-3p, miR-24, miR-21, miR-31, miR-150, and miR-184, or suppression of miR-505, miR-126-3p, miR-155, and miR-23/27. Further studies are warranted to determine miRNA expression in mouse laser-induced choroidal neovascularization models in order to validate and extend the reported findings. Important experimental variables need to be standardized; these include the strain and age of animals, gender, number and position of laser burns to the eye, laser parameters to induce choroidal neovascularization lesions including wavelength,power, spot size, and duration.
Key Words: age-related macular degeneration; angiogenesis; animal model; blood plasma; choroid; laser; microRNAs; neovascularization; retina; retinal pigment epithelium;therapeutic targets; vascular endothelial growth factor
Introduction
Wet (exudative or neovascular) age-related macular degeneration (AMD) is characterized by choroidal neovascularization (CNV) in which there is abnormal growth of blood vessels from the choroid into the retina (Agrawal and Chaqour, 2014). Wet AMD accounts for only 10% of all AMD cases but is responsible for causing severe loss of central vision in 90% of cases. The abnormal vessels grow from the choriocapillaris and extend through the Bruch’s membrane into the subretinal space. Blood and fluid leakage within the dissrupted tissue causes inflammation and scar formation resulting in retinal damage and detachment (Witmer et al.,2003). The damage to the retina causes central vision loss and eventual loss of sight if untreated (Bhise et al., 2011;Farnoodian et al., 2017).
CNV formation involves a primarily angiogenic process that is combined with both inflammation and proteolysis(Hagerman et al., 2001). A primary cause of CNV pathogenesis is alterations in pro- and anti-angiogenic factors derived from the retinal pigment epithelium (RPE). Proangiogenic factors e.g., vascular endothelium growth factor (VEGF), basic fibroblast growth factor, and platelet-derived growth factor can all increase endothelial cell proliferation in CNV, with VEGF being mainly responsible for both clinical and experimental CNV (Amin et al., 1994; Kvanta et al., 1996; Lopez et al., 1996).An early step in CNV initiation is the disruption or degradation of Bruch’s membrane, allowing proliferating neovascular tissue derived from the choroid to enter the subretinal space and evoke an inflammatory response. Pro- and antiinflammatory cytokines, chemokines, and the complement cascade are also involved in CNV formation. Macrophages play a crucial role in CNV development by releasing multiple inflammatory and angiogenic factors that stimulate monocyte recruitment and endothelial cell proliferation and migration(Grossniklaus et al., 2010). In addition, an imbalance between matrix metalloproteinases and tissue inhibitors influences extracellular matrix degradation and the formation of a fibrin matrix scaffold which are essential for CNV initiation (Carmeliet and Collen, 1998; Steen et al., 1998).
Models of Experimental Choroidal Neovascularization
Three main models of experimental CNV have been described.They are the laser-induced CNV model, the surgically-induced CNV model, and a genetic model of CNV (Liu et al., 2017).Each of these models has advantages and disadvantages(Grossniklaus et al., 2010).
Laser-induced CNV model
The laser-induced CNV model is one of the most used to study the angiogenic aspect of wet AMD. Laser photocoagulation is used to injure the outer retina and disrupt the Bruch’s membrane, leading to the formation of CNV that invades the subretinal space (Montezuma et al., 2009). The cat was one of the first animals used to demonstrate CNV lesions and retinal detachment induced by laser photocoagulation(Baum et al., 1965), and subsequently a model of CNV was established in monkeys using an argon laser to disrupt the Bruch’s membrane (Ryan, 1979). In the late 1980s and 1990s,the laser-induced CNV model was extended to rodents (Dobi et al., 1989; elDirini et al., 1991; Tobe et al., 1998) and is now used extensively in both the mouse and rat to study CNV pathomechanisms and evaluate antiangiogenic therapies(Kwak et al., 2000; Takahashi et al., 2000; Yanagi et al., 2002).Laser photocoagulation in the mouse is performed with laser burns that are approximately 2 discs in diameter from the optic nerve. One of the great assets of this model is that it produces a characteristic inflammatory (day 3) and angiogenic (day 7–14) ocular response. CNV is expected to occur within 5 days. Inflammatory cells rapidly infiltrate the CNV lesion with a neutrophil peak at day 1 to day 3, followed by a macrophage peak on day 5. Inflammatory cells are no longer detected on day 7. On day 7, a typical mushroom-like lesion is seen with a regression of neoformed blood vessels from day 21 (Lambert et al., 2013). CNV lesions reach maximum sizes at day 7 post-laser and can be examined and quantified for leakage and lesion size by fluorescein fundus angiography and immunohistological staining (Gong et al., 2015). CNV then regresses and completely disappears approximately 1month post-laser. Subretinal fibrosis occurs at the lesion sites and increases up to day 35 post-laser (Ishikawa et al., 2016).As an acute injury model, it does not recapitulate the aging aspect of AMD, and although being limited by the small size of the mouse eye and lacking a macula, the laser-induced CNV model is one of the standard models for investigating choroidal angiogenesis. It enabled the therapeutic value of anti-VEGF therapies to be investigated and laid the experimental foundation for current anti-VEGF therapies in wet AMD (Aiello L et al., 1995; Krystolik et al., 2002). Having advantages such as an appropriate time course of events (1–2 weeks), high reliability and cost-effectiveness, the mouse model of laser-induced CNV has become the most established and commonly utilized model worldwide for studying the pathogenesis of CNV and its response to treatment (Tobe et al., 1998; Toma et al., 2010). The model is relatively easy tocreate, inexpensive, reproducible, efficient, and can be used in conjunction with immune manipulation (Bora et al. 2005) or transgenic mice (Rakic et al., 2003; Sengupta et al., 2003).Disadvantages include the artificial nature of the model, the small size of the mouse/rat eye, the absence of a macula, and laser photocoagulation has been used to treat and induce CNV. Also, several factors affect the quantification of the CNV lesions including ages of the mice, gender, and duration of the CNV process (Zhu et al., 2014).
Surgically-induced CNV model
A less commonly used model involves a subretinal injection of Matrigel to induce CNV in mice and rats (Cao et al., 2010; Li et al., 2011). Subretinal/RPE injection of Matrigel solidifies after implantation in tissue and stimulates local angiogenesis. CNV lesions in rats can be observed 4 days after Matrigel injection and they increase in size progressively for up to at least 20 days after Matrigel injection (Cao et al., 2010). A disadvantage of this model is the small percentage of eyes that develop CNV, with it being reported to induce CNV in B6 mice with 31% incidence (Shen et al., 2006).
Genetic model of subretinal angiogenesis
The very low-density lipoprotein receptor gene (Vldlr) is associated with the risk of developing AMD in humans (Haines et al., 2006).Vldlrgermline-knockout (Vldlr–/–) mice were generated (Frykman et al., 1995) and characterized as a model of subretinal neovascularization and choroidal anastomosis(Heckenlively et al., 2003). The abnormal neovessels inVldlr–/–retinas sprouted from the deep vascular layer in the outer plexiform layer and grew into the subretinal space as early as postnatal day 15 (Heckenlively et al., 2003; Hua et al., 2011).New vessels appeared in the subretinal space by 20 days, and subretinal hemorrhages and choroidal anastomoses were frequent by 30 days. Mice had increased vascularity of the iris and ciliary body by 8 months (Heckenlively et al., 2003), with secondary photoreceptor degeneration and subretinal fibrosis(Hu et al., 2008). Other pathological features of wet AMD developed in mice withVldlrdeficiency, such as degeneration of rod and cone photoreceptors and chronic inflammation in the retina and RPE (Chen et al., 2009; Dorrell et al., 2009).The advantages of this model are the ability to study various biological components of CNV by comparison with controls and cross breeding experiments. Disadvantages relate to the length of time for CNV to develop, the relatively small percentage of eyes that develop CNV, and the small size of the CNV.
MicroRNAs in Laser-Induced Choroidal Neovascularization Animals
An increasing number of specific microRNAs (miRNAs),called angiomiRs, have been shown to be key modulators of angiogenesis (Wang et al., 2012; Zhou et al., 2014). Several angiomiRs have been shown to be involved in CNV (Wang et al.,2012) and miRNA-based therapy may provide a rational basis for effective antiangiogenic treatment (Landskroner-Eiger et al.,2013).
MiRNAs comprise a very large number of endogenous single-stranded non-coding RNA molecules approximately 22 nucleotides long. MiRNAs are involved in basic cellular processes such as proliferation, differentiation, apoptosis, and cell cycle regulation (Mens and Ghanbari, 2018). Also miRNAs have a major role in regulating various pathological processes involved in AMD pathogenesis, including inflammation and angiogenesis (Kawa and Machalińska, 2014; Martinez and Peplow, 2020a). Dysregulation of miRNAs occurs in AMD and may facilitate the early detection of the disease and monitor disease progression (Martinez and Peplow,2020a). MiRNAs have also been shown to be involved in other neurodegenerative and age-related diseases such as Alzheimer’s disease, multiple sclerosis, diabetic retinopathy(Martinez and Peplow, 2019a, b, 2020b) and can serve as diagnostic and prognostic biomarkers and therapeutic targets. MiRNAs bind to complementary sequences in the 3′-untranslated regions (3′-UTR) of target mRNAs, and either induce mRNA degradation (Bagga et al., 2005) or inhibit their translation (He and Hannon, 2004; Meister, 2007). For example, miR-126-3p was found to decrease VEGF mRNA expression and VEGF-A protein levels in RPE cells (Zhou et al., 2016). Mechanistically, miR-126-3p directly targets VEGF-A 3′-UTR region, but another mechanism relevant to AMD is through repressing CryaB promoter activity. CryaB is a chaperone protein that can protect VEGF and other factors from denaturation and destabilization (Ruan et al., 2011).
It happened that the King s son14 gave a ball,15 and invited all persons of fashion to it. Our young misses were also invited, for they cut a very grand figure among the quality. They were mightily9 delighted at this invitation, and wonderfully busy in choosing out such gowns, petticoats, and head-clothes16 as might become them. This was a new trouble to Cinderella; for it was she who ironed her sisters linen10, and plaited their ruffles11;17 they talked all day long of nothing but how they should be dressed.
Search strategy and selection criteria
To provide further information on the involvement and role of miRNAs in CNV, we have performed a PubMed search for articles published from January 2008 to March 2020 on levels of miRNA expression in laser-induced CNV animal models to identify those likely involved in CNV development and whether overexpression or inhibition of specific miRNAs can alleviate CNV and thereby serve as therapeutic targets.
The steps involved in this review are shown in Figure 1. A total of 17 articles were found for the review. All of the studies except one had been performed with mice (mostly C57BL/6 strain) at 6–9 weeks of age and, where gender was reported,5 had used males and 2 females. One study had used female Brown Norway rats (Peng et al., 2016) and would have been≥15 weeks in age by reference to published growth charts.Except for one study that had used a 647 nm laser (Cai et al.,2014), all of the studies had used a 532 nm laser to injure the Bruch’s membrane. The number of laser burns to the eye was 1–6, laser power (intensity) 100–1000 mW, spot size 50 or 100µm, and laser duration 50–100 ms. All of the studies except one had examined retina, choroid, retina/choroid, or RPE/choroid at the sites of the laser burns; the other study had analyzed blood plasma.
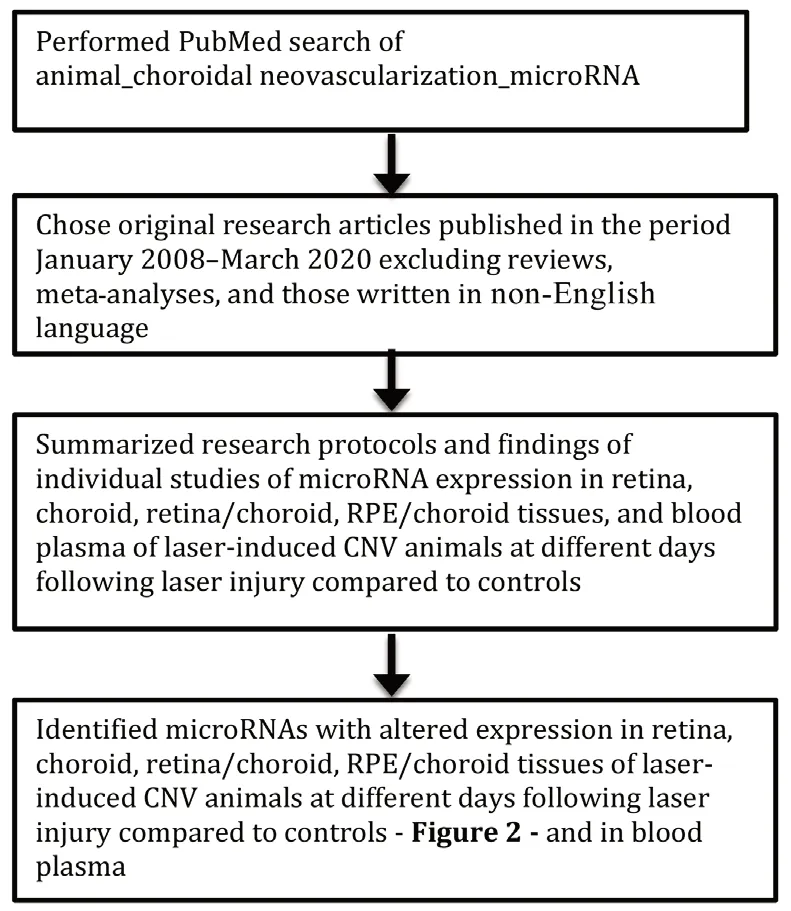
Figure 1 |Flow diagram to show how the review was performed and its contents.
RT-PCR was used in all of the studies to quantitate miRNA expression levels. The findings of the studies are summarized as follows.
Mouse studies
Zhao et al. (2019) found in whole retina and RPE/choroid of laser-induced CNV mice that miR-505 expression was significantly increased on days 1 and 3 post-laser and returned to baseline at day 7 compared to controls. A significant increase in VEGF protein in RPE/choroid was observed on days 1 and 3 post-laser. Intravitreal injection of miR-505 inhibitor almost completely eliminated VEGF induction on day 1 and day 3 post-laser, and significantly decreased CNV area at day 7 post-laser. Inhibition of miR-505 decreased M2 polarization of macrophages in CNV mice on days 1 and 3 post-laser.In an earlier study, Zhang et al. (2018) showed that miR-155 expression in the RPE/choroid tissues of CNV mice was significantly decreased on days 1 and 3 post-laser and then returned to baseline on day 7 compared to control group.VEGF protein in RPE/choroid was significantly increased on days 1 and 3, and then returned to baseline on day 7 compared to control group. Intravitreal injection of miR-155 mimic in CNV mice on day 0 and day 4 post-laser significantly increased miR-155 levels on days 1, 3 and 7 compared to control. VEGF protein was decreased on days 1 and 3.Examination of choroidal flat mounts on day 7 showed that intravitreal injection of miR-155 mimic resulted in a significant decrease of fluorescein leakage compared to control. The CNV lesion size on day 7 was significantly decreased after miR-155 mimic injection compared to control.
Hou et al. (2018) showed that miR-188-5p expression was significantly increased within the CNV lesions of chimeric mice on days 3, 5, 7, 14 and 28 compared to controls following intravitreal injection of miR-188-5p mimic, given immediately following laser photocoagulation. The levels of both MMP-2 and MMP-13 in CNV lesions were significantly decreased in the miR-188-5p mimic group on days 3, 5, 7 and 14, and CNV volumes were significantly decreased in the miR-188-5p mimic group on days 7, 14 and 28 after laser photocoagulation compared to controls. Askou et al. (2017) performed subretinal injection of mice with LV/VMD2-miR(5,B,7)-AsREDPE vector and found that this LV was localized in the RPE layer. MiR-B is a miR-93 mimic designed to release a miRNA targeting the same position in murine VEGF164as bevasiranib,a novel siRNA used for treatment of wet AMD (Askou et al.,2015). Laser-induced CNV was carried out at 21 days following LV injection, and RPE/choroidal flat mounts were prepared and examined at 7 days after CNV induction. The CNV area was decreased by approximately 85% in mice receiving the LV/VMD2-miR(5,B,7)-AsRED-PE compared to the group receiving control LV/VMD2-miR(Irr)-AsRED-PE vector. Treatment with LV/VMD2-miR(5,B,7)-AsRED-PE significantly decreased the level of VEGF protein in whole eye cellular extracts compared to the LV/VMD2-miR(Irr)-AsRED-PE group. These results suggested that the decreased VEGF levels as a consequence of LV-delivered anti-VEGF miRNAs caused the observed reduction in CNV area.
Zhou et al. (2016) observed a significant increase in miR-126-3p expression in the choroid of CNV eyes at 14 days after laser injury. Subretinal injection of locked nucleic acid (LNA)anti-miR-126-3p and LNA anti-miR-126-5p was employed to specifically silence miR-126-3p and miR-126-5p expression in the eye after laser injury. MiR-126-3p silencing significantly decreased CNV area by about 50% compared to scramble control at 14 days after laser injury. However, silencing of miR-126-5p did not significantly alter CNV area. To determine whether miR-126-3p or miR-126-5p overexpression promoted pathological angiogenesis, miR-126-3p mimic or miR-126-5p mimic was injected subretinally after laser injury and CNV was quantitated 2 weeks later. MiR-126-3p mimic led to ~60%decrease in CNV area, whereas miR-126-5p mimic mildly increased CNV lesion. Yan et al. (2016) found that miR-342-5p expression in choroid membranes was significantly increased on days 3 and 7 after laser-induced CNV, consistent with increased angiogenesis. Mice receiving intravitreal injection of miR-342-5p mimic at 24 hours post-laser showed a significant decrease in CNV area on day 7 compared to animals receiving control oligonucleotides. Wang et al. (2016a) reported that miR-93 expression was significantly decreased in RPE/choroid of the CNV eyes compared with the untreated eyes on day 14.In addition, VEGF-A mRNA and protein levels were significantly increased in RPE/choroid tissue of CNV mice compared to untreated mice. CNV mice receiving intravitreal injection of miR-93 mimic had significantly smaller CNV lesion area on day 14 post-laser compared to CNV mice treated with miR control.Overexpression of miR-93 in CNV mice resulted in a significant decrease in VEGF-A mRNA and protein level.
Mice with knockdown of miR-150 (miR-150–/–) were shown by Liu et al. (2015) to have significantly larger CNV lesions at day 7 after laser photocoagulation than wild type (WT) mice, with no significant difference in vascular leakage between miR-150–/–mice and WT mice. Cai et al. (2014) observed at 5 days after laser irradiation that miR-29a, b, and c were significantly decreased in RPE/choroid tissue of CNV eyes compared to the levels in contralateral untreated eyes, whereas at 3 days or 8 days the levels were not changed. NFκB was activated during the development of CNV with increased phospho-IKBα and decreased IκBα in RPE/choroid tissue on days 3 and 5 after laser induction compared to untreated eyes. Subretinal injection of miR-24 mimic in CNV eyes after laser injury was reported by Zhou et al. (2014) to cause a significant decrease(~60%) in CNV area at 14 days post-laser. In a previous study,Zhou et al. (2011) showed that miR-23a, miR-24, and miR-27a levels were significantly increased in the retina/choroid region of CNV eyes on day 7 after laser injury compared to day 0. Intravitreal injection of LNA-anti-miR-23/27 after laser photocoagulation decreased the CNV area by ~50% on day 14 post-laser compared with LNA-scramble.
Sabatel et al. (2011) performed intravitreal injection of CNV eyes with pre-miR-21 immediately after laser treatment,and on day 7 post-laser there was a significant decrease in CNV area (measured as blood vessel density) in mice treated with pre-miR-21. Intraocular injection of a mixture of premiR-31, pre-miR-150, and pre-miR-184 of CNV eyes after laser injury was shown by Shen et al. (2008) to cause a significant decrease in the mean CNV area at 14 days postlaser compared to CNV eyes injected with control pre-miR.There was also a significant decrease in CNV area in CNV eyes injected with pre-miR-31, pre-miR-150, or pre-miR-184 compared to CNV eyes injected with control pre-miR.
Rat study
Peng et al. (2016) found that blood plasma levels of miR-96,miR-182 and miR-183 were significantly increased on day 7 post-CNV induction in two groups receiving 6 laser burns on each of both eyes with 100 or 140 mW laser compared to pre-dose controls. The blood plasma levels of miR-96, miR-182 and miR-183 in groups receiving a smaller number of laser burns on one or both eyes with 140 mW laser were not significantly different from controls.
Discussion
Excess angiogenesis or neovascularization is a feature of several ocular diseases including retinopathy of prematurity,proliferative diabetic retinopathy, wet (neovascular) AMD, and neovascular glaucoma (Neeley and Gardner, 1998; Afzal et al., 2007; Stahl et al., 2010; Al-Latayfeh et al., 2012). Animal models have been developed to mimic vascular eye diseases with angiogenesis. They have significantly contributed to an increased understanding of basic angiogenic mechanisms and have enabled an evaluation of the efficacy and development of antiangiogenic therapies, including anti-VEGF therapies for patients with wet AMD. However, the clinical use of anti-VEGF drugs can cause severe side effects e.g., stroke,and a significant proportion of patients are nonresponsive to therapy. There is an urgent need to better understand the development and recurrence of CNV, and to identify new potential therapeutic strategies. Identifying additional antiangiogenic therapies that can be supplemental or independent of anti-VEGF therapies is dependent on basic experimental studies in proven preclinical models of ocular angiogenesis.
The mouse and rat models of laser-induced CNV have been used in studies of the wet (neovascular) form of AMD.C57BL/6 mice at 6–8 weeks of age were found to be ideal for the laser-induced CNV model and there were no gender differences when using mice of this age (Gong et al., 2015).Brown Norway male rats of 200–300 g body weight (8–15+weeks of age from published growth charts) were used in an earlier study of a laser-induced CNV model (Edelman and Castro, 2000). The CNV lesion area was proportional to the laser power level used in both mice (Gong et al., 2015) and rats (Peng et al., 2016).
MiRNAs can serve as diagnostic and prognostic biomarkers of AMD (Martinez and Peplow, 2020). The present review of studies of laser-induced CNV has shown altered miRNA expression in mouse CNV retina, choroid, retina/choroid,RPE/choroid tissues (Figure 2) and rat CNV blood plasma.Upregulation of miR-505 (days 1 and 3 post-laser), miR-155(day 14) occurred in retina; miR-342-5p (days 3 and 7), miR-126-3p (day 14) in choroid; miR-23a, miR-24, miR-27a (day 7) in retina/choroid; miR-505 (days 1 and 3) in RPE/choroid;and miR-96, miR-182, miR-183 (day 7, six laser burns on both eyes) in blood plasma. Downregulation of miR-155 (days 1 and 3), miR-29a, miR-29b, miR-29c (day 5), miR-93 (day 14), miR-126 (day 14) occurred in RPE /choroid. The measurements on days 1, 3 and 5 relate to an inflammatory response following the laser-induced injury to the retina, while those on days 7 and 14 relate to the angiogenic response (see Models of experimental CNV). There may be conflicting results regarding the expression of miR-126, as miR-126-3p was upregulated in choroid on day 14 post-laser while miR-126 was downregulated in RPE/choroid on day 14 post-laser.However, it is not reported in the latter whether it was the 3p or 5p strand that was measured. In a recent review, miRNAs that were dysregulated most often in neurodegenerative diseases and related animal models included miR-9-5p, miR-21-5p, the miR-29 family, miR-132-3p, miR-124-3p, miR-146a-5p, miR-155-5p, and miR-223-3p (Juźwik et al., 2019). Also, in retina from rats injected intravitreally with amyloid-β, as an animal model of AMD, miR-27a, miR-146a, and miR-155 were upregulated in comparison to control rats (Romano et al.,2017). These findings support linking of miR-155, miR-27, and miR-29 family to CNV.

Figure 2 |Changes in microRNA expression in retina, choroid, retina/choroid, and RPE/choroid tissues in laser-induced CNV mice as measured by real-time polymerase chain reaction assays.
Therapies using miRNA mimics or inhibitors were found to have a significant impact on CNV development in the mouse model (Table 1). Overexpression of miR-155, miR-188-5p,miR-(5,B,7), miR-126-3p, miR-342-5p, miR-93, miR-126, miR-195a-3p, miR-24, miR-21, miR-31, miR-150, miR-184, or suppression of miR-505, miR-126-3p, miR-155, miR-23/27,all resulted in decreased CNV lesions. Therapies giving rise to an increase in CNV lesion development were overexpression of miR-126-5p or suppression of miR-150. The decrease in CNV lesion caused by overexpression of the tested miRNAs except miR-126-5p most likely involves targeting of VEGF-A 3′-UTR region or repressing CryaB promoter activity as decreased VEGF expression was found with four of the tested miRNAs. Interestingly, miR-342-5p represses angiogenesis by reducing VEGF receptor and edoglin-mediated TGF-β receptor signaling, upregulating DII4, and downregulating jagged 1 in Notch signaling, leading to decreased endothelial cell proliferation and migration (Yan et al., 2016). It is less clear what mechanisms are involved in the decrease in CNV lesion brought about by suppression of some of the tested miRNAs. Certain miRNAs have proangiogenic actions and in the case of miR-23 and miR-27 they correlate with repression of their target mRNAs encoding Sprouty2 and Sema6A, which negatively regulate MAPK and VEGFR-2 signaling in response to angiogenic factors. Hence, in the absence of miR-23 and miR-27, Sprouty2 and Sema6A proteins are upregulated, with consequent dampening of MAPK and VEGFR-2 signaling (Zhou et al., 2011). Furthermore, miR-126-3p is proangiogenic and represses Sprouty 1 and PI3K regulatory subunit 2 (Cao et al., 2015). Inhibition of miR-505 suppressed M2 macrophage polarization in CNV mice on days 1 and 3 post-laser, thereby affecting the inflammatory response and reducing CNV lesion(Zhao et al., 2019).
It is noted that both overexpression and suppression of miR-155 and miR-126-3p caused a decrease in CNV lesion development. High levels of miR-155 were found to decrease the levels of SHIP1 (the SH-2 containing inositol 5′polyphosphatase), thereby promoting the PI3K/Akt pathway,while suppression of miR-155 reduced the inhibition of SHIP1 and downregulated the activity of Akt (Zhuang et al., 2015).Overexpression of miR-126-3p in RPE cells caused a significant reduction in VEGF-A protein level, while suppression of miR-126-3p led to a mild but significant upregulation of VEGF-A protein expression. MiR-126-3p regulates VEGF in RPE cells by two distinct mechanisms, namely repression of 3′-UTR VEGF-A activity and decrease of CryaB protein level. Silencing of CryaB in RPE cells significantly decreased the level of secreted VEGF in RPE cells (Zhou et al., 2016).
Anti-VEGF agents are used to reduce retinal and choroidal angiogenesis and halt the increase in capillary permeability in AMD patients. While at present there has been little research into the therapeutic potential of miRNAs for the treatment of AMD (Natoli and Fernando, 2018), supplementing anti-VEGF therapy in wet AMD patients with a set of miRNAs that have been shown to be effective in reducing CNV lesions and VEGF levels in the laser-induced CNV mouse model may enable the dose of the anti-VEGF agent injected intravitreally (e.g., brolucizumab, ranibizumab; Stewart et al., 2012) to be lowered, and could improve the number of patients responding to therapy and lower the incidence of adverse side effects. Two or three miRNAs could be chosen for example from miR-5, miR-7, miR-93 as overexpression of these in combination (miR-5, 7 with miR-93 mimic) or singly(miR-93) had been found to decrease VEGF in the mouse CNV model (Table 1). Interestingly, the anti-VEGF miRNA cluster miR-5,10,7 tested in adult human RPE cells resulted in a suppression of VEGF protein by approximately 75% (Pihlmann et al., 2012). Suppression of miR-155 by intravitreal injection of anti-miR-155 might also be a way of improving outcomes in wet AMD patients receiving anti-VEGF therapy, as miR-155 was upregulated in retinal tissue of CNV mice on day 14 post-laser (Zhuang et al., 2015) and also upregulated in retinal tissue of wet AMD patients (Pogue et al., 2018) and in neocortex and retina of AMD patients (Lukiw et al., 2012).
The laser-induced CNV model is currently the most widely used model for the wet form of AMD but has limitations.The model involves rupturing the Bruch’s membrane by laser irradiation and thereby damaging the tissues underneath.Inflammatory cells initiate the angiogenic process in this model, and depletion of either neutrophils or macrophages decreases CNV development (Espinosa-Heidmann et al., 2003;Sakurai et al., 2003; Zhou et al., 2005; Shi et al., 2011). Major features of AMD such as the formation of drusen deposits and the influence of age are absent in this model. In the absence of an aging model that does not have these limitations, the laser-induced CNV model remains one of the most commonly used models for AMD research (Gong et al., 2015).
In summary, the laser-induced CNV mouse model has provided important information on miRNA levels in CNV tissues and the influence of overexpression or suppression of specific miRNAs on CNV development. Further studies are warranted on determining miRNA expression in mouse and rat laser-induced CNV models to validate and extend the findings reported herein, as there is no mention of how reproducible the results were in many of the individual studies reviewed. Important experimental variables need to be standardized regarding strain and age of animals, gender,number and position of laser burns made to one or both eyes,laser parameters used to induce CNV including wavelength,power, spot size, and duration (see Zhu et al., 2014; Gong et al., 2015), and identifying possible confounding factors,so that more similar experiments can be performed and the findings more reliably compared and also with those of previous studies. For example, mice at 12–16 weeks of age developed more severe CNV than mice at 6–8 weeks of age,and gender differences were observed in mice at 12–16 weeks of age (Gong et al., 2015). Also, a marked decrease in CNV was observed in knockout C3–/–or C4–/–mice compared to control mice (Bora et al., 2005, 2006). Recommended methods have been described for conducting experiments with the mouse laser-induced CNV model to increase reproducibility and minimize investigator bias (Poor et al., 2014).

Table 1 |Alteration in CNV lesion development in laser-induced CNV mice following overexpression or suppression of specific microRNAs
Author contributions:Both authors contributed equally.
Conflicts of interest:The authors declare no conflicts of interest.
Financial support:None.
Copyright license agreement:The Copyright License Agreement has been signed by both authors before publication.
Plagiarism check:Checked twice by iThenticate.
Peer review:Externally peer reviewed.
Open access statement:This is an open access journal, and articles are distributed under the terms of the Creative Commons Attribution-Non¬Commercial-ShareAlike 4.0 License, which allows others to remix,tweak, and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms.
- 中国神经再生研究(英文版)的其它文章
- The use of hydrogel-delivered extracellular vesicles in recovery of motor function in stroke: a testable experimental hypothesis for clinical translation including behavioral and neuroimaging assessment approaches
- Advances in human stem cell therapies: pre-clinical studies and the outlook for central nervous system regeneration
- The emerging role of probiotics in neurodegenerative diseases: new hope for Parkinson’s disease?
- The phenotypic convergence between microglia and peripheral macrophages during development and neuroinflammation paves the way for new therapeutic perspectives
- Modeling subcortical ischemic white matter injury in rodents: unmet need for a breakthrough in translational research
- Hippo signaling: bridging the gap between cancer and neurodegenerative disorders

