Reliability of the ocular trauma score for the predictability of traumatic and post-traumatic retinal detachment after open globe injury
Simon Dulz, Vasilis Dimopoulos, Toam Katz, Robert Kromer, Eileen Bigdon, Martin Stephan Spitzer, Christos Skevas
1Department of Ophthalmology, University Medical Center Hamburg-Eppendorf, Hamburg 20246, Germany
2Care-Vision, Hamburg 20246, Germany
Abstract
● KEYWORDS: intraocular foreign body ocular trauma score; open globe injury; retina; retinal and vitreous surgery;retinal detachment; trauma
INTRODUCTION
Ocular trauma presents a prominent cause of visual impairment. The burden of blindness is related to both its inevitable effect on the quality of life and the loss of productivity that occurs in these subjects[1-2]. It can cause extreme psychological and emotional stress, as well as an economic burden to society. Worldwide, every year there are approximately 1.6 million people blinded from ocular injuries[3].Modern intraocular surgical techniques have shifted the treatment of ocular trauma and allowed for vision to be salvaged in many formerly hopeless cases. It is important to accurately diagnose open globe injury (OGI) to enable prompt referral to ophthalmology for management and to correctly counsel the patient and his family. Previous studies have reported that the following prostnostic factors according to the OGI are of relevance: initial best corrected visual acuity(BCVA), adnexal trauma, mechanism or type of injury, zone of injury, relative afferent pupillary defect (RAPD), retinal detachment (RD), vitreous hemorrhage, uveal or retinal tissue prolapse, lens injury, hyphema and delay to surgery[4-5]. Well established is the fact that young male adults are primarly affected by open or closed globe injuries[6-7].
The Ocular Trauma Score (OTS) was suggested as a standardized categorical system for prediction of visual prognosis[8]. OTS is calculated based on six risk factors (initial vision, rupture, endophthalmitis, perforating injury, RD, and RAPD) and its usefulness for predicting final visual acuity(VA) has been validated by a number of studies[9-10]. The prognostic value of the OTS for injuries in adults is widely recognized[8].
The definitions described by Pieramiciet al[11]on the localization of injury give important information on the prognosis and severity of trauma. A zone I injury is restricted to the cornea (including the limbus), a zone II injury includes the sclera no more than 5 mm posterior to the limbus, and a zone III injury is referred to scleral injury that are 5 mm posterior to the limbus. However, especially the state of the retina is essential for the long-term outcome of OGI-patients and RD during or after trauma limits the visual prognosis.
The aim of this study was to assess the prognostic value of the OTS and the zone of injury based on the definitions of Pieramici for predicting the likelihood of traumatic or posttraumatic RD. Further parameters like visual prognosis,number of surgeries required were also taken into consideration in our large cohort of patients in this one-year retrospective analysis.
SUBJECTS AND METHODS
Ethical Approval Data acquisition and evaluation of data was obtained according to the Declaration of Helsinki (1991).This study has been approved by the Ethical Committee of the Medical Association of Hamburg (PV7192) and an informed consent of the patients was not needed due to a retrospective,anonymized medical chart review.
We performed a retrospective observational chart analysis and identified 106 patients with OGI at the Medical University Center Hamburg-Eppendorf between 2010 and 2017 by searching the computerized institutional database. An OGI was referred to as a full-thickness structural break of the cornea,sclera, or both. Inclusion criteria of the retrospective analysis consisted of a follow-up of more than 1y. Four patients revealed an incomplete follow-up, therefore, a total of 102 charts were available for review and further statistical analysis.Ultrasonography was performed when indicated. Pars plana vitrectomy (PPV) was scheduled as needed.
Acquired demographic and clinical variables consisted of age, date, gender, time of injury, time until repair, mechanism of injury (rupture, laceration with further subdivision into foreign body penetration or perforation), zone of injury(zone I: corneal wound; zone II: corneoscleral injury within 5 mm of the limbus; zone III: corneoscleral wound ranging 5 mm from the limbus)[11]: injury-associated with vitreous hemorrhage, traumatic RD, post-traumatic RD (described as the occurrence of RD after a minimum of 14d), aphakia at injury, and periocular trauma. In order to evaluate a functional outcome, BCVA decimal at presentation and after a minimum of 12mo as well as the presence of afferent pupillary defect,was evaluated based upon chart review. The OTS categorical system for standardized assessment and visual prognosis associated with ocular injuries was also used. The OTS was developed by Kuhnet al[8]in 2002 and was based on the eye injury registry databases in the United States and Hungary. In addition, enucleation and the potential etiology (phthisis, pain)were evaluated accordingly.
Surgical Technique All patients gave their informed consent prior to surgery. Primary enucleation or evisceration was not performed in a single case. A 360 degree conjunctival peritomy with blunt dissection of conjunctiva to identify scleral laceration was performed. Limbal and corneal laceration repair was performed using interrupted 10-0 nylon sutures. Scleral laceration were sutured with interrupted 7-0 vicryl sutures. The entire length of the scleral wound was explored and sutured.Incarceration of the uveal/choroidal tissue or retinal tissue into the scleral wound was either replaced or removed with Vannas scissors. Scleral cryopexy was performed at all sites the surgeon considered to be at high risk for retinal breaks. All lacerations were reevaluated for their integrity (Seidel test)after forming the anterior chamber with balanced salt solution(BSS). Subsequently, vitreoretinal surgery with or without lens extraction was performed at a later stage in indicated eyes.
No chandelier light was used. A complete vitrectomy was performed and in the presence of RD, vitreoretinal incarceration a necessary retinotomy or retinectomy was performed. In addition, a peripheral 360-degree endolaser was performed and a silicone oil endotamponade (5000 cSt) was applied.
Postoperative treatment consisted of a combined dexamethasone and gentamycin ointment four times daily as well as tropicamide eye drops once daily for two weeks.
Statistical Analysis Statisical analysis were performed with SPSS software, version 27.0 (SPSS, Inc., Chicago, IL, USA).Demographic statistics were calculated for injury types and etiology and subsequently for all variables. A Pearson’s Chisquare test was used to perform frequency analysis. A oneway analysis of variance (ANOVA) was used to evaluate differences in parametric variables and a Spearman rank test was used to correlate non parametric data.Pvalues were evaluated in a two-sided fashion and aP<0.05 was considered statistically significant.
RESULTS
General Observations In total 102 patients with traumatic OGI and a completed follow-up of more than 12mo [mean:20.46mo (range: 12-105mo)] were identified and underwent further statistical analysis. The median age at presentation of injury was 48.6y (range: 3-104y) and 73.5% (75 of 102) of treated patients were male. Fifty percent (51 of 102) of injuries presented as perforating injuries followed by blunt rupture of the globe in 40.2% (41 of 102) and 9.8% by penetrating intraocular foreign body (IOFB) injuries (10 of 102).Primary surgical repair was performed in 63 patients (61.8%)within 0-6h, 32 patients (31.4%) within 6-12h and 7 patients(6.9%) after 12-24h.
Functional Outcome and Associated Analysis VA at presentation was documented in 97 patients and ranged between loss of vision [no light perception (NLP)] and 20/25.The majority of patients (82.3%) presented with a VA below 20/400. A moderate positive correlation (r=0.67,r2=0.23,P=0.00) between initial BCVA and BCVA at last follow-up was observed. In the case of a loss of vision (NLP) at presentation,BCVA improved in 54.5% until the follow-up. Enucleation(n=7) was only necessary in few cases at presentation, in which the globe was so severely damaged (e.g., loss of the entire retina),that recovery of any vision was deemed to be impossible and the patient developed a phthitic and painful eye.
Final BCVA was independent from the time of repair (Table 1),yet a statistically significant difference was present between the final BCVA and the zone of injury. Patients presenting with a zone I injury had a statistically better final BCVA when compared to zone II (P<0.001) and zone III (P<0.0001)injuries (Figure 1).
Correspondingly, severe trauma presenting with an OTS score I (P<0.0001) or II (P<0.0001) revealed a significantly worse BCVA at last follow up when compared to the cohort with an OTS score >III (Figure 2).
Zone of Injury A zone I injury was documented in 34.3%(n=35) of patients, a zone II injury in 29.4% (n=30) of patients and a zone III injury in 36.3% (n=37) of patients. Traumatic RD was observed with increasing frequency. In 22.86% of zone I injury patients RD was observed, whereas 33.33% of zone II injury patients and 56.76% of zone III injury patients presented with an initial RD (Table 2).
Additional surgeries due to post-traumatic RD was statistically more likely in patients with a zone III injury (P=0.013) when compared to a zone I injury. Of note, almost half of the patients(18 of 37 patients; 48.65%) with a zone III injury required additional surgical intervention due to post-traumatic RD(Table 3).
Retinal Detachment OGI-associated RD was observed in 36/102 patients (35.3%), whereas post-traumatic RD (defined as RD occuring 14d after OGI) occurred in 37 patients(36.3%). OGI-associated RD did not correlate with the OTS and the zone of injury, yet post-traumatic RD, as outlined previously correlated significantly with zone III injuries (Table 3).The development of proliferative vitreoretinopathy (PVR) was statistically more frequently observed in patients with zone III injuries in comparison to zone I injuries (Figure 3).
DISCUSSION

Figure 1 Association of final VA with zone of injury.
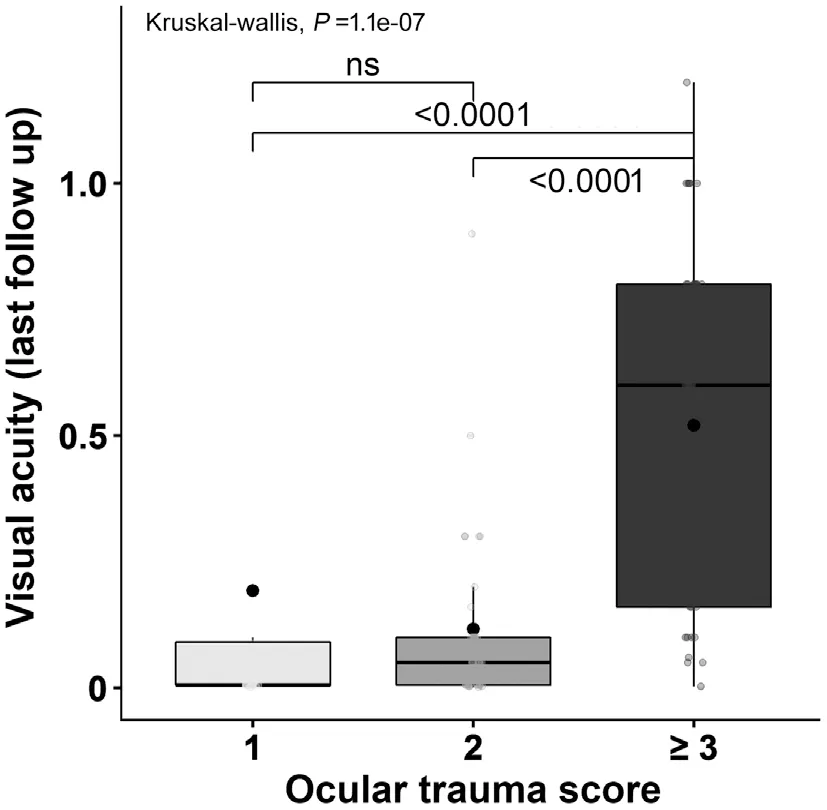
Figure 2 Association between final VA and OTS.

Figure 3 Association between PVR grade and zone of injury.
OGI belong to the most severe eye injuries, but their prognoses are very heterogeneous and depend on multiple factors[12].Treatment costs for OGI are high, including expensive surgeries and procedures, long admission time in the hospital,compensation payment to the injured patients, and loss of working days[3]. The final visual outcome among OGI patientsranges from full recovery to complete blindness or even loss of the affected globe[13-14].

Table 1 Association between final VA and the time to primary repair
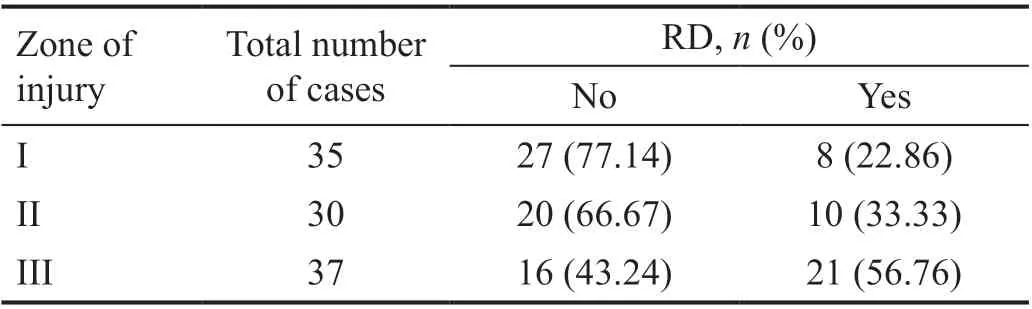
Table 2 Prevalence of traumatic RD in association with zone of injury

Table 3 Retreatment by zone of injury due to post traumatic RD
OGI with RD are a subgroup of particularly severe injuries that can be expected to have an even worse prognosis than OGI without RD. The visual prognosis is extremely guarded in part because of a high prevalence of posterior segment complications such as PVR. Stryjewskiet al[15]reported an RD rate of 29% in a series of approximately 900 OGIs. After an OGI, a PPV is often indicated in the setting of posttraumatic endophthalmitis, IOFB, media opacity, vitreoretinal traction,retinal incarceration, and RD.
Surgical timing is an important consideration in the treatment of ocular injuries and may play a critical role in the final outcome, but the timing of the intervention remains controversial. The standard practice worldwide is to conduct primary surgical repair at the earliest opportunity (in the first 24h) to preserve the structural integrity of the globe.PPV is often undertaken several days to weeks later. Most patients need on average two surgeries, and the most common surgeries performed after OGI repair are PPV, lensectomy,anterior vitrectomy, anterior chamber washout, IOL insertion,enucleation, and other vitreoretinal operations (laser,membrane peeling, cryotherapy, silicone oil tamponade, and gas injection).
PPV within one to two weeks (as we prefer as well) is recommended,because it is associated with a significant reduction of RD risk resulting from PVR and better BCVA[2,16-18], whereas delayed vitrectomy (10-14d from the time of injury) seems to be a significant risk for the development of PVR, which leads to recurrent RD[19-22]. The benefit of early intervention with PPV is to remove the maximum amount of vitreous, thus eliminating the depot for inflammation (and reduce the risk of PVR) to settle and epiretinal membranes to form. Other authors contend for delayed intervention, allowing time for the eye to recover, a complete posterior vitreous detachment to develop, and the PVR process to settle, thus making the surgery less complicated[23-27].
The results of our study show that prompt primary repair of the OGI in the first 24h was performed in the majority of cases,but interestingly the timing of intervention within the cohort was not associated with final BCVA. A major risk factor of RD and subsequently decreased final BCVA is the development of PVR. We conclude that the development of PVR is independent of timing of surgery and is instead influenced by the zone of injury (Tables 2 and 3).
The majority of patients in our cohort were male, which is in agreement with other studies. A male preponderance is a universal characteristic of eye trauma and is thought to be related to occupational exposure, participation in dangerous sports and hobbies, alcohol usage and risk-taking behavior.This might be due to gender-based behavior and male involvement in working activities with a higher risk for injuries[28-30].
Our study found a moderate positive correlation between initial and final BCVA. Better initial BCVA conceivably reflects milder ocular tissue damage, thus ensuring better visual outcome. On the contrary, an initially poor BCVA or even NLP suggests serious ocular tissue destruction, particularly of the retina and optic nerve[31-32].
The most widely used predictive model in ocular trauma is the validated OTS, which predicts final visual potential after OGI and provides the treating ophthalmologist with realistic expectations of the visual potential and, subsequently in deciding among various management strategies[8]. A patient with OTS category one will have a higher risk of poorer final VA in contrast to a patient with OTS category five who will have a higher probability of a better final VA[8].
One of the aims of our study was to elucidate the possibility of using the OTS as an RD predictive model. In our study,we found a significant association between lower OTS and lower initial BCVA and between lower OTS and a higher number of ensuing surgeries (Figure 2). However, there was no association between lower OTS and higher RD rate. Our findings are in accordance with the results of Man and Steel[33]that suggested that OTS potentially had a predictive value of the final BCVA in OGI but not for RD.The findings of our study can support the assumption that zone of injury as defined by Pieramiciet al[11]is a reliable predictive factor for RD. Zone III injuries were significantly associated with a higher number of surgeries, lower initial and final BCVA, a higher-trauma induced RD rate and post-traumatic PVR RD rate compared to zone I injuries (Tables 2 and 3).
A zone II or III wound resulted in significantly higher rates of poor visual outcome than those involving zone I OGIs.Correspondingly, Madhusudhanet al[28]predicted a 20 times the risk of having poor final VA in zone III injuries when compared zone I injuries. This could be explained by the fact that posterior wounds could cause irreparable damage to photoreceptors[28]. According to Pieramiciet al[11], Thakker and Ray[34]and Phillipset al[35], posterior OGIs are particularly serious since a zone II and/or III injury is more likely than a zone I injury to be associated with RD, phthisis, enucleation,and worse final VA.
Sympathetic ophthalmia with potential for bilateral blindness is nowadays a rare indication for enucleation of an injured eye as most cases of sympathetic ophthalmia can today be controlled by corticosteroids or other immunosuppressants[36].Most reported cases (65%) occur between two weeks to two months after injury and sympathetic ophthalmia are rare during the first two weeks after trauma[37]. As such primary surgical repair should not be abandoned for the risk of sympathetic ophthalmia in eyes with NLP. In our case series there were no cases of sympathetic ophthalmia and all enucleations (seven cases) were performed in non-salvable eyes after primary surgical repair and after vitrectomy (RD non sanata and phthisis bulbi).
Which patients are at higher risk of RD and in need of continued monitoring by a retina specialist? Reliable predictive models are essential in the treatment of such complex cases.To quantify this risk of RD, we tried to elucidate the question of whether the OTS and the zones of injury could be used as a predictive model of RD. Both models are widely used and established. Our study showed a significant association between lower OTS score and zone III injury with lower final BCVA and a higher number of surgeries, but only zone III could be significantly associated with a higher rate of RD.
A number of novel and reliable models are being developed to help address this question. Brodowskaet al[16]reported on a clinical prediction model that was developed at the Massachusetts Eye and Ear Infirmary to predict the risk of RD after OGI. The ability to reliably predict the likelihood of a patient developing an RD after OGI has implications for expectation setting, counseling, follow-up, and surgical planning.
The drawback of our study is its retrospective nature. However all patients had a one year follow-up, the models used to evaluate RD are simple and all of the patients underwent surgery with the same two experienced surgeons. Thus,further studies may be necessary to identify predictors for the occurrence and outcome of traumatic and post-traumatic RD. We hope that the results of our study could help fellow ophthalmologists to treat and monitor OGI patients closely and safely.
ACKNOWLEDGEMENTS
Authors’ contributions:Data acquisition (Dulz S,Dimopoulos V, Kromer R); Statistical analysis (Dulz S,Bigdon E, Kromer R); Manuscript preparation (Dulz S, Katz T,Kromer R, Skevas C); Internal review (Dulz S, Katz T, Spitzer MS, Skevas C).
Conflicts of Interest:Dulz S, None; Dimopoulos V, None;Katz T, None; Kromer R, None; Bigdon E, None; Spitzer MS, None; Skevas C, None.
 International Journal of Ophthalmology2021年10期
International Journal of Ophthalmology2021年10期
- International Journal of Ophthalmology的其它文章
- Exosomal miR-29b found in aqueous humour mediates calcium signaling in diabetic patients with cataract
- Intraluminal stenting versus external ligation of Ahmed glaucoma valve in prevention of postoperative hypotony
- Visual acuity after intravitreal ranibizumab with and without laser therapy in the treatment of macular edema due to branch retinal vein occlusion: a 12-month retrospective analysis
- Dexamethasone intravitreal implant (Ozurdex) in diabetic macular edema: real-world data versus clinical trials outcomes
- Comparative analysis of the clinical outcomes between wavefront-guided and conventional femtosecond LASlK in myopia and myopia astigmatism
- Vitreous function and intervention of it with vitrectomy and other modalities
