Clinical study on Tuina plus Shen Ling Bai Zhu San in treating children with diarrhea due to spleen deficiency
LI Jia (李佳)
Huguosi Hospital of Chinese Medicine, Beijing University of Chinese Medicine, Beijing 100036, China
Abstract
Keywords: Massage; Pediatric Tuina; Diarrhea, Infantile; Spleen Deficiency; Shen Ling Bai Zhu San
Diarrhea is a common disease in young children characterized by changes in stool form, such as loose or watery stools, and increased stool frequency. Children with diarrhea may also show symptoms such as fever,vomiting and abdominal pain, varying degrees of dehydration, and electrolyte and acid-base disorders[1].Western medicine usually recommends oral antidiarrheal drugs, antibiotics, and a standardized diet to prevent or correct dehydration and electrolyte and acidbase imbalance to improve the clinical symptoms.Although these methods have certain curative effects,some irrational medication and antibiotic abuse in the treatment process may bring harm to the children[2-3].
Traditional Chinese medicine (TCM) believes that the cause of pediatric diarrhea is mostly spleen and stomach deficiency. The insufficient function of transporting and transforming water and food results in unseparated water and food descending into large intestine and developing into diarrhea. There are many methods for treating pediatric diarrhea in TCM, such as Chinese material medica, acupoint injection, Tuina (Chinese therapeutic massage) and acupuncture[4-5]. In this study,we used Tuina plus Shen Ling Bai Zhu San for the treatment of pediatric diarrhea due to spleen deficiency,to provide guidance for the clinical treatment of this medical condition.
1 Clinical Materials
1.1 Diagnostic criteria in Western medicine
The diagnostic criteria in Western medicine referred to theZHU Futang Textbook of Pediatrics[6]. Daily defecation frequency >3 times, pale yellow stools like egg drop soup,or brown and smelly, might contain a small amount of mucus; stool examination showed fat globules and a small number of red and white blood cells, or pathogenicEscherichia colior rotavirus were isolated; and had a history of improper breastfeeding or unclean diet.
1.2 Criteria for syndrome differentiation of TCM
This study referred to the diagnostic criteria for the syndrome of pediatric diarrhea due to spleen deficiency in theCriteria of Diagnosis and Therapeutic Effects of Diseases and Syndromes in Traditional Chinese Medicine[7]. Primary symptoms: defecation disorders,loss of appetite, sallow and lusterless complexion,emaciated physique, a pale tongue with thin white coating. Secondary symptoms: abdominal bloating,fatigue and lassitude, watery saliva, mild puffy, eyes incompletely shut during sleep or profuse sweating,thready and weak pulse, and thin superficial veins on the index finger. It can be differentiated as spleen deficiency syndrome with four primary symptoms, or two primary symptoms and two secondary symptoms.
1.3 Inclusion criteria
Those who met the above diagnostic criteria of pediatric diarrhea in Western medicine and criteria for TCM syndrome differentiation; with disease duration over one week; aged six months to three years old; no Tuina contraindications such as bruises or skin lesions;those whose parents voluntarily allow the kids to participate in this study and signed informed consent.
1.4 Exclusion criteria
Children with infectious diarrhea, vomiting, or severe dehydration; those with other severe diseases; those with a history of diarrhea-related drug treatment in the past 2 weeks; those who had drug allergies or other contraindications.
1.5 Elimination and dropout criteria
Those who could not follow the protocol to complete the treatment; those who accidentally took some other drugs during the treatment; those who dropped out during the trial.
1.6 Statistical methods
All data were statistically analyzed by the SPSS version 21.0 statistical software. Measurement data like age,disease duration, body mass, and TCM symptom score were all in normal distribution and expressed as mean ±standard deviation (±s). The pairedt-test was used for intra-group comparisons before and after the treatment.The comparisons between the groups were analyzed by the independent samplest-test. If data did not meet normal distribution, the non-parametric test was applied.Counting data such as clinical efficacy were expressed as case or rate and processed by Chi-square test.P<0.05 was considered to indicate a statistically significant difference.
1.7 General data
A total of 105 children with diarrhea due to spleen deficiency were selected as the study objects from Huguosi Hospital of Chinese Medicine, Beijing University of Chinese Medicine between July 2019 and June 2020.The children were numbered from 1 to 105, and randomly divided into an observation group (53 cases)and a control group (52 cases) by the random number table method. During the trial, three cases dropped out in the observation group, and a total of 50 cases completed the study. Two cases dropped out in the control group, and a total of 50 cases completed the study. There were no statistical differences in the clinical data of gender, age, duration of disease, or body mass between the two groups (P>0.05), indicating that the two groups were comparable (Table 1).
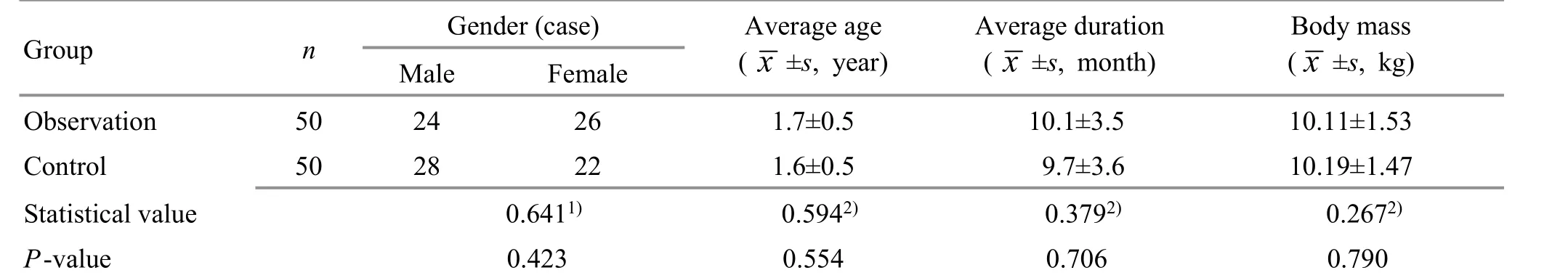
Table 1. Comparison of general data between the two groups
2 Treatment Methods
All the children received the same basic treatment,such as oral rehydration salts or intravenous rehydration according to the dehydration condition. Symptomatic treatments were adopted. Use of anti-diarrheal or antibiotics was prohibited. At the same time, feeding guidance was given to feed light and digestible food.During the treatment, the breast-fed children’s mothers were required to reduce the intake of lipid food.
2.1 Observation group
2.1.1 Tuina
Bu-Reinforcing Pijing: The physician fixed the fingerprint side of the child's thumb with the thumb and index finger, and placed the other thumb on the thumb belly of the child, Tui-Pushing the thumb belly of the child in circles 300 times (Figure 1).
Bu-Reinforcing Dachang: The physician held the child's hand and fixed his index finger with one hand, and Tui-Pushed with the radial side of the other thumb from the tip of child’s index finger till the connection between the thumb and index finger 300 times (Figure 2).

Figure 1. Bu-Reinforcing Pijing

Figure 2. Bu-Reinforcing Dachang
Yun-Circularly pushing Banmen: The physician held the child's palm with one hand, and Tui-Pushed with the other hand from the base of the thumb toward the wrist crease of the child 200 times (Figure 3).
Rou-Kneading Wailaogong: The physician held the child's palm with one hand, and An-Pressed and Rou-Kneaded Wailaogong at the center of the back of child's hand with the other hand 200 times (Figure 4).
Tui-Pushing Shangsanguan: The physician held the child's palm with one hand, and Tui-Pushed with the radial side of the other thumb pulp from the radial side of child’s wrist joint toward the elbow 200 times(Figure 5).
Mo-Rubbing the abdomen: The child took a supine position. The physician Mo-Rubbed the abdomen clockwise with his palm 200 times (Figure 6).

Figure 3. Yun-Circularly pushing Banmen

Figure 4. Rou-Kneading Wailaogong

Figure 5. Tui-Pushing Shangsanguan

Figure 6. Mo-Rubbing the abdomen
Rou-Kneading the navel: The child took a supine position. The physician Rou-Kneaded the child’s umbilicus with the thumb 200 times (Figure 7).
Tui-Pushing Shangqijiegu: Taking the coccyx tip of the child as the starting point, the physician straightly Tui-Pushed with the thumb along the line from bottom to the fourth lumbar spine 200 times (Figure 8).
Rou-Kneading Guiwei: The physician An-Pressed and Rou-Kneaded Guiwei at the end of the coccyx of the child with the thumb 200 times (Figure 9).
Nie-Pinching the spine: The child took a prone position.The physician placed two thumbs by the two sides of the child’s spine, with the index and middle fingers together in front, and Nie-Pinched the skin around the spine with the three fingers, from Guiwei to Dazhui (GV14), focusing on Shenshu (BL23), Weishu (BL21), Pishu (BL20), Ganshu(BL18), Xinshu (BL15), and Feishu (BL13), 200 times(Figure 10).
Oils, talcum powder or refreshing powder can be used for lubrication during Tuina treatment to prevent skin damage. The intensity of Tuina should be moderate,caring to protect the child’s skin. The treatment was performed once a day, 5 d as one treatment course, with a 2-day interval between two treatment courses, and a total of two courses of treatment were performed.

Figure 7. Rou-Kneading the navel

Figure 8. Tui-Pushing Shangqijiegu
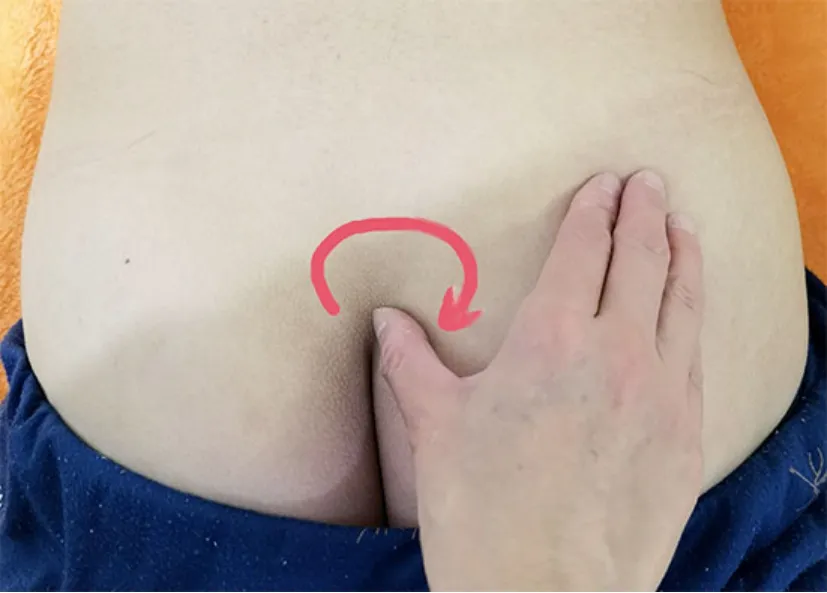
Figure 9. Rou-Kneading Guiwei

Figure 10. Nie-Pinching the spine
2.1.2 Medication
Shen Ling Bai Zhu San (State Food and Drug Administration Approval No. Z22021157, Jilin Aodong Group Vigor Pharmaceutical Co., Ltd., China), 6 g/time for children under two years old, 2 times/d; 6 g/time for children over two years old, 3 times/d; taken after mixed with warm water. Seven consecutive days consisted a treatment course, and a total of two courses were taken.
2.2 Control group
Children in the control group received the same medication as in the observation group.
在利息支出中,吸收存款的利息支出占有十分重要的地位。从图2中可见,两家银行的吸收存款利息支出增长率基本呈现下降趋势,说明对于吸收存款的利息支出趋于稳步增长。2017年南京银行吸收存款利息支出总额为145.77亿元,增长率为12.65%,中国工商银行吸收存款利息支出总额为2,504.39亿元,增长率为0.94%。总体来说,南京银行存款利息支出较大,主要原因是南京银行存款规模变大,利息支出增多,从而导致南京银行利息支出占比较高。
3 Observation of Curative Efficacy
3.1 Observation items
3.1.1 Safety indicator
During the treatment, adverse reactions were observed, and stool, urine and blood routine tests were performed.
3.1.2 TCM symptom score
Primary symptom (stool form and frequency) scores:Normal stools, banana-shaped, 1 time/d, scored 0 point;abnormal stools, soft and unshaped, 2-3 times/d, scored 1 point; mushy or loose stools, 4-5 times/d, scored 3 points; watery stools, >5 times/d, scored 5 points.
Secondary symptom (loss of appetite, abdominal bloating, and lassitude) scores: Normal state, scored 0 point; low appetite, lassitude, slight abdominal bloating but disappeared or lessened within 30 min,scored 1 point; appetite reduced by about 1/3 than normal, fatigue, and abdominal discomfort that did not disappear or reduce within 1 h, scored 2 points; food intake decreased by 2/3 or no intake, mental fatigue,lassitude, and severe abdominal bloating that did not relieve in 2 h, or even aggravated, scored 3 points.
3.2 Criteria for curative efficacy
According to theGuiding Principles for Clinical Study of New Chinese Medicines[8], and combined with the reduction rate of the total TCM symptom score, the criteria for curative efficacy in this study were established.Reduction rate of total score = (Total score before treatment - Total score after treatment) ÷ Total score before treatment × 100%.
Cured: After the treatment, the primary symptoms(stool form and frequency) returned to normal, and the secondary symptoms (loss of appetite, abdominal bloating, and mental fatigue) basically disappeared. The reduction rate of total score was ≥95.0%.
Markedly effective: After the treatment, the primary symptoms (stool form and frequency) basically returned to normal, and the secondary symptoms (loss of appetite,abdominal bloating, and mental fatigue) obviously improved. The reduction rate of total score was ≥70.0%,but <95.0%.
Effective: After the treatment, the primary symptoms(stool form and frequency) improved, and the secondary symptoms (loss of appetite, abdominal bloating, and mental fatigue) had certain improvement. The reduction rate of total score was ≥30.0%, but <70.0%.
3.3 Results
3.3.1 Safety observation
During the treatment, the stool, urine and blood routine tests of the two groups were normal, and there were no obvious adverse reactions.
3.3.2 Comparison of the therapeutic efficacy
The cured and markedly effective rate in the observation group was 60.0%, and the total effective rate was 100.0%. The cured and markedly effective rate in the control group was 38.0%, and the total effective rate was 90.0%. The differences between the two groups were statistically significant (P<0.05), (Table 2).
3.3.3 Comparison of the TCM symptom score
Before the treatment, there were no statistical differences in the primary symptom score, secondary symptom score, or total score between the two groups(P>0.05). After the treatment, the primary symptom scores, secondary symptom scores and total scores in both groups decreased significantly (P<0.05). And the above three scores in the observation group were lower than those in the control group. The differences between the two groups were statistically significant (P<0.05),(Table 3-Table 5).
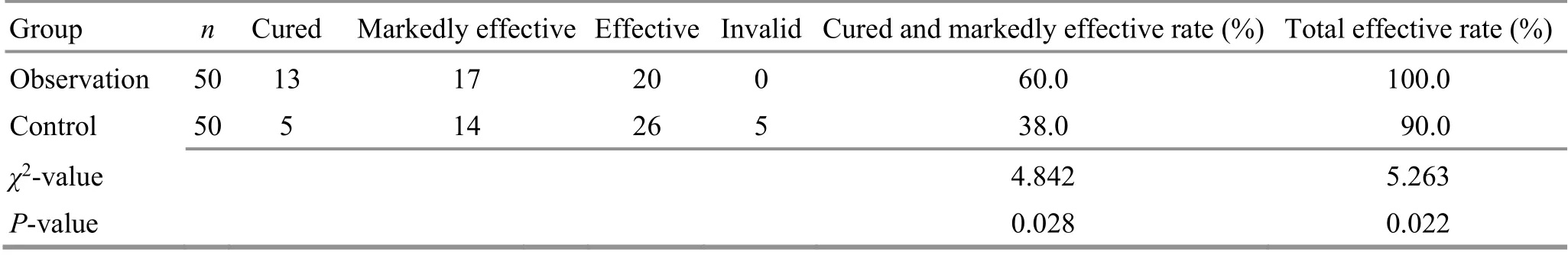
Table 2. Comparison of the therapeutic efficacy between the two groups (case)
Table 3. Comparison of the primary symptom score between the two groups before and after the treatment ( ±s, point)
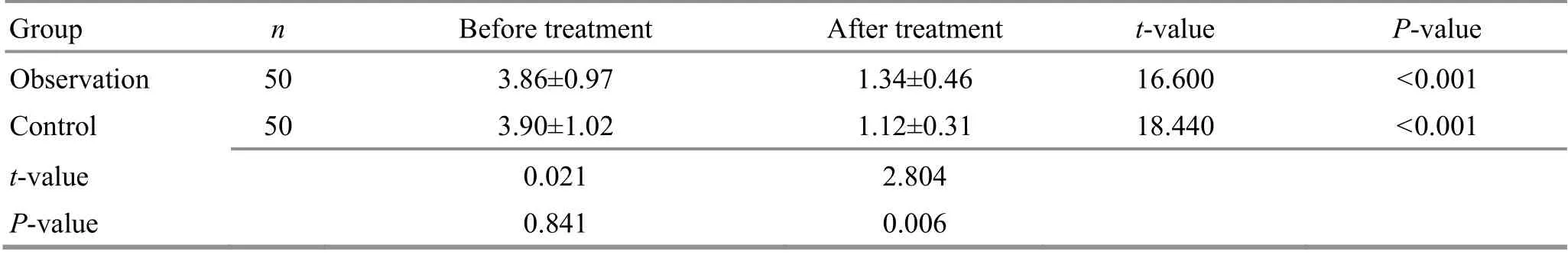
Table 3. Comparison of the primary symptom score between the two groups before and after the treatment ( ±s, point)
Group n Before treatment After treatment t-value P-value Observation 50 3.86±0.97 1.34±0.46 16.600 <0.001 Control 50 3.90±1.02 1.12±0.31 18.440 <0.001 t-value 0.021 2.804 P-value 0.841 0.006
Table 4. Comparison of the secondary symptom score between the two groups before and after the treatment ( ±s, point)
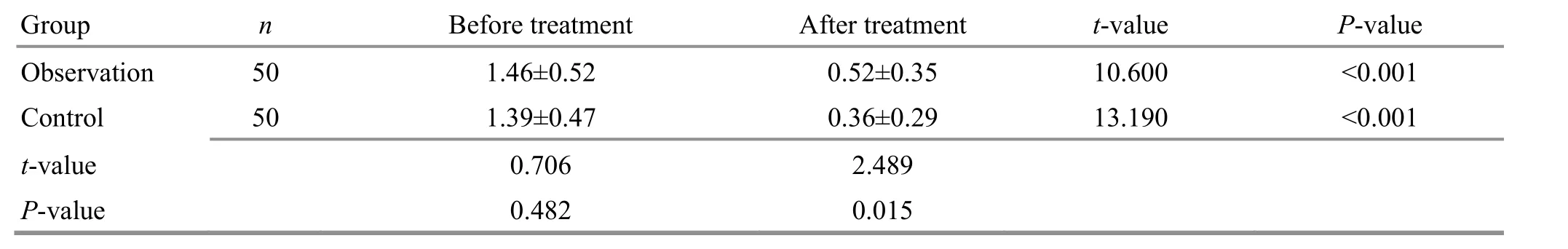
Table 4. Comparison of the secondary symptom score between the two groups before and after the treatment ( ±s, point)
Group n Before treatment After treatment t-value P-value Observation 50 1.46±0.52 0.52±0.35 10.600 <0.001 Control 50 1.39±0.47 0.36±0.29 13.190 <0.001 t-value 0.706 2.489 P-value 0.482 0.015
Table 5. Comparison of the total TCM symptom score between the two groups before and after the treatment ( ±s, point)
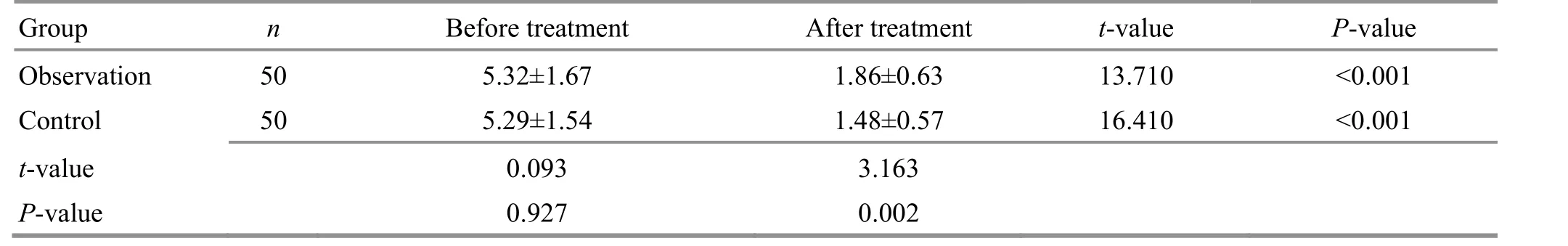
Table 5. Comparison of the total TCM symptom score between the two groups before and after the treatment ( ±s, point)
Group n Before treatment After treatment t-value P-value Observation 50 5.32±1.67 1.86±0.63 13.710 <0.001 Control 50 5.29±1.54 1.48±0.57 16.410 <0.001 t-value 0.093 3.163 P-value 0.927 0.002
4 Discussion
Pediatric diarrhea is a common gastrointestinal disease that usually occurs in infants and young children under two years old. Its incidence is second only to respiratory infections. It can cause developmental disorders and malnutrition in children. Based on etiology,the disease is divided into two types, which are infectious diarrhea and non-infectious diarrhea. Pediatric diarrhea due to spleen deficiency belongs to the latter, mostly caused by gastrointestinal dysfunction due to improper diet, allergic reactions, congenital enzyme defects, and poor immunity[9-11]. The growth and development of infants and young children need a lot of nutrients, but due to the imperfect development of their digestion and absorption systems, they are prone to have a series of symptoms of diarrhea when nutrients are excreted before being fully absorbed and digested. At the same time, because of the low levels of serum immunoglobulin (Ig) A and IgM in infants and young children, the immune function is poor. Once invaded by external pathogenic factors, they are liable to develop gastrointestinal disorders and diarrhea[12-13]. Western medicine treatment of the disease mainly aims at the pathogenic factors and improving the balance of water,electrolytes and acidolysis by supplementing nutrition and regulating the distribution of intestinal flora.
Pediatric diarrhea belongs to “Xie Xie” (diarrhea) in TCM. TCM believes that the cause of the disease is mainly related to spleen and stomach deficiency, and its pathogenesis is the transporting and transforming disorder of the spleen and stomach. Under normal physiological conditions, the stomach governs receiving and decomposing water and food, and the small intestine separates the clear from the turbid. The clear is transformed and transported to the whole body through the three Jiao (triple energizer) pathways, and part of it is discharged as urine through the bladder. The turbid is transmitted to the large intestine and discharged as stools through the anus. If the transportation and transformation of spleen and stomach fail, and the small intestine fails to separate the clear from the turbid, the clear will mingle with the turbid and pour downward together to cause diarrhea. Because the Zang-Fu organs of infants and young children are delicate, if effective treatment is not given in time after diarrhea, it will seriously affect their health[14].
In this study, we observed the curative effect of internal treatment combined with external treatment for infantile diarrhea. The internal treatment was oral Shen Ling Bai Zhu San, which can invigorate the spleen and stomach, benefit lung Qi, and has a good effect on the deficiency of spleen and stomach, poor appetite, loose stools, and lassitude. CHEN L[15]applied Shen Ling Bai Zhu San to treat 124 cases of infantile diarrhea, and the clinical effect was satisfactory. MA J X,et al[16]found that Shen Ling Bai Zhu San can improve the clinical symptoms in children with diarrhea due to spleen and stomach deficiency, and improve their quality of life. The results of these studies all suggest that Shen Ling Bai Zhu San has a good effect on pediatric diarrhea.
Pediatric Tuina is a unique treatment of TCM.Compared with oral Chinese medicine, Tuina can avoid the irritation of the gastrointestinal tract of children with no toxic side effects but higher clinical compliance[17].Acupoint Tuina can improve gastrointestinal blood circulation, regulate digestive and absorptive function of gastrointestinal tract, and at the same time stimulate the corresponding nervous system and tissues to release bioactive substances, accelerate the excretion of inflammatory substances and acidic metabolites, and improve the immunity of the body[18]. Bu-Reinforcing Pijing and Bu-Reinforcing Dachang applied in this study can invigorate the spleen and stomach, replenish Qi and blood, achieving effects of astringing intestine and arresting proptosis, warming spleen and stomach for stopping diarrhea. Yun-Circularly pushing Banmen can invigorate the spleen and harmonize the stomach,resolve food stagnation, and stop diarrhea and vomiting.Rou-Kneading Wailaogong and Nie-Pinching the spine can warm Yang for dispelling cold, rouse the Yang Qi, and harmonize the stomach Qi. Mo-Rubbing the abdomen,Rou-Kneading the navel, Tui-Pushing Shangqijiegu and Rou-Kneading Guiwei are four methods to stop diarrhea.The abdomen and navel belong to the Conception Vessel,while Guiwei and Qijiegu belong to the Governor Vessel,one for Yin and one for Yang. The combination of Yin and Yang can promote the gastrointestinal function of clearing the clear from the turbid. Tui-Pushing Shangsanguan can invigorate the healthy Qi and promote sweating for activating Qi flow, making all the meridians harmonized. The combination of the above methods can invigorate the spleen and harmonize stomach, warm Yang for dispelling cold, resolve food stagnation, and stop diarrhea and vomiting[19-20].
Results of this study showed that the improvements of primary and secondary symptoms after treatment in the observation group were more significant than those in the control group, and the total effective rate was higher than in the control group, suggesting that Tuina plus Shen Ling Bai Zhu San is effective and safe for pediatric diarrhea due to spleen deficiency.
Conflict of Interest
The author declares that there is no potential conflict of interest in this article.
Acknowledgments
There was no project-fund support for this study.
Statement of Informed Consent
Informed consent was obtained from the guardians of all individual participants.
Received: 14 December 2020/Accepted: 27 April 2021
 Journal of Acupuncture and Tuina Science2022年1期
Journal of Acupuncture and Tuina Science2022年1期
- Journal of Acupuncture and Tuina Science的其它文章
- Effects of electroacupuncture with different frequencies on hippocampal neuronal apoptosis and JNK signaling pathway in rats with vascular dementia
- Effects of electroacupuncture pretreatment on M1 polarization of alveolar macrophages in rats with acute lung injury
- Clinical observation on row needling at the Governor Vessel on the head for poststroke insomnia
- Effects of Tuina combined with graded motor imagery on the upper-limb motor function and quality of life of patients with hemiplegia after stroke
- Effects of acupuncture combined with Brunnstrom staging on upper-limb motor function, cerebral arterial blood flow velocity, and brain function remodeling after stroke
- Observation of the efficacy and safety of the Song-Relaxing and Zhen-Vibrating abdomen manipulation for patients with prediabetes
