An updated study of traditional medicines to the era of 1,3,4 oxadiazole derivatives for malaria treatment
Davinder Kumar,Harsh Kumar,Aakash Deep,Rakesh Kumar Marwaha*
1Department of Pharmaceutical Sciences, Maharishi Dayanand University,Rohtak 124001, Haryana, India. 2Department of Pharmaceutical Sciences, Chaudhary Bansi Lal University,Bhiwani 127021,Haryana,India.
Abstract
Keywords:antimalarial; Plasmodium falciparum;1,3,4 oxadiazoles; traditional medicines
Background
Modern antimalarial drugs are derived from two types of traditional medicines (artemisinin and quinine derivatives), which have been used by human beings since thousands of years. Traditional medicines are potentially a viable source of antimalarial treatment in poor communities due to the problems of drug resistance and limitations on access to antimalarial drugs. Research initiative on traditional antimalarial methods is research enterprise that focuses on traditional antimalarial methods for malaria treatment. It was created in 1999 with the aim of promoting research on available traditional medicines[1]. Malaria is a severe infection that fatal in its nature and spreads by the biting of an infected Anopheles mosquito. Plasmodium parasite is carried out by infected mosquitos. The parasite is released into the bloodstream when mosquito bites and the parasites migrate to the liver, where they mature. The mature parasites then, enter the bloodstream and begin to infect red blood cells after a few days. The parasites multiply inside the red blood cells within 48 to 72 hours,causing the infected cells to burst open [2-4] (Figure 1).
Malaria can also be transmitted through blood transfusion, organ transplantation and the use of shared needles or syringes. Typically, it takes up to 4 weeks following infection to develop symptoms of malaria (Figure 1). Some common symptoms of malaria include high fever, muscular pain, headache, nausea, diarrhoea, vomiting, bloody stools, coma and abdominal pain.
Malaria can occur if you are bitten by an infected mosquito carrying the Plasmodium parasite.Plasmodium vivax,Plasmodium ovale,Plasmodium malariaeandPlasmodium falciparum,Plasmodium knowlesi
(Figure 2) are the five types of malaria parasites that can infect humans and 2 of these species -Plasmodium falciparumand
Plasmodium vivaxbring the greatest risk.Plasmodium falciparumis the most dangerous malaria parasite and the most widespread to African continent.Plasmodium vivaxis the leading malaria parasite in most countries outside of sub-Saharan Africa. It is sometimes preventable and curable [5,6].
The blood tests can also give some vital information to the doctor such as the type of malarial parasite, the extent that the infection has spread and damaged certain organs. Anemia can be caused by due to the destruction of erythrocytes caused by certain parasites that are resistant to drugs (Haematinics). There are certain antimalarial compounds, their targets and mode of action used to treat malaria(Figure 3) such as quinine, mefloquine, primaquine etc., but these drugs also come with their own set of problems like adverse events,long dosage regimens. These antimalarial drugs are efficient but are increasing the drug resistance of the parasite which could be terrible in the long run, that is why we need to start looking for better pharmaceutical compounds from the traditional medicine to treat malaria[7-12].
Sources and selection criteria for this review study
Through the many scientific platforms i.e. Medline, Embase, CAB,PubMed, Scopus, Sociofile and the Cochrane Library, we gone through and screened various published articles over the past decade for this study.
Malaria and its impact over the worldwide
Worldwide, there are estimated to be 241 million malaria cases and 627,000 malaria deaths in 2020, according to WHO’s latest world malaria report. The number of cases in 2020 increased by about 14 million over 2019 and the number of deaths rise by 69,000.
In the pandemic, interruptions in malaria treatment, diagnosis and prevention contributed to roughly two thirds of these additional deaths [13-15].
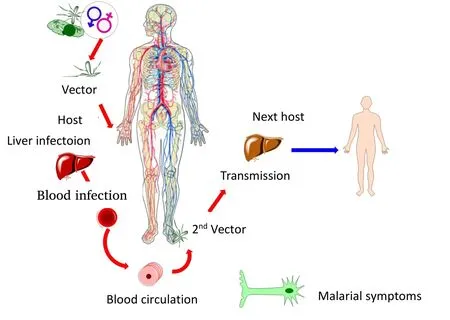
Figure 1 Transmission process of malarial infection in human
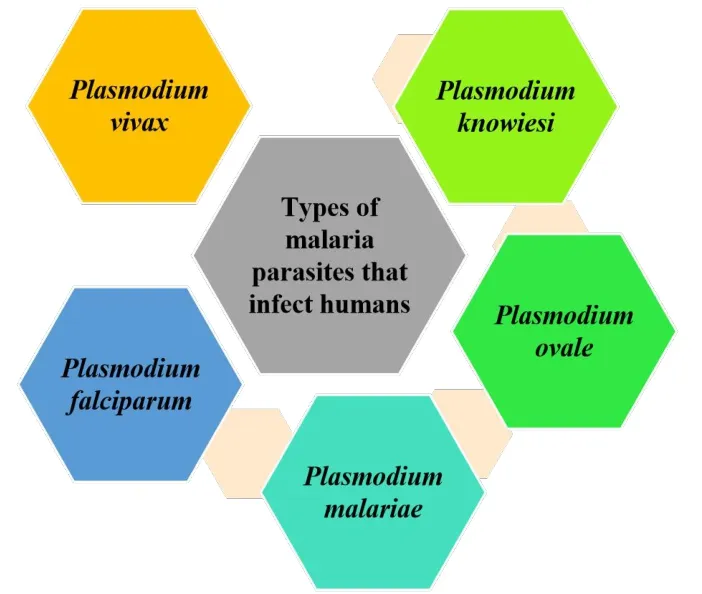
Figure 2 Different types of malarial parasites
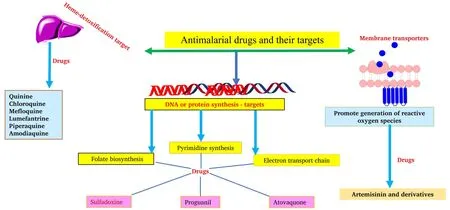
Figure 3 Antimalarial drugs and their mode of actions
India reported more deaths and cases than any other country during the period of 2019 to 2020. There have been more than 150 million malaria cases and 390,000 deaths in high burden to high impact countries since 2015, followed by 154 million cases and 398,000 deaths by 2019 and 163 million cases and approx. 45 thousand Plasmodium sporozoites deaths by 2020 [16-18]. Modern medicine evolved from certain natural products or was inspired by them in the recent past.They have also contributed to the development of antimalarial drugs. Even uncomplicated malaria is now recommended to be treated with artemisinin-based combination therapy by the WHO. Artemisinin’s should not be used as monotherapy,in order to avoid rapid emergence of resistance, they should be used alongside other antimalarials[19-22]. This study focuses on compounds that have already been identified in traditional medicine, including artemisinin (a sesquiterpene lactone) and potent synthetic derivatives.
Traditional medicines
Malaria is treated with traditional medicines from thousands of years and the source of the two main groups of modern antimalarial drugs are artemisinin and quinine derivatives. Traditional medicines are potentially a viable source of malaria treatment in poor communities due to the problems of drug resistance and limitations on access to antimalarial drugs [23]. Artemisinin is a compound found in the herbArtemisia annuaand was first extracted in 1971 [24]. The 2015 Nobel Prize was awarded to Tuyou for his work on artemisinin in the fight against malaria and reported extensive use of artemisinin and its derivatives in combination therapy (artemether, artesunate, artether and dihydroartemisinin) [25].
Other traditional medicines are available in different countries
The antimalarial activity of several natural compounds is being investigated, besides artemisinin. In studies on stilbene glycoside compound, a stilbene glycoside compound extracted fromParthenocissus tricuspidata(Vitaceae), as well as being effective againstPlasmodium bergheiat the blood stage and overall survival, the drug was also associated with a long-term anti-toxin response. The extract ofPlasmodium tricuspidatainhibitsPlasmodium falciparumwith an inhibitory concentration (half-maximal inhibitory concentration(IC50)) of 5.3 μM [26, 27].
Malaria is treated with a leaf extract ofVernonia amygdalina, a natural plant common in southern Nigeria that has shown activity against Plasmodium. An extract of theVernonia amygdalinaleaf containing ethanol inhibited the growth ofPlasmodium bergheiin vivo based on its concentration. Furthermore, leaf extracts also reduced nitric oxide levels, lipid peroxidation levels and proinflammatory cytokines (tumour necrosis factor and interferon gamma), which is an indication of immunomodulatory effects [28-30]. Different plants were also tested for antiplasmodial compounds such asCalotropis gigantea(L.) (Poacae),Alchornea laxiflora,Toddalia asiatica(L.) Lam.(Rutaceae),Pongamia pinnata(L.) (Poacae),Pierre,Zea maysL.(Poacae),Murraya koenigii,Quassia amaraL. (Simaroubaceae) andTriclisia gilletiiagainstPlasmodium falciparumandPlasmodium berghei[31-33].
Alternative medicines and treatment modalities
In light of the resistance to the current front-line antimalarial therapy,artemisinin combination therapies, the discovery of new chemical entities to treat malaria has been recognized as a global health priority[34]. Therefore, new antimalarial drugs are still urgently required to supplement or replace existing treatments. Antimalarial drugs must meet strict criteria to be considered for use, such as being safe,effective against strains showing clinical resistance to existing antimalarials, having good pharmacokinetics for oral use, being affordable and exhibiting symptoms relief as fast as artemisinin’s [35,36]. Due to their many applications, heterocyclic chemistry has become a leading area of research in the pharmaceutical industry. A wide variety of heterocyclic molecules containing oxygen and nitrogen have demonstrated the greatest biological activity. Chemical moieties i.e. five membered heterocyclic ring containing compound especially 1,3,4-oxadiazoles and its derivatives are known to possess diverse pharmaceutical applications along with various biological actions[37, 38].
Felix Caldero’n et al. (2017) prepared and investigated in vitro antimalarial activity of novel aminoxadiazoles derivatives. All the novel derivatives tested in vitro antimalarial activities using sensitive strain 3D7A by (3H) hypoxanthine incorporation assay method. After completion of all studies, they found compound 5-((3,4’-bipyridin)-2’-yl)-N-(4-(pyrrolidin-1-ylmethyl) phenyl)-1,3,4-oxadiazol-2-amine (Figure 4) was administered (300 and 500 mg/kg)to female Swiss CD-1 mice. The concentration achieved at the highest dose was 68.9 μg·h/mL. Scientists observed no serious adverse effects at 500 mg/kg of the functional observatory battery, but they observed some clinical signs of passivity. The antiparasitological profile or parameters shown in Table 1 [39].
Arabinda Ray et al. (2009) design and synthesized 1, 2, 4-triazole and 1, 3, 4-oxadiazole analogues and investigated antimalarial activity againstPlasmodium falciparum[40].The compounds 4-(((4-(4-((4-hydroxybenzylidene) amino)-5-mercapto-4H-1,2,4-triazol-3-yl)phenyl) imino) methyl) phenol 01 and 5-(4-((4-chlorobenzylidene) amino) phenyl)-1, 3, 4-oxadiazole-2-thiol 02 (Figure 5) were found most active. Furthermore, these compounds were tested both computationally and in vitro for their potential as dihydrofolate reductase inhibitors against thePlasmodium falciparumdihydrofolate reductase receptor.
Potent compounds 01 and 02 were further examined for their ability to inhibit bovine liver dihydrofolate reductase enzyme activity usingPlasmodium falciparumstrains and standard drugs (chloroquine &pyrimethamine). The average IC50(µM) values of potent compounds(01 and 02)are presented in Table 2.
The IC50values of active derivatives, indicating that both of compounds are significantly dihydrofolate reductase inhibitors as compared to standard drugs (Table 2). According to structure activity relationship studies (Figure 6), nitrogen containing triazole scaffold attached with two m-nitrobenzene groups (IC50= 0.0259 ± 0.006µM) was found to be most potent derivative, while compound (02)with 4-Cl in phenyl ring was found to be moderate inhibitor(IC50(µM)= 0.0450 ± 0.005) of enzyme compared to chloroquine (Table 2).Thus these dihydrofolate reductase enzyme inhibitors could be lead structure as antimalarial agents.
M. Shaquiquzzaman et al. reported novel pyrazole-1,3,4-oxadiazole hybrid derivatives and evaluated them in vitro antiparasitic (Malarial)activity using the schizont maturation inhibition assay [41]. All the synthesized derivatives tested against ofPlasmodium falciparumstrain using a culture of 3D7. Among the all derivatives, compound 03 (IC50= 0.248 µg/mL), a furan-linked oxadiazole (Figure 7) derivative was found to be the most potent as compare to refrence drug chloroquine(IC50= 2.154 µg/mL).
In continuation of similar work, M. Shaquiquzzaman et al. reported pyrazole clubbed 1,3,4 oxadiazole with their amide derivatives [42].All synthesized derivatives were evaluated their antimalarial potential using schizont maturation inhibition assay against chloroquine sensitive ofPlasmodium falciparum(3D7 strain). Among the all-synthesized derivatives, 04 different oxadiazole derivatives, i.e.,04, 05, 06 and 07 were found most active (Figure 8), with IC50less than 1 µM. From all potent derivatives, compound 07 had shown significant antimalarial potential as compare to chloroquine (IC50=0.405) as reference drug.
Discussion
Over three million deaths each year are attributed to parasitic diseases caused by various plasmodium’s in developing nations. We review recent studies involving secondary metabolites from medicinal plants that have demonstrated a moderate to high level of activity against plasmodium in vitro and in vivo bioassays. Despite the widespread practice of traditional medicine to treat malaria and its availability and affordability, it is out of limitations. Firstly, there is a lack of clinical and scientific data on safety and efficiency. The best plants,preparations and dosages have also yet to be agreed upon even among traditional healers. Different plant species have considerably different concentrations of active ingredients, which is caused by a variety of factors. Therefore, we need to express the benefits of the alternative treatment modality i.e. synthetic heterocyclic derivatives-1,3,4-oxadiazoles and its derivatives, due to drug resistance in prevention of malaria. So many research on going to develop novel molecules due to drug resistance in prevention of malaria and target to treat this deadly disease.
Possible targets for development of novel antimalarial drugs
Throughout this time, a consistent effort has been made to cure malaria. The biggest obstacle to progress against malaria is the emergence and spread of resistance to current drugs. Therefore, the majority of research seems to focus on finding solutions to counteract this. Therefore, huge efforts have been putted into the development of new drugs for finding new mechanism of actions. The pharmaceutical industries are currently studying metabolic and biochemical pathways of parasites to find and exploit new drug targets. Thus, from the last decade, the drug development focus has been primarily only on different metabolic pathways of malarial parasites. Researchers are also developing new chemical complexes or specific inhibitors that attack these new targets. These possible targets are summarised in the Figure 9 and these targets may be played significant role for the development of novel antimalarial molecules with high efficacy and less toxicity.
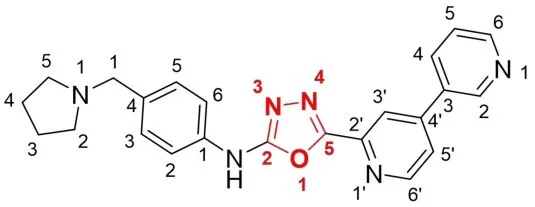
Figure 4 5-((3,4’-bipyridin)-2’-yl)-N-(4-(pyrrolidin-1-ylmethyl)phenyl)-1,3,4- oxadiazol-2-amine
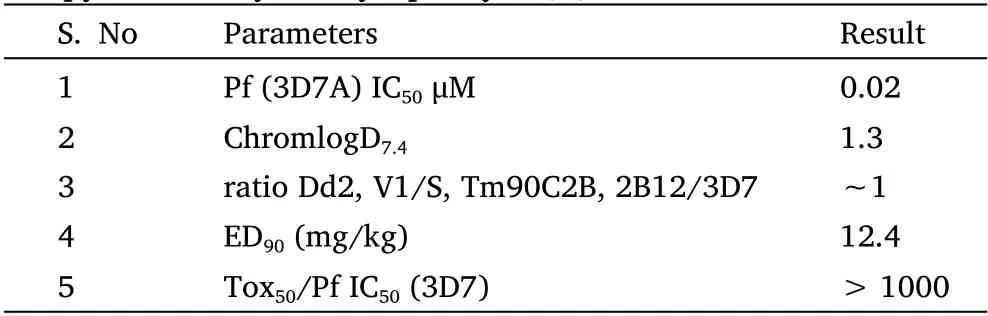
Table 1 Antiparasitological profile of 5-([3,4’-bipyridin]-2’-yl)-N-(4-(pyrrolidin-1-ylmethyl) phenyl)-1,3,4-oxadiazol-2-amine
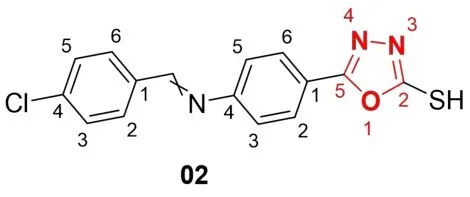
Figure 5 Potential as dihydrofolate reductase inhibitors
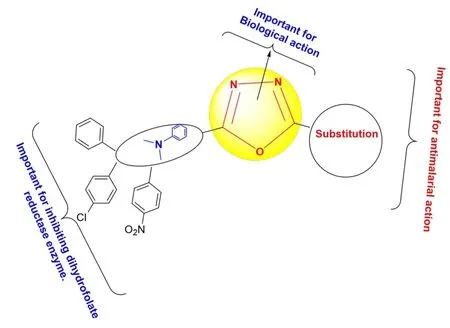
Figure 6 Structure activity relationship of derivatives
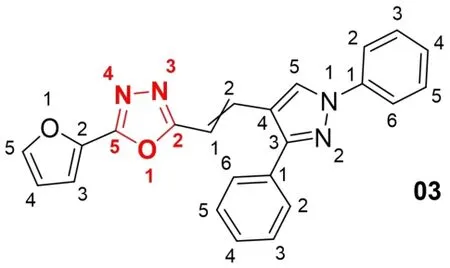
Figure 7 2-(2-(1,3-Diphenyl-1H-pyrazol-4-yl) vinyl)-5-(furan-2-yl)-1,3,4-oxadiazole(Compound 03)
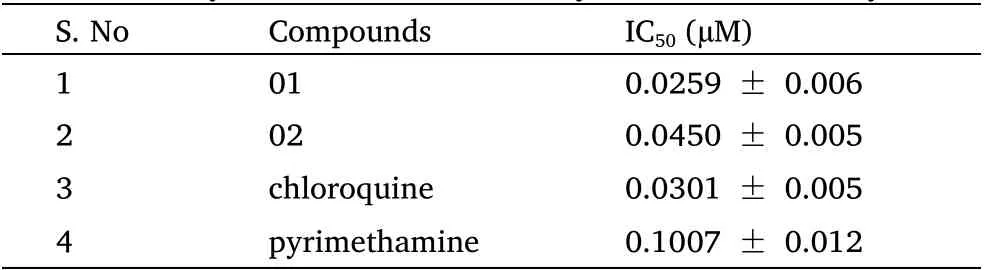
Table 2 Dihydrofolate reductase enzyme inhibition assay
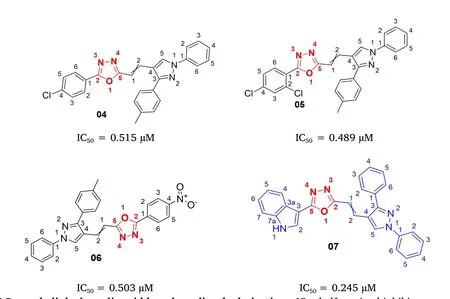
Figure 8 Pyrazole linked acrylic acid based oxadiazole derivatives.IC50, half-maximal inhibitory concentration.
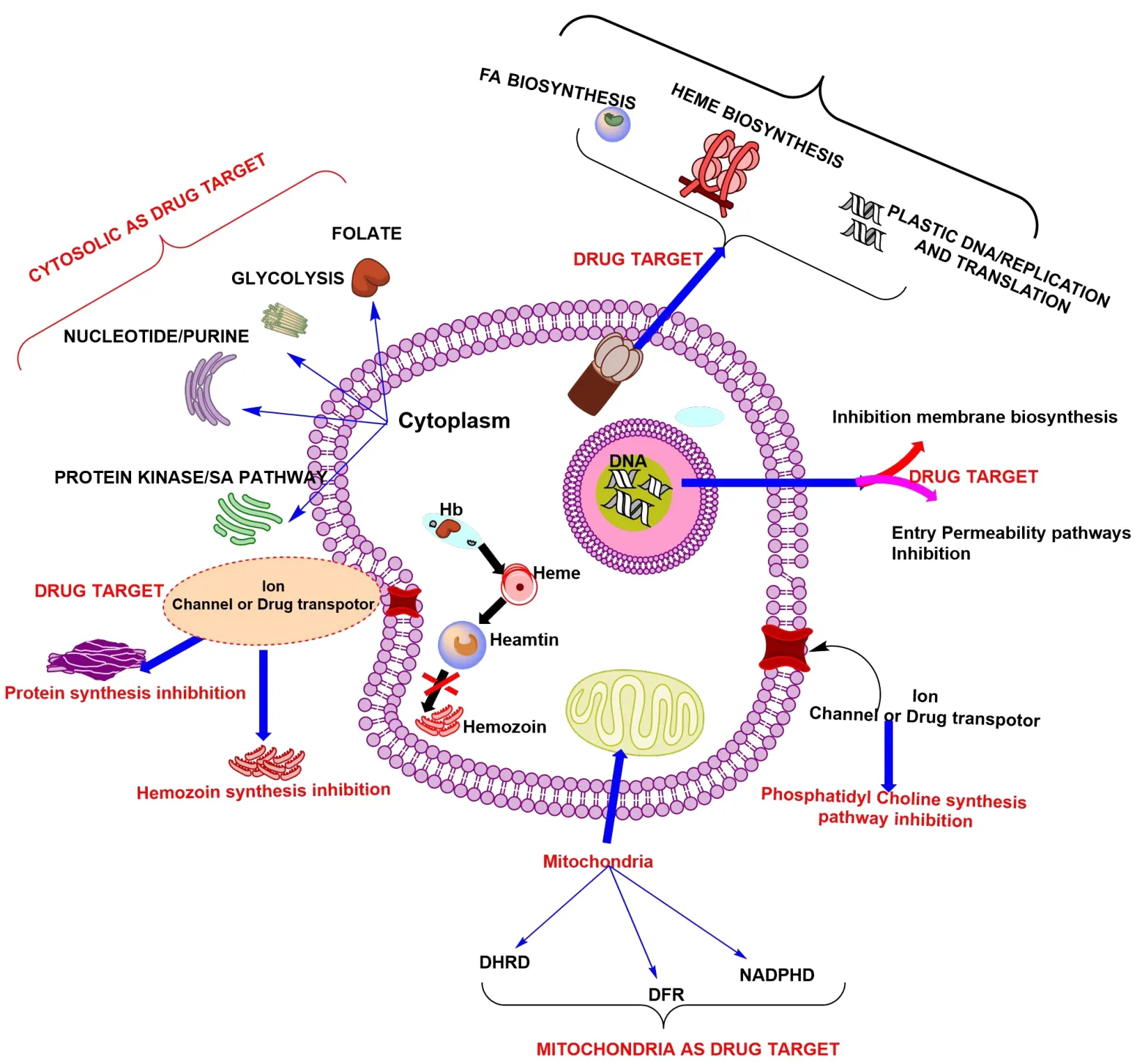
Figure 9 Different possible targets for antimalarial drugs development.FA,fatty acid;Hb,hemoglobin;DHRD,dihydropteroate synthase;DFR,dihydrofolate reductase; NADPHD, nicotinamide adenine dinucleotide phosphate dehydrogenase; DNA, deoxyribonucleic acid.
Conclusion
The current review sheds vital light on the prevalence and profile of the use of traditional medicines for malaria. There are currently no other drugs that can treat chloroquine-resistantPlasmodium falciparuminfections and there has not yet been any evidence of resistance to these compounds. Around the world, there are a variety of strategies being used to prevent malaria. These strategies are making significant progress, especially in decreasing total mortality rates in endemic nations like tropical and subtropical areas. In addition, drug-resistant forms have caused a setback and new drugs are needed going forward that do not have the same mechanisms of action as existing medications. The availability of several treatments is not enough;novel, effective, cost-effective and better patient-friendly treatment options are urgently needed to reduce this threat. Treatment with the current therapeutic regimen is associated with toxicities, long durations, high costs and parasitic resistance. The chemical approaches aren’t the only way to overcome this obstacle; many biologically based treatments are being studied (neutralizing antibodies, immunotherapy). In addition to their diverse benefits for pharmaceutical applications, 1,3,4-oxadiazoles and its derivatives are known for exhibiting antimalarial effects with specific mechanism of action. Therefore, to prevent the rapid emergence of resistance, every effort should be made to use these compounds (Traditional medicines or synthetic heterocyclic derivatives), vaccine development and another novel drug discovery, there is still room for improvement.
 Traditional Medicine Research2023年1期
Traditional Medicine Research2023年1期
- Traditional Medicine Research的其它文章
- Metabolomics and network pharmacology reveal the mechanism of the Jiawei Yangshen pill in treatment of cyclophosphamide-induced dyszoospermia in mice
- Multi-component quantitative and feed-forward neural network for pattern classification of raw and wine-processed Corni Fructus
- Rutaecarpine attenuates monocrotaline-induced pulmonary arterial hypertension in a Sprague-Dawley rat model
- Forget the past,there is no future
- Medicinal plants and phytomedicines are used to treat or prevent illnesses in Sudan:a review
