Changes of optic nerve head microcirculation in high myopia
Wen-Quan Tang, Yu-Lin Luo, Xi-Lang Wang, Xuan-Chu Duan
1Department of Ophthalmology, Hunan Children’s Hospital,Changsha 410007, Hunan Province, China
2Changsha Aier Eye Hospital, Changsha 410011, Hunan Province, China
3Aier School of Ophthalmology, Central South University,Changsha 410011, Hunan Province, China
Abstract
● KEYWORDS: high myopia; optic nerve head; optical coherence tomography angiography; vascular density; axial length
INTRODUCTION
Myopia is the most prevalent correctable visual impairment worldwide. The prevalence of myopia and high myopia (HM) is continuously increasing, especially in Asian populations[1‐2]. HM is characterized by progressive extension of the axial length (AL) and degenerative structural changes in the fundus[3]. Increasing evidence suggests that chorioretinal vascular dysfunction may be an associated complication or factor of HM[4‐5]. Of note, previous studies have reported a decrease in the retinal vessels perfusion in HM[5‐6]. Besides stenosis of retinal arterioles, and decrease in retinal blood flow is also associated with AL elongation[7‐9].Thus, impaired retinal blood flow can play a crucial role in developing HM‐associated degenerative changes. Therefore,it is important to study optic disc microcirculation changes in HM. In this study, we used optical coherence tomography angiography (OCTA) to detect changes in the optic nerve head(ONH) microcirculation in HM. We compared microcirculatory parameters at different ages, spherical equivalent (SE), and AL.Further, we assessed the correlation between microcirculatory parameters with these factors to screen out the related and predictable indicators of HM related degenerative changes.
SUBJECTS AND METHODS
Ethical ApprovalThe study adhered to the principles of the Declaration of Helsinki. The study protocol was approved by the Ethics Committee of Changsha Aier Eye Hospital, Central South University, Changsha, China. Written informed consents were obtained from all cases.
SubjectsFrom May 2020 to June 2021, the medical records of 167 consecutive patients with myopia in the Refractive Department were reviewed. Comprehensive examinations including slit‐lamp biomicroscope, mydriatic indirect ophthalmoscopy, intraocular pressure (IOP), AL (IOL Master 700; Carl Zeiss Meditec, Germany), ultra‐widefield fundus imaging (Optos; Daytona P200T, Nikon, Japan), OCTA(RTVue‐XR Avanti; Optovue, Fremont, CA, USA), visual acuity and refractive error were assessed.
Inclusion criteria: 1) SE<‐6.00 D; 2) IOP≤21 mm Hg; 3)OCTA signal strength index ≥50. Exclusion criteria: Patients with hypertension, diabetes, systemic connective tissue disorder, or any other ophthalmic disease (such as cataract,glaucoma, macular hole, retinal hole, or retinal hemorrhage),history of ophthalmic trauma, or surgery.
Parameters from Optical Coherence Tomography AngiographyOCTA system automatically measured the peripapillary vascular density (PVD) and intrapapillary vascular density (IVD). A 6×6 mm2cube and a 4.5×4.5 mm2cube scan centered were obtained on the fovea and ONH,respectively. ONH was divided into 8 sectors (superanasal,SN; nasosuperior, NS; nasoinferior, NI; inferonasal, IN;inferotemporal, IT; temporoinferior, TI; temporosuperior, TS;superotemporal, ST; Figure 1).
Statistical AnalysisSPSS22.0 software was used for the statistical analysis. The data were presented as mean±standard deviation (SD). Analysis of variance (ANOVA) and least significant difference (LSD) was applied for different analyses between groups. With theP‐value of <0.05, the difference was considered to be statistically significant.
RESULTS
Demographic DataIn total, 164 right eyes met the inclusion and exclusion criteria. Among them, 36 males and 128 females were included, with a mean age of 25.11±5.69. The SE was ‐9.25±2.10 D. AL was 26.99±1.11 mm. IVD was 54.04%±4.94%, and PVD was 49.81%±3.24% (Table 1).
Microcirculation Changes of Optic Nerve Head in Different Age GroupsNo significant difference was observed in the IVD or PVD among the Age1, Age2, and Age3 groups(P>0.05). However, with the increase of age, the IVD and PVD decreased (Table 2).
Microcirculation Changes of Optic Nerve Head in Different Spherical Equivalent GroupsNo significant difference was observed in the IVD or PVD among the SE1, SE2, and SE3 groups (P>0.05; Table 3).
Microcirculation Changes of Optic Nerve Head in DifferentAxial Length GroupsNo significant difference was observed in the IVD among AL1, AL2, AL3, and AL4 groups (P>0.05).In contrast, PVD in AL1, AL2, and AL3 groups was higher than in the AL4 group (P<0.05). Among 8 regions of PVD, the NI, IT, TI, and TS regions were significantly different (P<0.05).The temporal direction was higher than that of the nasal direction. However, IVD did not change significantly with AL growth (Table 4, Figure 2).

Figure 1 Parameters by optical coherence tomography angiography.
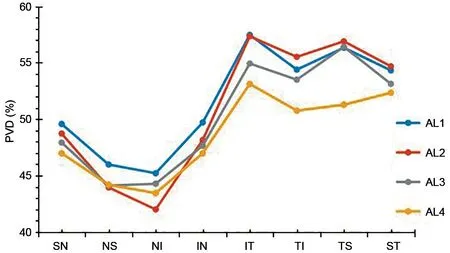
Figure 2 Peripapillary vascular density in eight sectors of different axial length groups.

Table 1 Clinical characteristics of the patients mean±SD
Correlation AnalysisIVD was negatively correlated with age (r=‐0.190,P=0.042) but was not correlated with AL(r=0.145,P=0.063) or SE (r=0.088,P=0.263). PVD had a significant negative correlation with AL (r=‐0.236,P=0.002;Figure 3) but was not correlated with age (r=0.042,P=0.597)or SE (r=‐0.047,P=0.550).
DISCUSSION

Table 2 Microcirculation changes of optic nerve head in different age groups mean±SD

Table 3 Microcirculation changes of optic nerve head in different SE groups mean±SD

Table 4 Microcirculation changes of optic nerve head in different AL groups mean±SD
In this study, we analyzed the vessel density parameters of ONH in HM, and found that the PVD decreased with AL elongation, while the IVD remained stable.The ONH is a conspicuous structure with optic nerve and retinal vessels entering or exiting the eyeball. In concurrence with previous reports, this study also observed that the PVD decreases with the growth of the AL[10‐12]. Importantly,two mechanisms may lead to a decrease in perfusion in the peripapillary region of the HM. First, the growth of the eyeball leads to the expansion and thinning of the retina, especially around the optic disc[13], resulting in a decrease in the vascular tissue per unit area. Al‐Sheikhet al[14]and Milaniet al[15]reported that the retinal vessel density in the macular area of myopia patients was significantly decreased. Moreover,the excessive axial elongation resulted in straightening and stenosis of blood vessels, causing an overall decrease in vessel density. Second, the possible mechanism of thinning in the peridiscal retinal tissue decreases the oxygen demand,which further causes a decrease in blood circulation[16‐17]. To a certain extent, the supply‐demand relationship explains that the decrease in vessel density in HM is a physiological rather than a pathological phenomenon. Further, previous studies have reported thinning of the retinal nerve fiber layer in HM[18‐20], which may reduce oxygen and blood flow demand.In this study, the PVD on the temporal side (IT, TI, TS, and ST) was higher than on the nasal side (SN, NS, NI, and IN).Of note, when AL was greater than 28 mm, the three regions of temporal PVD (IT, TI, and TS) were significantly reduced.These findings are in coherence with our morphological studies on the ONH. Thus, as AL elongates, the morphological changes on the temporal side of the ONH significantly increase compared to the nasal side. This observation indicates that there may be a relation between the morphological structure of the peripapillary area and PVD in HM, which needs to be explored further.
Our study revealed that the IVD (54.04%±4.94%) was greater than the PVD (49.81%±3.24%) in HM. In contrast to PVD,with the increase of AL, IVD remained stable. To date, no relevant research has been performed on this topic. The blood supplied to the optic disc is complex, mainly provided by retinal and choroidal circulations. The Zinn‐Haller arterial ring provides the main blood supply to the optic disc at the level of the lamina. However, as AL increases, the distance between the Zinn‐Haller and the optic disc boundary increases significantly[21‐22]. Therefore, the different changes in IVD and PVD might occur due to the inside and peripapillary blood supply provided by different blood circulations.
Additionally, in another possible mechanism, changes in the ONH are mainly focused on the peripapillary area. Thus, blood perfusion is compensated by increasing the disc area while the IVD remains stable for preserving the optic nerve tissue. This mechanism may explain why not all high myopia eyes undergo optic nerve degenerative pathological changes.
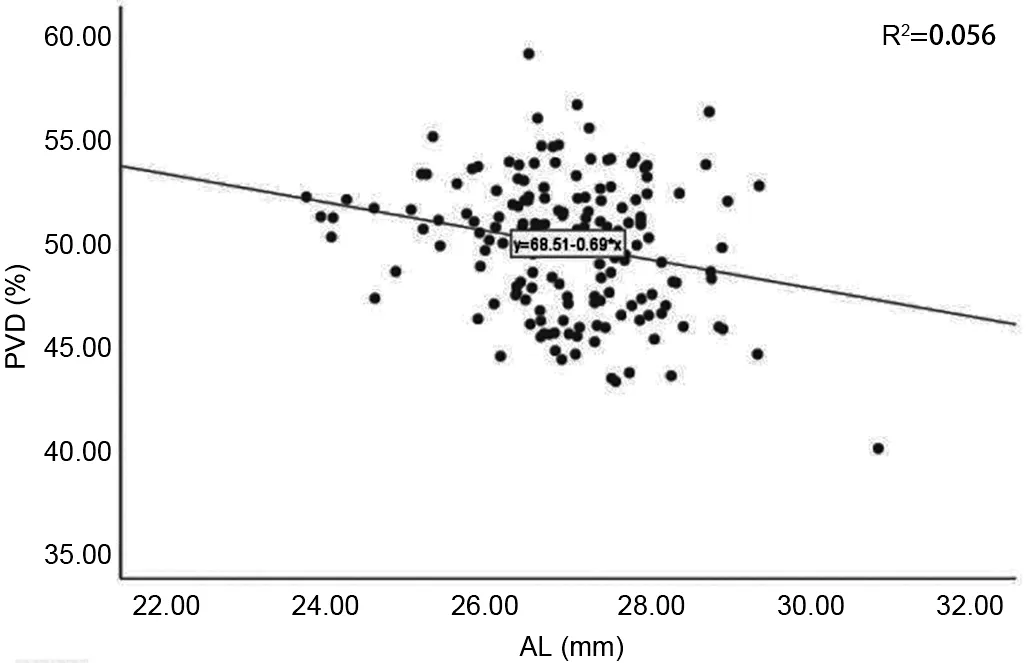
Figure 3 The correlation between peripapillary vascular density and axial length.
Previous studies have shown that SE was significantly correlated with changes in retinal microvessels[23]. On the contrary, our results suggest that the SE does not correlate with ONH vessel density. The SE is mainly determined by various components of the anterior and posterior segments,including the eyeball’s corneal curvature, lens, and AL. Axial elongation is generally the result of structural changes in the posterior segment. Nonetheless, the mechanical stretching caused by axial elongation is usually accompanied by a reduction in oxygen consumption, eventually affecting the structure of the posterior segment[24‐25], such as the retina[26].Although not completely equivalent, AL and SE changes occur almost simultaneously during the development of HM[27].In this study, we found that the relationship between vessel density and AL was more profound than between vessel density and SE. Therefore, in clinical diagnosis and treatment,ophthalmologists and myopia patients should pay more attention to axial elongation and not just refractive changes.In addition, we found that the ONH vessel density did not show a significant change with the increase in age, which was in agreement with the previous findings of Liuet al[23]. They reported that in the age of 18‐45y, the vessel density in the macular region was relatively unaffected by age. However, this finding was inconsistent with the conclusion of Weiet al[28], who studied people between 18 and 82 years of age. They found that only those aged 65y or older had a significant decrease in vessel density. Lenget al[29]found that with the increase in age, the vessel density of macula decreased significantly,while the vessel density of macula did not correlate with sex,race, SE, or AL. The findings of these studies were contrary to our conclusions. The reasons could be the differences in the clinical characteristics of the study population, inclusion, and image analysis criteria. Yuet al[30]reported that in a healthy Chinese population, the blood flow index and vessel density of the superficial macular parafoveal decreases with age with constant decreases of 0.6% (blood flow index) and 0.4% (vessel density) each year. Therefore, it is critical to conduct future studies in larger cohorts to clarify and validate the potential impact of age on retinal perfusion in HM.
The study had certain limitations. First, this was a retrospective study; hence, longitudinal data were unavailable. Thus, the causality of the conclusion cannot be confirmed. Second, an OCTA scan requires the subjects to maintain a stable position and fixation; however, elderly patients with refractive interstitial opacity or poor fixation can’t receive accurate measurements.The subjects were young to middle‐aged; thus, we could obtain satisfactory image quality under full guidance with the credibility of the results. Further, a sample selection bias also occurred to some extent. Third, the magnification effect of the images may affect the results of OCT measurements (e.g.,vessel density, and area). The range of 4.5×4.5 mm2scans used in this study was small, so the effect of the amplification effect was not significant.
In conclusion, in HM, IVD, and PVD did not change significantly with an increase in age or SE. However, with the increase in AL, the IVD remained stable, but the PVD decreased, especially in the three temporal regions (IT, TI, and TS). The PVD was negatively correlated with AL. In young patients, the SE and age were not significantly correlated with ONH vessel density. Therefore, ophthalmologists and myopia patients should pay attention to AL elongation, not merely to refractive changes. The asymmetric changes in IVD and PVD may explain why not all HM patients undergo optic nerve degenerative pathological changes.
ACKNOWLEDGEMENTS
Authors’ contributions:Tang WQ and Duan XC designed the research study; Tang WQ wrote the paper; Tang WQ, Luo YL, and Wang XL analyzed and interpreted the data; Duan XC, Luo YL and Wang XL contributed to critical revision of the article; Duan XC and Luo YL obtained and provided administrative, technical, or logistic support. All authors approved the manuscript.
Foundations:Supported by National Natural Science Foundation of China (No.81970801); Health Commission of Hunan Province (No.202107020468; No.202107021955).
Conflicts of Interest: Tang WQ,None;Luo YL,None;Wang XL,None;Duan XC,None.
 International Journal of Ophthalmology2023年1期
International Journal of Ophthalmology2023年1期
- International Journal of Ophthalmology的其它文章
- Visual perception alterations in COVID-19: a preliminary study
- COVID-19 pandemic impact on ocular trauma in a tertiary hospital
- Apolipoprotein A1 suppresses the hypoxia-induced angiogenesis of human retinal endothelial cells by targeting PlGF
- Comparison of vegetable oils on the uptake of lutein and zeaxanthin by ARPE-19 cells
- Identifying a novel frameshift pathogenic variant in a Chinese family with neurofibromatosis type 1 and review of literature
- Recurrence risk factors of intravitreal ranibizumab monotherapy in retinopathy of prematurity: a retrospective study at one center
