Sarcopenia affects the treatment and prognosis of colorectal cancer
Neng-Liang Zhang, Chun-Lei Qian, Jian-Hua Wang*Clinical Medical College of Dali University, Dali 67000, China.Department of Oncology, The First Affiliated Hospital of Dali University, Dali 67000, China.
Abstract Sarcopenia is a common complication of malnutrition.Patients with colorectal cancer are prone to secondary sarcopenia due to nutrient absorption, intestinal obstruction, metabolic disorders and other reasons.Nutritional status not only participates in the body’s normal function but also has an important impact on anti-tumor treatment.More and more evidence shows that sarcopenia has a negative effect on the treatment and prognosis of colorectal cancer.This article summarizes the related research, such as the influence of sarcopenia on the treatment of colorectal cancer.To evaluate the clinical value of sarcopenia in treating colorectal cancer and provide new ideas for the comprehensive treatment of sarcopenia in patients with colorectal cancer.
Keywords: sarcopenia; colorectal cancer; early screening; review
Background
Sarcopenia atrophy is a degenerative disease characterized by progressive loss of muscle mass and function [1].First described by Rosenberg in 1989 [2].Sarcopenia is common in the elderly and can be caused by many factors, such as malignant tumors, malnutrition,chronic renal failure and chronic obstructive pulmonary disease.It can increase the incidence of adverse events, such as falls, fractures,weakness and death [3].In 2020, the number of new cases and deaths of colorectal cancer in the world ranked third and second, respectively[4].Therefore, it has brought a heavy economic and psychological burden to patients.Secondary sarcopenia is common in malignant tumors, organ dysfunction and other diseases.The decline of muscle mass and function in cancer-related sarcopenia is related to reduced nutritional intake, systemic inflammatory response and complications[5].The prevalence of sarcopenia in patients with colorectal cancer ranges between 12-60% [6-8].A preliminary study of sarcopenia in patients with colorectal cancer has found a possible correlation between sarcopenia and prognosis in patients with colorectal cancer undergoing surgery [9].In neoadjuvant therapy, previous studies have suggested that muscle loss is related to the dose-limiting toxicity of chemotherapeutic drugs for colorectal cancer [10].In recent years,there has been evidence that targeted drugs such as bevacizumab can also cause muscle loss, which has a negative impact on the prognosis of patients with advanced colorectal cancer [11, 12].In view of the clinical value of sarcopenia in the treatment of colorectal cancer, this paper reviews the definition and diagnosis of sarcopenia and its influence on the treatment and prognosis of colorectal cancer.To provide an empirical basis for subsequent screening and management of sarcopenia.
Definition
The word “sarcopenia” comes from the Greek words “sarx” and“penia”, meaning “physical reduction”.It was first described as an age-related decrease in muscle mass, nutritional status and standard of living [2].In 2016, the International Classification of Diseases identified sarcopenia as an independent disease; this marks that the medical community officially regards it as a disease with independent characteristics [13].The European Working Group on Sarcopenia in Older People (EWGSOP) proposed the most widely cited definition of sarcopenia and updated it to EWGSOP2 in 2018 [14, 15].The EWGSOP2 stipulates that people with low muscle strength, muscle mass or mass will be diagnosed with sarcopenia.
Pathophysiology
Every skeletal muscle is a complex organ that participates in the functions of motion production, nerve conduction, metabolism,hormone secretion and so on.The pathological changes of sarcopenia are mainly the metabolic disorder of skeletal muscle, which affects the synthesis and degradation of protein and glycogen, resulting in muscle fiber atrophy, thus weakening muscle strength and regenerative function [16, 17].In addition, the interaction between fat and muscle tissue is an essential factor leading to sarcopenia.Lex et al.proposed that muscle fibers gradually atrophy with age, and fat infiltrates into muscle tissue [18].Excessive fat will produce endotoxin and aggravate muscle loss.Studies have confirmed that lipids deposited in muscle cells can further promote lipotoxicity and lead to mitochondrial dysfunction, oxidative stress, inflammation, etc.And ultimately lead to decreased muscle renewal and increased fat infiltration; this vicious circle is called visceral obesity [19].Cross-talk between muscle and fat is mediated through endocrine factors.The accumulation of fat in abdomen and viscera of postmenopausal women is related to the imbalance of secretion of growth hormone,testosterone, thyroid hormone and insulin-like growth factor,accompanied by the decline of muscle mass and function [20].With the increase of age, the secretion of pro-inflammatory factors increases, and the secretion of pro-inflammatory factors such as tumor necrosis factor-α and interleukin-6 will lead to the decrease of muscle fiber synthesis, while sarcopenia will aggravate the inflammatory process [21].This metabolic disorder is age-related, ageing disturbs the homeostasis of skeletal muscle.It can be seen that sarcopenia is a multi-etiological, multi-mechanism complex disease.
Evaluation and diagnosis
In 2018, EWGSOP2 put forward the diagnosis process of sarcope nia: finding cases, evaluating, diagnosing and grading severity [1 5].The updated EWGSOP2 proposed a stepwise approach to diag nosis (Figure 1).First of all, muscle strength was evaluated by th e self-evaluation questionnaire of SARC-F (including strength (S),assisted walking (A), rising from a chair (R), climbing stairs (C),and falls (F)).According to the patient’s answers, the score of ea ch item was 0-2, and finally, the total score was added, ≥4 poi nts indicated the risk group of sarcopenia.In the second step, m uscle strength was determined by grip strength test (normal male grip strength ≥ 27 kg, female grip strength ≥ 16 kg) and 5 sit-up tests (≤ 15 seconds for normal men and women for 5 conse cutive times).Abnormal patients were assigned to perform dual-e nergy X-ray absorptiometry to analyze muscle mass, that is, the t hird step.In clinical work, dual-energy X-ray absorptiometry, bio electrical impedance measurement and computerized tomography(CT) is recommended [22].With the deepening of the study, CT can quantify muscle area, while colorectal cancer patients also m onitor tumor growth through CT, so this imaging method is very suitable for quantitative muscle mass in clinical work.It is wort h noting that the third step is the diagnosis step; if there is a de cline in skeletal muscle mass can be clearly diagnosed as sarcope nia, so in many clinical studies, researchers often directly throug h CT and other examinations to determine whether the experime ntal group has sarcopenia if it is diagnosed as sarcopenia.In 201 6, Barbosa et al.added calf circumference to the SARC-F questio nnaire (male < 34 cm, female < 33 cm indicates that sarcopeni a was positive), namely SARC-CalF questionnaire.Compared with SARC-F questionnaire, SARC-CalF questionnaire has higher sensit ivity [23].Compared with CT and other instrument testing meth ods, SARC-CalF questionnaire is more suitable for community scre ening and home self-test.
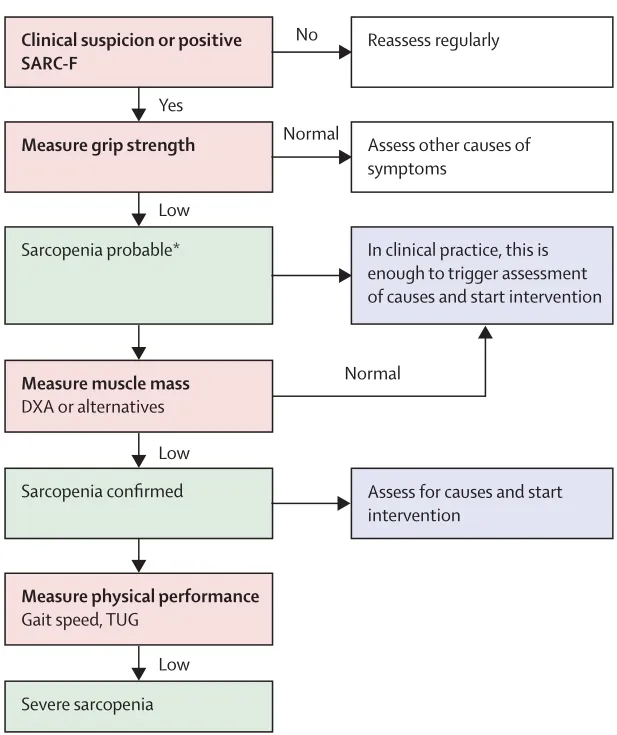
Figure 1 A simple algorithm to diagnose sarcopenia
Sarcopenia and the treatment of Colorectal Cancer
According to different stages, patients with colorectal cancer can choose surgery, neoadjuvant therapy (that is, preoperative treatment for patients with decent tumors, including chemotherapy, targeted therapy and radiotherapy) and immunotherapy.Its treatment is affected by nutrition, metabolism, drugs and other factors.In 2019,EWGSOP2 proposed that sarcopenia is a muscle exhaustion disease that increases the risk of adverse clinical outcomes [15].Previous studies have shown that body composition and functional status are important factors related to the prognosis of patients, and weight loss and muscle mass loss may affect the prognosis of tumors [24].The following describes the influence of sarcopenia on different treatments for colorectal cancer.
Surgery
Surgery is the primary treatment for early digestive tract tumors,including colorectal cancer.Sarcopenia is closely related to many adverse clinical outcomes in the perioperative period of colorectal cancer, such as increased postoperative complications, prolonged hospital stay, increased hospitalization costs and so on [25].Sarcopenia can be used as a predictor of perioperative complications.A large number of studies have found that changes in body composition parameters, such as decreased skeletal muscle mass and increased visceral adipose tissue have adverse effects on the outcome of patients undergoing gastrointestinal tumor surgery [26-28].Japanese scholars studied the relationship between 494 cases of colorectal cancer patients and sarcopenia.Multivariate regression analysis showed that sarcopenia was an independent risk factor for the total incidence of postoperative complications of colorectal cancer.Colorectal cancer patients with sarcopenia have an increased risk of infection at the non-operative site [29].The reason may be the decrease of muscle mass and the decrease of interleukin-15, which was originally highly expressed in muscle tissue, resulting in a decrease in natural killer cell activity and a decrease in immunity[30].Mario et al.found that sarcopenia is a powerful predictor of worse survival in patients with colorectal cancer by comparing the postoperative outcome and survival rate between the non-sarcopenia r group and the sarcopenia group [31].Lorena et al.analyzed progression free survival and overall survival (OS) in 72 stages IV colorectal cancer patients.The results showed that sarcopenia had a negative effect on progression free survival and OS of colorectal cancer, and sarcopenia was an independent prognostic factor for metastatic colorectal cancer [32].Preoperative and postoperative sarcopenia may adversely affect the prognosis of colorectal cancer surgery [33].Careful attention should be given to correcting sarcopenia status from the preoperative to the postoperative period.These studies suggest that sarcopenia has obvious negative effect on the postoperative prognosis of patients with colorectal cancer,including increasing the incidence of postoperative complications,increasing mortality rate and reducing the survival time of patients.Clinicians must be aware of the existence of sarcopenia to identify this risk factor in colorectal cancer surgery.In the future perioperative period of colorectal cancer patients, early screening and timely intervention for sarcopenia will help improve the effect of surgical treatment and prognosis of colorectal cancer patients.
Chemotherapy and targeted therapy
A variety of different schemes composed of chemotherapeutic drugs combined with targeted therapy are the main treatment for colorectal cancer in addition to surgery.Side effects of oxaliplatin include reduced nutritional intake and reduced physical activity.Clinical studies evidence from animal studies suggests that oxaliplatin may cause skeletal muscle damage by targeting mitochondria, leading to sarcopenia [34].Chemotherapy leads to a decrease of muscle mass,and muscle loss increases the adverse events of chemotherapy drugs.The high incidence of clinical adverse events will lead the doctors to reduce the chemotherapy dose, stop taking drugs or delay chemotherapy.Insufficient chemotherapy will lead to tumor progression and affect prognosis.This seems to have formed a vicious circle.David et al.found that OS was lower in patients with sarcopenia after first-line chemotherapy in patients with metastatic colorectal cancer, and patients with sarcopenia showed more severe restrictive adverse reactions [35].Some studies have confirmed that sarcopenia is an independent negative prognostic factor in patients with advanced neoadjuvant chemotherapy for rectal cancer [36].Traditional chemotherapeutic drug dose calculation multi-reference body surface area and other indicators but not included in the muscle mass.In view of the effect of muscle mass on the side effects of chemotherapeutic drugs, muscle mass may be included in the reference index in the future.To establish a more scientific formula for calculating the dosage of chemotherapy drugs.Targeted therapy is suitable for patients with colorectal cancer with genetic mutation.In the treatment of advanced colorectal cancer, chemotherapy drugs are usually combined with targeted drugs.Bevacizumab is a targeted anti-angiogenesis drug which is commonly used in metastatic colorectal cancer.In patients with metastatic colorectal cancer treated with bevacizumab, Adeline et al.evaluated changes in muscle mass over 70 days and found that 47% of patients showed loss of skeletal muscle mass [37].In the study of regofenil, another oral targeted drug, it has been shown that the dose-limiting toxicity of regofenil is significantly increased in patients with metastatic colorectal cancer accompanied by sarcopenia.Still, it has no significant correlation with the overall survival and progression-free survival of the patients [38].At present, there is little evidence about whether various targeted drugs will affect the therapeutic effect of colorectal cancer patients with sarcopenia, and more research is needed in the future.It can be seen that sarcopenia significantly increases the toxicity and side effects of chemotherapy and reduces the tolerance of patients with colorectal cancer to high-intensity chemotherapy.
Radiotherapy and Immunotherapy
Radiotherapy for colorectal cancer is mainly focused on neoadjuvant therapy for colorectal cancer.In 2018, a cohort study showed that low muscle mass and low muscle radioactivity density were risk factors for mortality in patients with stage I-III colorectal cancer [39].In 2021,Shinya evaluated the muscle mass of 234 patients with advanced rectal cancer who received a long course of radiotherapy.It was found that sarcopenia was a poor prognosis index for patients with low advanced rectal cancer who received radiotherapy and chemotherapy[40].Radiotherapy-induced interleukin-6 may be responsible for tumor growth and therapeutic resistance, resulting in an adverse prognosis [41].At present, most of the related results come from clinical observation, and the research on the pathogenesis of skeletal muscle loss caused by radiotherapy is not in-depth.Immunotherapy is a new treatment method to achieve anti-tumor effects by restoring the normal anti-tumor immune response of the body.There is little information about neoadjuvant therapy of colorectal cancer.In 2021,Takenaka and others found that sarcopenia was negatively correlated with the efficacy of immunotherapy through systematic review and meta-analysis, and sarcopenia could predict the poor prognosis of immunotherapy [42].Summing up the above studies, it can be found that no matter what kind of treatment is used for colorectal cancer,sarcopenia is one of the risk factors for poor prognosis.It is suggested that screening for sarcopenia in patients with colorectal cancer before treatment may have a certain clinical significance in reducing treatment complications, improving treatment effects and improving the prognosis of patients.
Treatment of sarcopenia
At present, there is no guidelines to recommend the treatment of patients with colorectal cancer with sarcopenia.The treatment of sarcopenia includes non-pharmacological approaches and pharmacological approaches.In view of the close relationship between sarcopenia and nutrition, exercise and other factors, patients with colorectal cancer are often accompanied by problems such as malnutrition, chronic consumption and reduced exercise, so the treatment of sarcopenia can start with strengthening exercise and nutrition supplement.In 2018, evidence-based clinical practice guidelines were published and provide recommendations for physical activity as the treatment of sarcopenia [43].Lack of physical exercise is an identified risk factor for sarcopenia, and the protective mechanism of exercise on skeletal muscle is not completely clear,which may be related to the fact that physical exercise can increase exercise units and down-regulate the expression of pro-inflammatory factors [44].Mello et al.compared the characteristics of muscle reduction in the elderly with and without exercise intervention, and found that muscle mass and muscle function were improved in the experimental group with resistance exercise training [45].On the other hand, nutrition and eating strategies also play an essential role.The practice of rehabilitation nutrition can improve function and activities of daily living in cases of sarcopenia [46].Evidence-based clinical practice guidelines strongly recommend conditionally protein supplementation/a protein-rich diet, no recommendation is given for Vitamin D supplementation or for synthetic hormone drug [43].Nutrition therapy should be performed in combination with physical exercise.Studies have shown that taking leucine-rich branched-chain amino acids/low enriched uranium supplements can activate the signal pathway of rapamycin target protein,promote protein synthesis,and improve tumor prognosis [46].Some evidence to suggest that perindopril and espindolol may improve muscle function[47].There is inadequate data to recommend these drugs for the treatment of sarcopenia.With regard to the research and development of drugs for the treatment of sarcopenia, several drugs have entered the III phase trial, including selective androgen receptor regulation and targeted sarcopenia activation pathway [48].We believe that in the near future, the related drugs will be gradually applied to clinical practice.
Discussion
To sum up, the incidence of sarcopenia is high in patients with colorectal cancer, and many studies have confirmed that sarcopenia will have a negative impact on the treatment and prognosis of colorectal cancer.However, the pathogenesis of sarcopenia is not completely clear, and there is no scientific treatment for tumor-associated sarcopenia.Because of this, in the future, we should strengthen the understanding of sarcopenia in patients with colorectal cancer, incorporate the screening of sarcopenia in the pre-treatment evaluation of colorectal cancer, identify and formulate individualized treatment plans at an early stage, strengthen the rehabilitation and follow-up of patients with sarcopenia, and achieve early intervention,timely treatment and continuous care.To improve the prognosis and quality of life of colorectal cancer patients.