Intraoperative pancreas stump perfusion assessment during pancreaticoduodenectomy: A systematic scoping review
Francis P Robertson, Harry V M Spiers, Wei Boon Lim, Benjamin Loveday, Keith Roberts, Sanjay Pandanaboyana
Abstract
Key Words: Pancreatico-duodenectomy; Post-operative pancreatic fistula; Perfusion; Indocyanine green; Post pancreatectomy pancreatitis
INTRODUCTION
Pancreatic resection is a key component in the treatment pathways of various benign and malignant diseases[1]. The postoperative morbidity after pancreatic resection remains high despite centralisation[2,3] and improved surgical techniques[4]. Post-operative pancreatic fistula (POPF), serves as the key risk factor for other post-operative intraabdominal complications such as delayed gastric emptying (DGE) and intraabdominal collections[5-7], thereby prolonging hospital stay and increasing over all morbidity[8-11]. Furthermore, POPF is the root cause of mortality after pancreaticoduodenectomy[12,13]. Risk factors for POPF are very well defined[14]. Despite numerous trials aimed at reducing the incidence of POPF, its incidence has remained largely unchanged over decades[15]. This is likely due to poor understanding of the underlying pathophysiology, with failure of current interventions to reduce POPF suggesting something more than a mere loss of mechanical anastomotic integrity. One theory is that hypoperfusion of the pancreatic remnant results in pancreas transection margin ischaemia, necrosis and post pancreatectomy pancreatitis with subsequent failure of healing at the pancreatico-enteric anastomosis and resultant pancreatic leak[16-18]. The neck of the pancreas is a watershed area between coeliac and superior mesenteric arterial systems, hence, hypoperfusion in this area may be associated with poor healing and risk of anastomotic leak[15].
There is some evidence from the literature on intraoperative pancreas perfusion assessment and there is a need to identify and map the current evidence for its use in the context of POPF. This will allow identification of techniques used and provide insight into their effectiveness, paving the way for further prospective and randomised studies. Therefore,this scoping review aims to define the current experience with intraoperative pancreas perfusion assessment and highlight the published literature surrounding pancreas stump hypoperfusion as a potential risk factor for POPF.
MATERIALS AND METHODS
This scoping review was performed according to the Preferred Reporting Items for Systematic Reviews and Metaanalyses Scoping Reviews extension[19]. The study protocol was prospectively registered with the University of York Centre for Review and Dissemination international prospective register of systematic reviews PROSPERO database (2021:CRD42021296863).
Following pilot testing, a systematic search of Medline and EMBASE databases was conducted on 8thNovember 2022,with screening performed by two independent investigators (HS and FR). The search strategy was conducted using the following search algorithm: ((pancreatic fistula.ti.ab) OR (exp pancreatic fistula) OR (anastomotic leak.ti.ab) OR (exp anastomotic leak)) AND ((pancreatoduodenectomy.ti.ab) OR (exp pancreatoduodenectomy) OR (pancreaticoduodenectomy.ti.ab) OR (exp pancreatoduodenectomy) OR (Whipple’s surgery.ti.ab)) AND ((perfusion.ti.ab) OR (exp perfusion)OR (blood supply.ti.ab) OR (exp blood supply). All studies including patients undergoing pancreaticoduodenectomy were included. Full search strategy and results are presented in Supplementary Table 1. Titles identified following this literature search were entered into theReference Citation Analysis(RCA) (Baishideng Publishing Group) to search for further studies related to these articles.
Inclusion and exclusion criteria
Full text studies reporting patients undergoing intraoperative pancreas perfusion assessment, or correlating hypoperfusion with POPF were included regardless of language. Any type of publication reporting primary data on the topic was included. Review articles and studies not reporting primary data were excluded. After excluding duplicates, two researchers (Robertson FP and Spiers HVM) independently reviewed the titles and abstracts of studies identified by the literature search. Where a study was considered relevant to the research question a full copy of the publication was obtained for further review. The reference lists of included articles were hand-searched for any further relevant studies.Any areas of disagreement between the two primary researchers were resolved through discussion with the senior author(Pandanaboyana S).
Data extraction
Data were retrieved from published studies and extraction was performed by an individual author (Spiers HVM) and independently checked by a second author (Robertson FP), with any disagreement resolved by consensus or where necessary with a senior author (Pandanaboyana S). The post-operative outcomes chosen to explore were the development and grade of POPF as defined by the International Study Group of Pancreatic Surgery (ISGPS)[20], the incidence of postpancreatectomy haemorrhage, grade of DGE as defined by the ISGPS[21,22] and mortality. Study quality was not formally assessed as this is a scoping review.
RESULTS
Following the initial search (Figure 1), 90 studies were identified of which 74 remained following removal of duplicates.The 74 titles and abstracts were reviewed and 9 studies were selected for full review. Studies were excluded when not relevant, or non-primary literature. Of the 9 studies reviewed in detail, 4 were excluded because of operative procedure performed not being pancreaticoduodenectomy, conference abstract only or pancreas perfusion assessment not performed intraoperatively. Five studies including 156 patients were included in the final review. The median number of patients included in each study was 30 (1-123). Characteristics of the included studies are shown in Table 1.
Patient demographics
Studies were published between 2002 and 2021 and included three case reports of a single patient and two prospective non-randomised cohort studies. One hundred and fifty-six patients underwent pancreaticoduodenectomy, two of which were laparoscopic, the rest open. One hundred and forty patients (90%) underwent resection for malignancy and 16 (10%)underwent resection for chronic pancreatitis. Three studies included only patients undergoing pancreaticoduodenectomy with no vascular resection or resection of other organs[23-25]. One study included a patient undergoing open pancreaticoduodenectomy combined with distal pancreatectomy and splenectomy (middle segment-preserving pancreatectomy)[26]. One study included 10 patients undergoing vascular resection[27], 3 patients undergoing simultaneous vascular and arterial resection and 3 patients undergoing synchronous resection of other organs [partial splenectomy (n=1), partial nephrectomy (n= 1), minor hepatectomy (n= 2)].
Technical details of pancreas perfusion and assessment
In 4 studies pancreas perfusion was measured by intravenous injection of indocyanine green (ICG) into a peripheral vein allowing intra-operative fluorescence angiography under near infrared light[23,24,26,27] (Table 2). Adequate pancreatic perfusion was classified by Doussotet al[27] as homogonous perfusion of the pancreatic stump. Time to achieve this was also measured and divided into 3 groups (< 30 s, 30-60 s and > 60 s). One study assessed pancreas perfusion by visual inspection of arterial bleeding of the pancreatic stump following transection of the pancreatic neck[25]. Perfusion was classified as adequate when brisk arterial pulsatile bleeding was visualised superiorly and inferiorly to the pancreatic duct that required sutures to control the bleeding.
When pancreatic hypoperfusion was identified in the study by Strasberget al[25], the pancreatic margin was cut back further by 1.5-2.0 cm until improved perfusion was visualised. Similarly, when hypoperfusion was identified in the study by Subaret al[24], further cut back of the margin was performed. In the study by Doussotet al[27], the pancreatic stump was only further cut back in one patient. The results of pancreatic perfusion in the case study by Rhoet al[23] did not alter the operative strategy. Prophylactic octreotide was administered variably throughout the studies.
Outcomes
Perfusion of the pancreatic stump was assessed successfully in all patients recruited to the studies. Perfusion of the pancreatic stump was assessed by ICG angiography in 33 patients and visual inspection of bleeding from the cut surface in 123 patients. Hypoperfusion of the pancreatic stump was identified in 55 (35%) of patients (Subaret al[24]n= 1,Doussotet al[27]n= 6, Rhoet al[23]n= 1, Strasberget al[25]n= 47). Of these patients 49 (89%) underwent further cutback of the pancreatic stump prior to formation of the pancreatico-jejunostomy. Two patients in the study of Strasberget al[25]who had their stump cut back were found to still exhibit signs of hypoperfusion within their criteria.
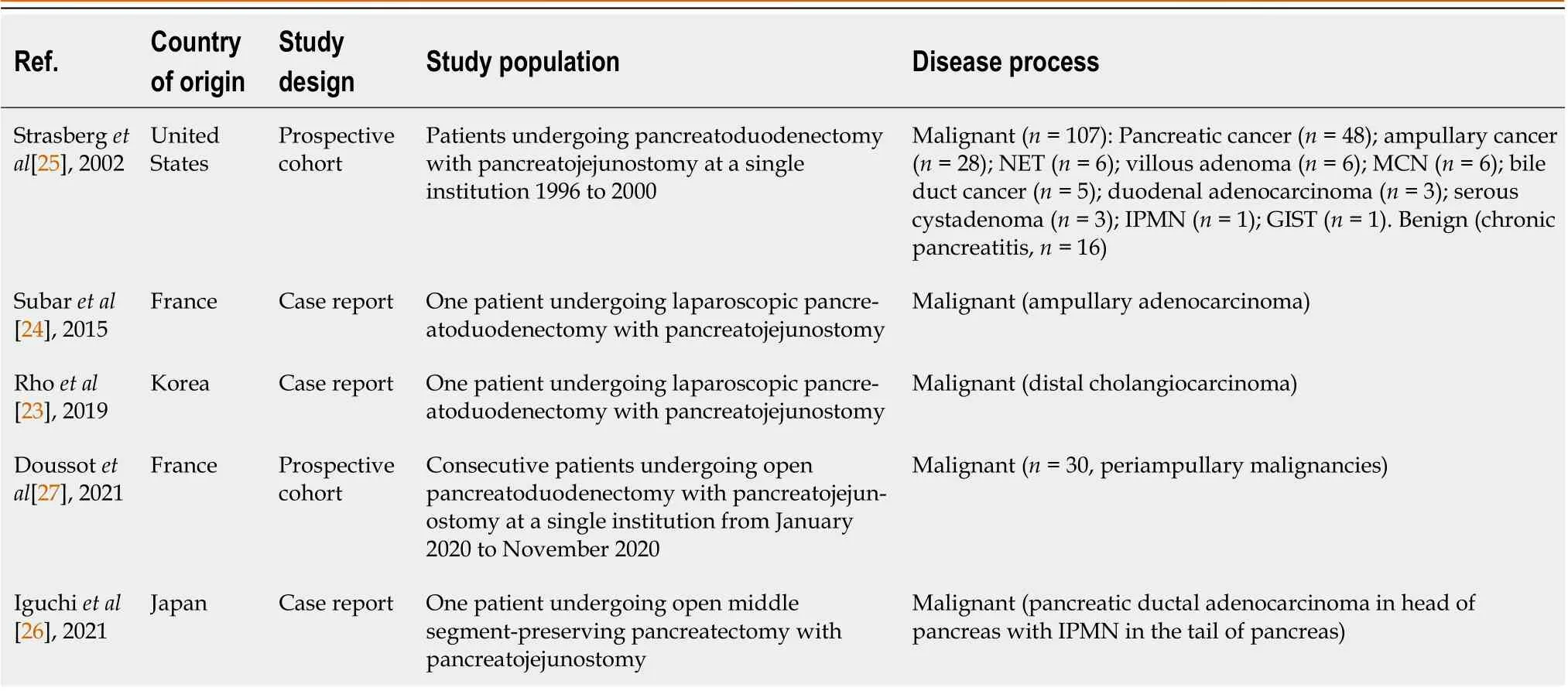
Table 1 Study characteristics of included articles
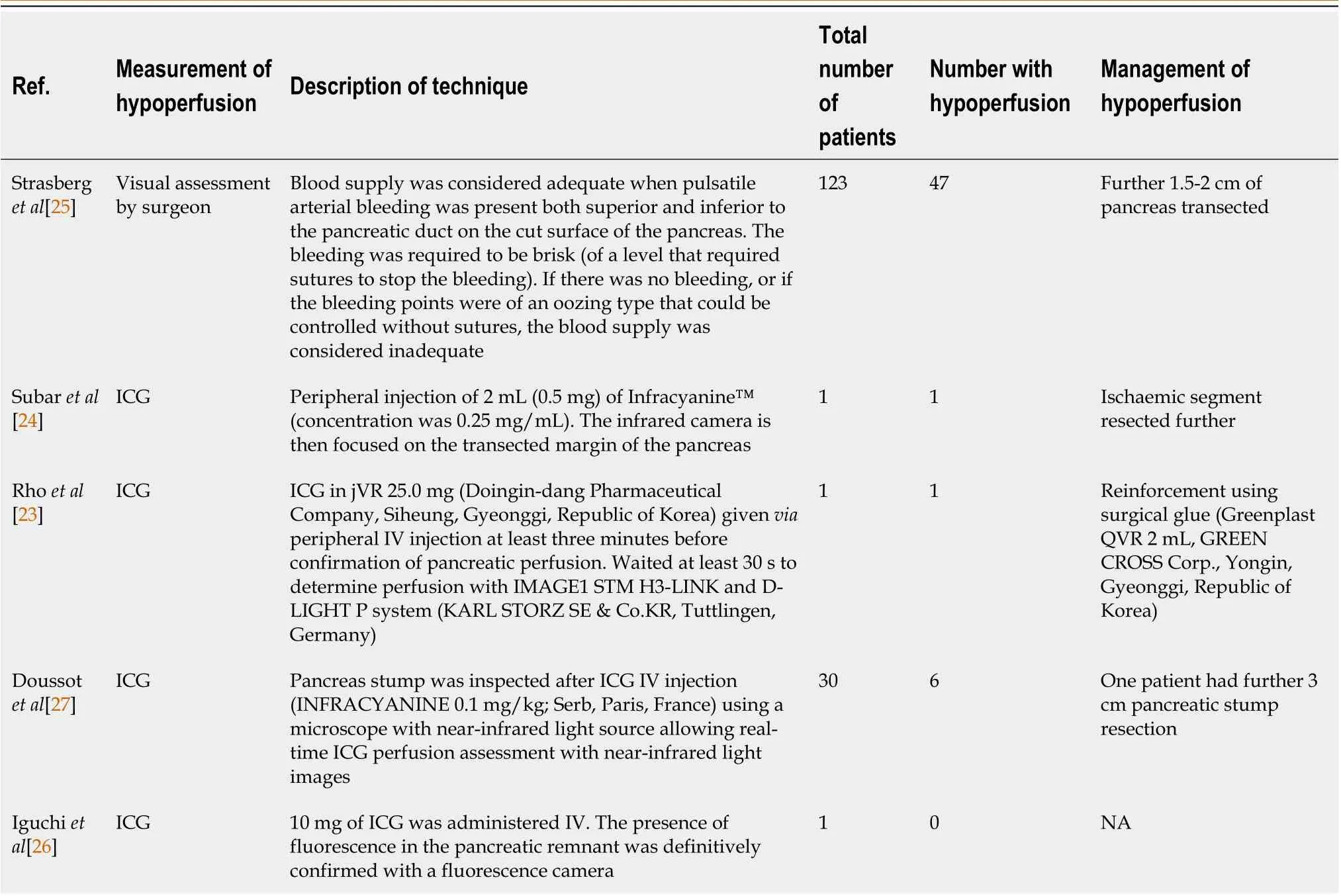
Table 2 Intraoperative perfusion assessment and management of hypoperfusion
The definition of POPF was heterogeneously defined between the studies. Strasberget al[25], which was published in 2002 prior to the ISGPS publication of the consensus definition of POPF in 2016, defined POPF as drainage of > 50 mL of pancreatic fluid (> 500 IU/L) for 3 consecutive days as long as it included post-operative day 10. There was no subclassification of clinically relevant POPFvsbiochemical leak in the study by Strasberget al[25]. All other studies defined POPF according to the ISPG classification. DGE was defined in the study by Rhoet al[23] according to the ISGPS definition.Neither Doussotet al[27] nor Strasberget al[25] clarified their definition of DGE. Post-pancreatectomy haemorrhage was measured in the study by Doussotet al[27] and was classified according to the ISGPS definition.
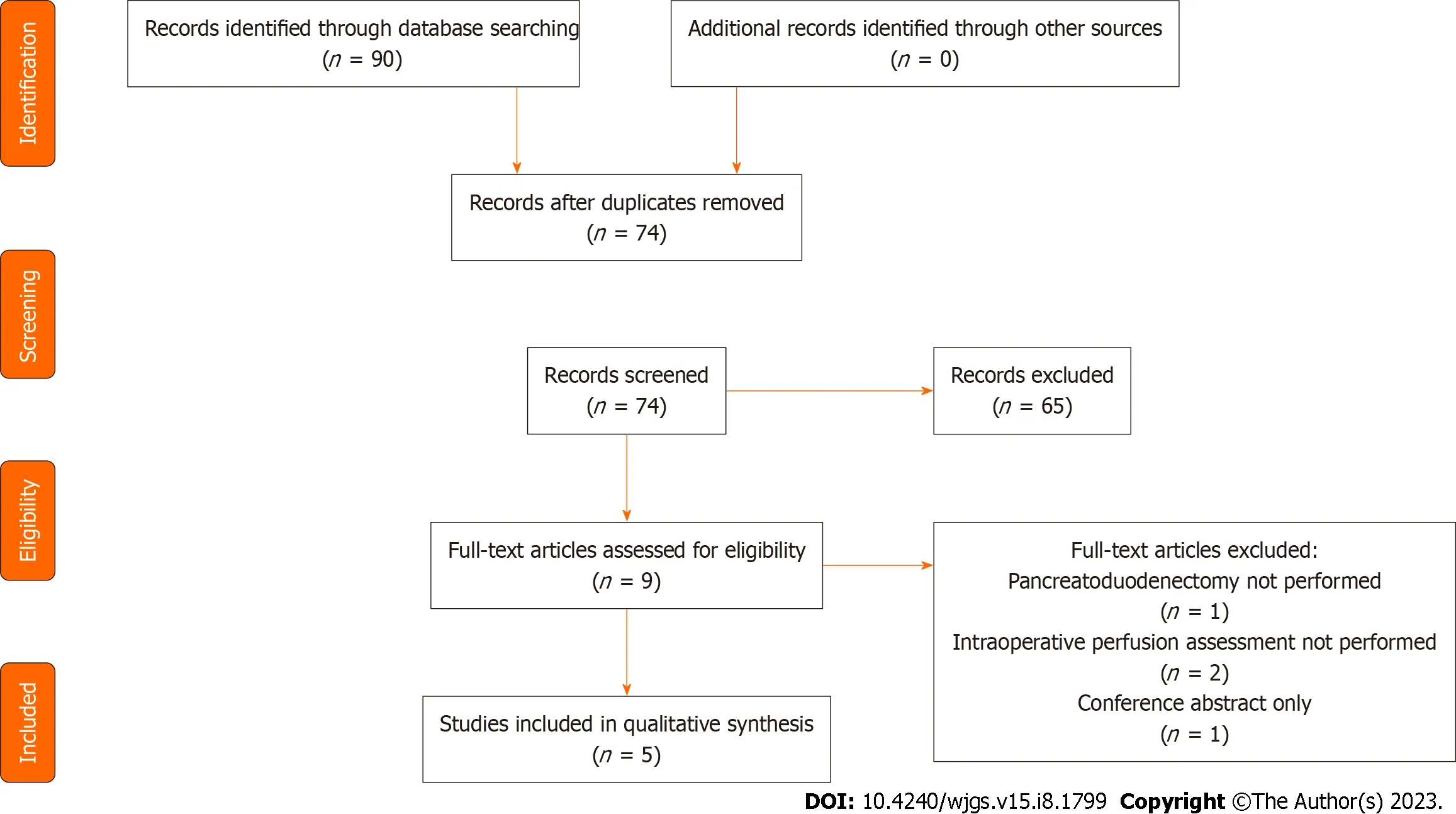
Figure 1 PRISMA diagram of included studies.
POPF
POPF occurred in 18 (12%) of patients (Table 3). No analysis of clinically relevant POPF has been performed as this was not defined in the study by Strasberget al[25] which contributes the majority of patients to the review. In the study by Doussotet al[27], 2 of the 3 (67%) clinically relevant POPF occurred in patients with documented hypoperfusion of the pancreatic stump. Rhoet al[23] identified hypoperfusion in their patient who developed a clinically relevant POPF. In the study by Strasberget al[25], all POPFs were identified in patients with hypoperfusion of the pancreatic stump, however,this should be interpreted with caution as all patients identified as having hypoperfusion underwent further resection of the pancreas prior to anastomosis. In the study by Iguchiet al[26], no hypoperfusion of the pancreatic stump was identified however they identified a leak from the distal end of the stump following distal pancreatectomy.
DGE
DGE was seen in 17 (11%) patients (Table 3). The incidence of DGE in patients with and without hypoperfusion of the pancreatic stump was not provided in either of the studies by Doussotet al[27] or Strasberget al[25]. The only patient in the case series by Rhoet al[23] experienced grade B DGE. They were found to have hypoperfusion of the pancreatic stump.
Post pancreatectomy haemorrhage
Post pancreatectomy haemorrhage (PPH) was seen in 2 (1%) patients (Table 3). The incidence of PPH in patients with and without hypoperfusion of the pancreatic stump was not provided.
90-d/inpatient mortality
Post-operative mortality was seen in 1 (0.6%) patient. It was not documented whether they had hypoperfusion of the pancreatic stump.
DISCUSSION
This scoping review mapped studies that assessed hypoperfusion of the pancreatic remnant during pancreaticoduodenectomy and its relationship with POPF. The five primary studies, including two prospective non-randomised studies and three case reports, identified utilisation of intraoperative assessment of perfusion using a range of techniques and variable resultant change in surgical management of the pancreatic remnant after confirmation of hypoperfusion. There was significant heterogeneity in the definition of POPF as the largest study in this series was published prior to the publication of the ISPGS definition. Our findings illustrate the safety and feasibility of intraoperative pancreas perfusionassessment and highlight its apparent limited usage since the first report twenty years ago. Variation in practice related to some patients having their pancreas remnant trimmed short if deemed to be hypoperfused whilst other patients were not.
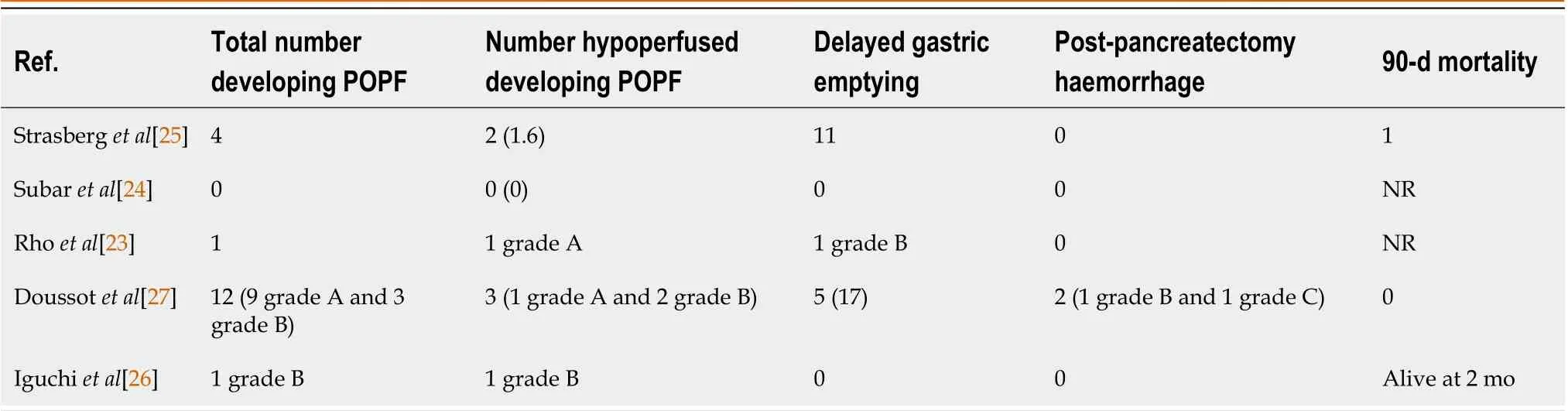
Table 3 Post-operative outcomes
The studies identified in this review have a combined POPF rate of 12%. This is lower than the published rate of 20%for clinically relevant POPF in recent randomised controlled trials comparing laparoscopic and open pancreaticoduodenectomies[28]. This is likely related to the Strasberget al[25] study which used a different definition for POPF as it was published pre ISPGS. Intraoperative pancreas perfusion assessment revealed that hypoperfusion was present in 39% of patients who developed POPF. The rate of POPF was 11% in patients with no evidence of hypoperfusion and 13% in those with evidence of hypoperfusion, suggesting that not all hypoperfusion gives rise to POPF and further analysis is required to analyse if there is a clinically relevant cut off. From this review, conclusive incidence of PPH and DGE in patients with hypoperfusion of pancreatic stump is not possible given the limited reporting of these complications. Noninvasive perfusion assessment modalities such as infra-red spectroscopy have been investigated in other surgical specialties and have been shown to accurately identify hypoperfusion, but their role in pancreatic surgery is yet to be investigated[29,30].
The link between hypoperfusion of the pancreatic stump and POPF remains inconclusive. In the large 123 patient study by Strasberget al[25] perfusion was assessed intraoperatively by subjective assessment of bleeding from the pancreatic stump with further resection in those deemed to be hypo-perfused. It demonstrated that 50% of clinically relevant POPFs occurred in patients with hypoperfusion that underwent further resection of the pancreas to well perfused tissue. This suggests that perfusion status of the stump intraoperatively,i.e.,local perfusion, may only be one component of the pathophysiology. Hyperlactataemia, a well-recognised hallmark of inadequate tissue perfusion and microcirculatory abnormalities[31], in the early post-operative period has been shown to be predictive of POPF.Hyperlactataemic patients (blood lactate ≥ 2.5 mmol/L) being 4.36 (1.70-11.15;P= 0.002) and 3.58 (1.22-10.48;P= 0.02)times as likely to develop POPF on uni- and multivariate analyses respectively[32].
Whilst several risk factors for POPF have been identified including consistency of the pancreatic parenchyma, size of the pancreatic duct and blood loss and have been combined to create the validated tool to predict POPF - the pancreatic fistula risk score[33], no study included this data and compared between the groups.
Post-operative acute pancreatitis (POAP) of the pancreatic remnant is an emerging entity in pancreas surgery[16], with inadequate tissue perfusion being key to its pathogenesis[34]. POAP exacerbates existing hypoperfusion, which may be why patients with higher vessel density (mm2) at histology show reduced POPF[35,36]. Intraoperative perfusion assessment may allow surgical optimisation of the pancreatic remnant, reducing the incidence and severity of POAP, in turn reducing POPF. Additionally, overall haemodynamic and perfusion status may contribute to local changes causing hypoperfusion, POAP and subsequent POPF, particularly in patients who are high-risk for POPF. Therefore, intraoperative perfusion assessment, coupled with goal directed therapy may improve pancreas perfusion and improve outcomes.
The use of ICG imaging for perfusion assessment is well established in gastrointestinal surgery, specifically in assessing tissues prior to anastomosis[37], yet it is not widely used in pancreas surgery. Four studies identified in this review demonstrated the feasibility of ICG usage to assess the pancreatic remnant, with an advantage over subjective visual assessment being clear identification and demarcation of hypoperfusion confirmed by a lack of fluorescence over affected areas. Moving forward, it is essential to determine the optimum dosage of ICG, timing of its measurement and distance the camera should be held from the anastomosis at time of imaging, to allow widespread reproducible use of this technique in pancreatic surgery. An objective scoring system would also need to be developed to allow reproducible results.
The findings of this review must be set in the context of its limitations. Firstly, data is only available from a small number of publications and it is plausible that the total number of patients who have had intraoperative perfusion assessment is much higher. Secondly, there is a likely publication bias, with only select centres who have experience with ICG and perfusion assessment publishing their results. Thirdly, there may be confirmation bias in those studies using subjective visualisation methods of perfusion assessment. Finally, current methods to assess perfusion of the stump only allow for assessment of the surface perfusion and not the deep tissues. However as robotic surgery develops further advances may allow for more detailed perfusion assessments using the firefly mode.
CONCLUSION
In conclusion, intraoperative perfusion assessment is technically feasible and appears safe. The quality of the current published literature is poor with the majority of publications included being either case reports or limited case series. The largest study was published prior to the publication of the ISPGS definition of POPF and clinically relevant POPF and their definition of POPF differed from the current accepted definition. There is insufficient evidence currently to evaluate whether poor perfusion of the pancreatic stump during pancreatico-duodenectomy is associated with an increased incidence of POPF. Moving forward further prospective studies are required to confirm the external validity of the studies identified in this review, ideally with creation of objective scoring systems allowing standardisation and improved analysis of data in future. Importantly, identifying the degree of hypoperfusion that is associated with, or predictive of, POPF and how this is best managed is a key priority.
ARTICLE HIGHLIGHTS
FOOTNOTES
Author contributions:Robertson FP, Spiers HVM, and Pandanaboyana S contributed to the manuscript preparation, study concept, and critical review; Loveday B and Roberts K were involved in the study concept and critical review.
Conflict-of-interest statement:All the authors report no relevant conflicts of interest for this article.
PRISMA 2009 Checklist statement:The authors have read the PRISMA 2009 Checklist, and the manuscript was prepared and revised according to the PRISMA 2009 Checklist.
Open-Access:This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers.It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: https://creativecommons.org/Licenses/by-nc/4.0/
Country/Territory of origin:United Kingdom
ORCID number:Francis P Robertson 0000-0001-5016-5944; Harry V M Spiers 0000-0001-7308-2711; Wei Boon Lim 0000-0002-7125-066X; Keith Roberts 0000-0003-1799-9829; Sanjay Pandanaboyana 0000-0003-3099-2197.
S-Editor:Wang JJ
L-Editor:A
P-Editor:Ju JL
 World Journal of Gastrointestinal Surgery2023年8期
World Journal of Gastrointestinal Surgery2023年8期
- World Journal of Gastrointestinal Surgery的其它文章
- Initial suction drainage decreases severe postoperative complications after pancreatic trauma: A cohort study
- Vascular complications of chronic pancreatitis and its management
- Historical changes in surgical strategy and complication management for hepatic cystic echinococcosis
- Post-transplant biliary complications using liver grafts from deceased donors older than 70 years:Retrospective case-control study
- Goldilocks principle of minimally invasive surgery for gastric subepithelial tumors
- Prognosis after splenectomy plus pericardial devascularization vs transjugular intrahepatic portosystemic shunt for esophagogastric variceal bleeding
