The effect of prophylactic antibiotics in acute upper gastrointestinal bleeding patients in the emergency department
Miao Gan, Liang Zong, Xuezhong Yu, Jun Xu
Emergency Department, State Key Laboratory of Complex Severe and Rare Diseases, Peking Union Medical College Hospital, Chinese Academy of Medical Science and Peking Union Medical College, Beijing 100730, China
KEYWORDS: Acute upper gastrointestinal bleeding; Prophylactic antibiotics; Stratification
INTRODUCTION
Acute upper gastrointestinal bleeding (AUGIB)refers to acute bleeding caused by diseases of the digestive tract above the flexor ligament, namely, the esophagus, stomach, duodenum, bile duct, and pancreatic duct.On the basis of the etiology, AUGIB can be divided into two types: varicose and nonvaricose.[1]AUGIB is one of the most common urgent and critical diseases worldwide, with an incidence rate of 47–150 cases per 100,000 person-years and a total mortality rate ranging from 3% to 15%.[2-6]Some studies have found that the mortality rate associated with gastrointestinal bleeding in patients with acute and chronic complications is as high as 35%.[4,7]
The current guidelines recommend prophylactic antibiotics for patients with liver cirrhosis accompanied by AUGIB.[8,9]Among cirrhosis patients during hospitalization for AUGIB, an increased risk of bacterial infection driven by portal hypertension and bacterial translocation has been reported.[10]
The study of the incidence of infection in noncirrhotic patients with AUGIB focuses mainly on elderly patients.Research has shown that AUGIB,especially severe bleeding, makes elderly people highly susceptible to infection.[11,12]However, for the entire group of AUGIB patients in the emergency department, the benefit of prophylactic antibiotics remains undetermined.We aimed to compare the clinical outcomes between AUGIB patients with and without prophylactic antibiotics to identify the population that requires this therapy in the emergency department.
METHODS
Study setting and study population
This was a retrospective study that enrolled patients with AUGIB admitted to the Emergency Department of Peking Union Medical College Hospital, Chinese Academy of Medical Sciences between 1stJanuary 2019 and 31stDecember 2021.
Inclusion criteria: 1) age > 18 years; 2) clinically diagnosed with AUGIB; and 3) admitted to our hospital’s Emergency Rescue Room.
Exclusion criteria: 1) AUGIB combined with lower gastrointestinal bleeding; 2) AUGIB caused by mechanical injury or other trauma; 3) participation in clinical trials of other drugs; 4) admitted owing to another disease, or AUGIB was not the major disease;and 5) AUGIB combined with other diseases requiring antibiotic therapy.
Antibiotic therapy
Current clinical guidelines recommend oral quinolones, fluoroquinolones, or intravenous thirdgeneration cephalosporins as standard prophylactic antibiotics.[13,14]Patients were divided into two groups,as follows: those who received any of the antibiotics mentioned above, as the antibiotic group, and those who did not receive any of the listed antibiotics, as the nonantibiotic group.
Outcomes
The primary outcome was the in-hospital death, and the secondary outcome was the onset of new infection.New infection was defined as no infection diagnosis at admission and infection diagnosis at discharge or inhospital death, using the diagnostic criteria for related infections (respiratory system, digestive system, urinary system, skin infection, or other systems).
Statistical analysis
SPSS 22.0 (IBM Corp., USA) was used for the analysis.Continuous data were expressed as the mean ± standard deviation or median (interquartile range), and two independent samplest-test or the nonparametric rank sum test was used for comparisons, as appropriate.Categorical data were expressed as number(proportions), Chi-square test or Fisher’s exact test was used for comparisons, as appropriate.Indicators with significant differences between the groups were included in the logistic regression analysis.AP-value <0.05 was considered statistically significant.
RESULTS
Characteristics of the enrolled patients
The current study included 392 individuals with AUGIB who were hospitalized in our hospital’s emergency department between 2019 and 2021; 281 patients received prophylactic antibiotics during hospitalization.Standard prophylactic antibiotics comprised intravenous third-generation cephalosporins,which were administered immediately upon admission and maintained until discharge.Demographic data for the antibiotic and non-antibiotic groups are shown in Table 1.The age distribution and sex were similar between the two groups.Patients in the antibiotic group had higher rates of bleeding history and higher C-reactive protein levels than those in the non-antibiotic group.This may be owing to the clinical physicians’ preferences for prophylactic antibiotics in patients with multiple bleeding episodes and high baseline C-reactive protein values.Other baseline characteristics were similar between the two groups.
Mortality
Heart failure was the main cause of death, and the deterioration of systemic chronic diseases, coagulation dysfunction, and severe infections led to multiple organ dysfunctions, which is the end-stage manifestation of critical illness.Acute blood loss itself is an important susceptibility factor for AUGIB and infection in the elderly, and infection is an important cause ofexacerbation and death.In this study, 17 (45.95%)patients died because of new infection.
The mortality rates were significantly lower in patients in the antibiotic group than those in the nonantibiotic group (6.41% vs.17.12%, χ2=10.68,P=0.001).As shown in Table 2, patients with advanced age,male sex, endotracheal intubation, no endoscopy, no prophylactic antibiotics, low platelet counts, high international normalized ratio, high AIMS65 score,concurrent infection, and myocardial injury had higher mortality rates.According to the multivariate logistics regression analysis, older age (odds ratio [OR]=1.049,95% confidence interval [CI]: 1.013–1.086;P=0.007),endotracheal intubation (OR=7.329, 95%CI: 2.859–18.786;P<0.001), no endoscopy performed (OR=3.507,95%CI: 1.427–8.620;P=0.006), variceal bleeding(OR=2.877, 95%CI: 1.043–7.933;P=0.041), and myocardial injury (OR=3.443, 95%CI: 1.313–9.028;P=0.012) were risk factors for mortality.
Risk factors for infection
Among 281 patients who received prophylactic antibiotics, 20 patients were infected during h o s p i t a l i z a t i o n; 111 c a s e s d i d n o t r e c e i v e prophylactic antibiotics, and 79 of these cases were infected during hospitalization.Prophylactic antibiotics reduced the incidence of infection compared with no prophylactic antibiotics (7.12% vs.71.17%, χ2=172.94,P<0.001).
In the patients with prophylactic antibiotics,univariate analysis showed that variceal bleeding(P<0.001), endotracheal intubation (P<0.001),endoscopy exam (P=0.002), endoscopy treatment(P=0.001), hepatic encephalopathy (P=0.001), and procalcitonin concentration (P=0.012) were the risk factors for infection.Multivariate logistic regression analysis revealed that the independent risk factors for infection were varicose veins (OR=3.684, 95%CI:1.030–13.179;P=0.045) and endotracheal intubation(OR=5.410, 95%CI: 1.688–17.364;P=0.005).
F o r t h e p a t i e n t s w i t h o u t p r o p h y l a c t i c antibiotics, variceal bleeding (P<0.001), tracheal intubation (P=0.001), hypertension (P=0.041), and cerebrovascular disease (P=0.018) were the risk factors for infection.Multivariate logistic regression analysis revealed that endoscopic treatment (OR=4.972, 95%CI: 1.459–16.943;P=0.010) was the independent risk factor for infection.
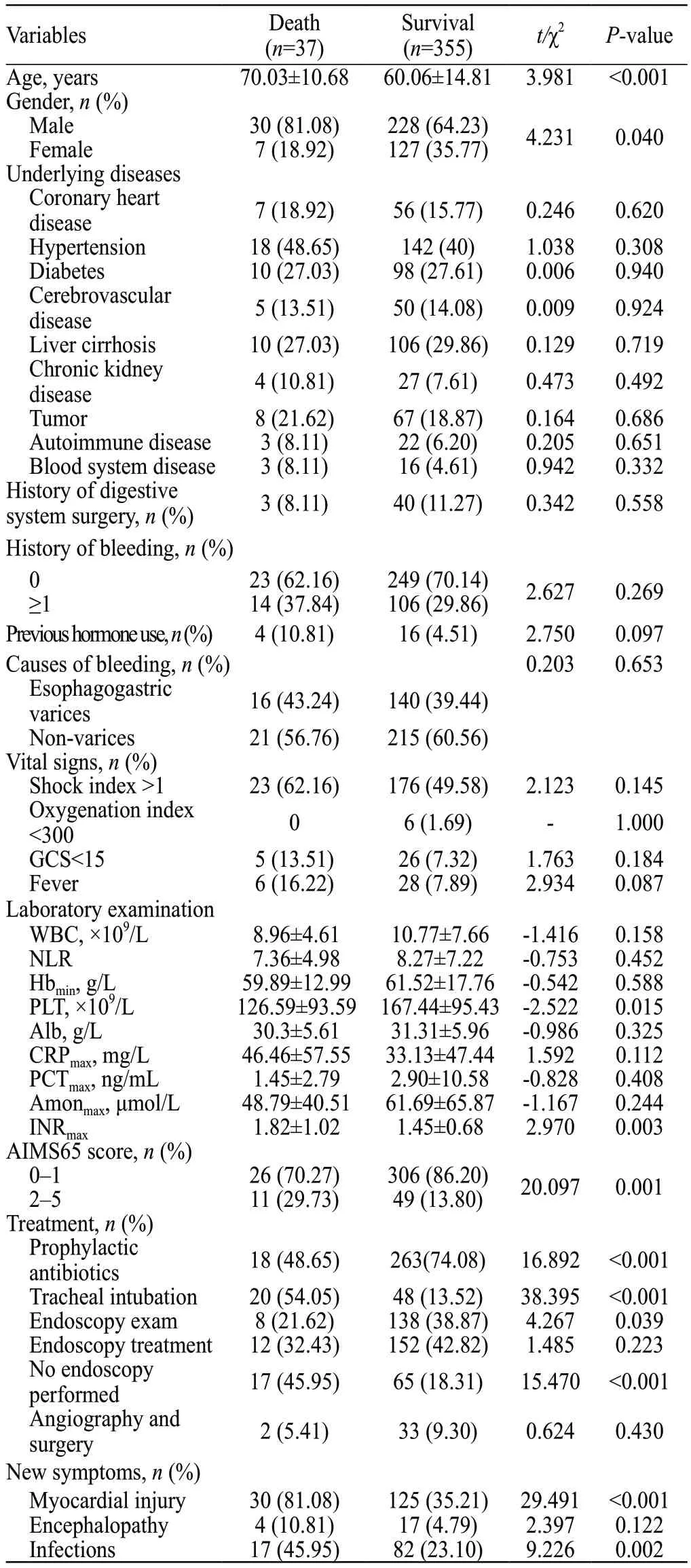
Table 2.Risk factors associated with mortality in AUGIB patients
Stratified analysis
A stratified analysis was performed and showed that patients aged ≥ 65 years, and those with endotracheal intubation, endoscopic treatment, and AUGIB with variceal etiologies benefited from prophylactic antibiotics (Table 3).
DISCUSSION
This study found that the mortality rates of AUGIB in our emergency department were significantly lower in antibiotic group than non-antibiotic group.Cirrhotic patients with AUGIB are susceptible to bacterial infection and its related rebleeding and increased mortality, which are driven by bacterial translocation and rebounding portal hypertension.Prophylactic antibiotics and endoscopic therapy are vital to stopping this vicious cycle.With recent advances in general management and endoscopic treatment of severely ill patients, the mortality rates due to uncontrolled bleeding from both gastroesophageal variceal bleeding and peptic ulcer bleeding have decreased markedly.[15-18]Age and comorbidities are significant contributors to patient mortality,[19]and prophylactic antibiotics are critical in addressing this concern.
Intestinal microorganisms are the largest and most complex microbial community in the human body.Studies have confirmed that intestinal microorganisms have an impact on nonalcoholic fatty liver disease, liver cirrhosis, liver failure, and hepatocellular carcinoma at different stages.[5,20-23]Currently, it is believed that with the development of liver cirrhosis to portal hypertension, a series of interactions occur between the intestinal flora and liver that are mutually causal.However, the relationship between changes in the intestinal microecology and the clinical outcomes of variceal upper gastrointestinal bleeding is still unclear.
Upper gastrointestinal bleeding and infection often coexist and impact each other.The reasons for upper gastrointestinal bleed complicated by infection include low immunity, imbalance of intestinal microbiota,invasive treatments, and hypoproteinemia.[24]In the current study, compared with patients who received prophylactic antibiotics, patients who did not receive prophylactic antibiotics had a higher infection rate(71.17%), which may be related to the severity of the disease, poor baseline condition, and high proportion of elderly patients in this study population.
In our cohort, the majority of the patients wereelderly and male.We found that advanced age and male sex were associated with elevated susceptibility to infection, and both were independent risk factors for death.Additionally, gastrointestinal bleeding is also more common in older patients and men in other countries.[20,21]Patients above the age of 65 have poor airway protection ability and many comorbidities,emphasizing the importance of prophylactic antibiotics to mitigate complications and death.
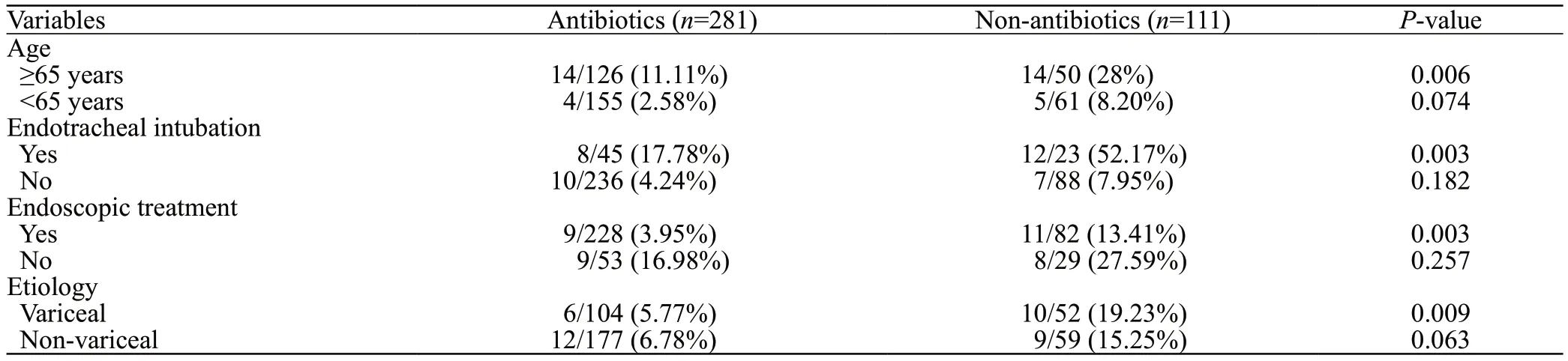
Table 3.Stratified analyses based on the age, endotracheal intubation, endoscopic treatment and etiology
A meta-analysis showed that pre-endoscopic intubation of patients with gastrointestinal bleeding was associated with a higher incidence of nosocomial pneumonia, longer hospital stay, and higher mortality compared with no intubation.[25]Endotracheal intubation is usually performed in emergency departments as an intervention for patients experiencing hematemesis and an inability to protect their airway.These patients have substantial gastrointestinal bleeding and large wounds that are prone to infection; therefore, prophylactic antibiotics are recommended.
Our study found that patients who could not undergo endoscopic examination owing to their physical condition had higher mortality; however,patients who received endoscopic treatment had higher infection rates.Patients usually undergo endoscopic therapy because of active or massive bleeding, which may lead to aspiration or mucosal damage during the operation.Additionally, the injection of sclerosing agent may prompt the onset of bacteremia.Therefore,prophylactic antibiotics in the emergency department are recommended for patients undergoing endoscopic therapy.
CONCLUSION
In conclusion, the administration of prophylactic antibiotics proved advantageous in reducing mortality among patients presenting with AUGIB at the emergency department.This was particularly noteworthy for patients aged 65 years and above,as well as those requiring endotracheal intubation,endoscopic intervention, and whose AUGIB was of variceal etiologies.Notably, the sample size in this study was small, and further prospective studies are needed to confirm our findings.
Funding:None.
Ethical approval:The study protocol was approved by the Ethics Committee of Peking Union Medical College Hospital, Chinese Academy of Medical Sciences (No.K1954).
Conflicts of interest:None.
Author contribution:MG: designed the experiments, conducted research, collected data, analyzed and interpreted data, drafted the article.LZ: criticized the knowledge content of the article.XZY:support work, including statistical analysis, obtaining research funding and guidance.JX: support work, including statistical analysis, obtaining research funding and guidance.
 World journal of emergency medicine2023年6期
World journal of emergency medicine2023年6期
- World journal of emergency medicine的其它文章
- Hemorrhagic pancreatitis from fenofibrate and metformin toxicity: a case report
- Omadacycline for the treatment of Legionella pneumophila pneumonia caused by drowning: a case report
- A case of pulmonary mucormycosis presented with cardiac arrest
- Pyopneumothorax caused by Parvimonas micra and Prevotella oralis: a case report
- Uterine artery pseudoaneurysm after subtotal hysterectomy: a case report
- The effects of hyperbaric oxygen therapy on paroxysmal sympathetic hyperactivity after cardiopulmonary resuscitation: a case series
