Ocular decompression retinopathy after phacoemulsification in a patient with primary acute angleclosure glaucoma undergoing chemotherapy
Yi-Lin Chen, Xiao-Nan Yang, Ying-Li Liu, Wen-Tao Li, Li-Jun Huo
Department of Ophthalmology, the First Affiliated Hospital,School of Medicine, Sun Yat-sen University, Guangzhou 510080, Guangdong Province, China
Dear Editor,
Ocular decompression retinopathy (ODR), which manifests as diffuse retinal hemorrhage occurring abruptly in multiple locations, including the subretinal,intraretinal, and preretinal spaces, is a rare complication after glaucoma surgery and is caused by sudden, iatrogenic lowering of intraocular pressure (IOP).Implicated procedures include glaucoma drainage implantation, trabeculectomy, iridotomy,and even cataract surgery[1].One report described a case of ocular decompression management following uncomplicated cataract surgery with no posterior capsular rupture or other intraoperative complications[2].Here, we report a rare case of
ODR triggered by phacoemulsification and the use of systemic
chemotherapeutic drugs in a patient with primary acute angleclosure glaucoma (PACG).The case not only improves our understanding of potential side effects of chemotherapeutic drugs on ophthalmic surgery but may also serve as a reference for clinicians in the management of patients with glaucoma with similar medical histories.Our study was approved by the Ethics Committee of the First Affiliated Hospital of Sun Yat-sen University in China (IIT-2022-041) and conducted in compliance with the guidelines of the Declaration of Helsinki.Written informed consent for publication was obtained from the patient.
CASE REPORT
First Ophthalmic AdmissionA 75-year-old woman who presented with persistent eye pain and blurred vision loss in the left eye for 1d came to the First Affiliated Hospital of Sun Yat-sen University on May 1, 2015.She was diagnosed with PACG and treated with tobramycin dexamethasone eye drops,brinzolamide eye drops, carteolol hydrochloride eye drops, and mannitol injection to reduce IOP and control inflammation.After 22d, because her visual acuity did not improve and IOP not well controlled, the patient was admitted to the ophthalmology department for further surgical treatment.Regarding past history, we learned that the patient had cervical cancer for which she had been treated with two courses of neoadjuvant intravenous chemotherapy using paclitaxel and cisplatin before this admission.In addition, she had been suffering from hypertension for over 20y, which was well controlled with amlodipine besylate (Figure 1).
At admission, the patient’s best-corrected visual acuity(BCVA) was 20/20 in the right eye and 20/40 in the left eye.The IOP was 13 mm Hg in the right eye and 33 mm Hg in the left eye.Upon slit-lamp examination, the left eye exhibited mild conjunctival congestion; a shallow anterior chamber with a small number of cells; a fixed, longitudinally elliptic,moderately dilated pupil; and grade 3 nuclear sclerosis (LOCS III)[3].Fundus examination revealed a cup-to-disk ratio of 0.4 with arteriolar narrowing.Besides, preoperative general examinations did not show any systemic contraindication for surgery.The patient’s coagulation parameters were normal,and her platelet counts were within normal range.
Phacoemulsification and intraocular lens implantation combined with goniosynechialysis was performed in the left eye under topical anesthesia on May 26, 2015.On postoperative day 1, the BCVA was 20/500 and the IOP was 17 mm Hg in the left eye.Fundus examination revealed a massive intraretinal hemorrhage in the posterior pole.Additionally, a massive preretinal hemorrhage was observed behind the internal limiting membrane of the retina.Optical coherence tomography (OCT) revealed dense hyperreflexia in front of the retina of the left eye (Figure 2A).

Figure 1 The course of PACG and cervical cancer, as well as the ophthalmological condition of the patient PACG: Primary acute angle-closure glaucoma; BCVA: Best-corrected visual acuity; OS: Lefteye.
For this patient’s fundus hemorrhage, we administered carbazochrome for hemostasis and methylprednisolone against inflammation within three days of surgery and instructed her to attend regular follow-ups.The BCVA of the patient remained 20/25 during a 5-month follow-up period.Moreover, the IOP was controlled at a normal level, fluctuating in the range of 14-19 mm Hg.Fundus examination and OCT revealed that the hemorrhage was absorbed gradually during the follow-up(Figure 2B-2E).
Second Ophthalmic AdmissionMore recently, presenting with visual loss in the right eye for 2mo, this patient was again admitted to our hospital for cataract surgery on November 22, 2021.Her last postoperative chemotherapy had been completed in September 2015.During the second treatment,the same surgical procedures and equipment were used as those for the first treatment.We observed no abnormal changes in the fundus examination or OCT after the second operation(Figure 2F-2G).
DISCUSSION
In this case, a complication in the form of fundus hemorrhage occurred 1d after phacoemulsification and intraocular lens implantation combined with goniosynechialysis in a 75-yearold patient with PACG.These procedures were conducted after she received a second cycle of neoadjuvant chemotherapy for cervical cancer.The hemorrhage might have been caused by a sudden lowering of IOP, which carries a high risk of ODR.However, the chemotherapeutic drugs might also have played a roleviaa toxic effect on the retinal vessels.
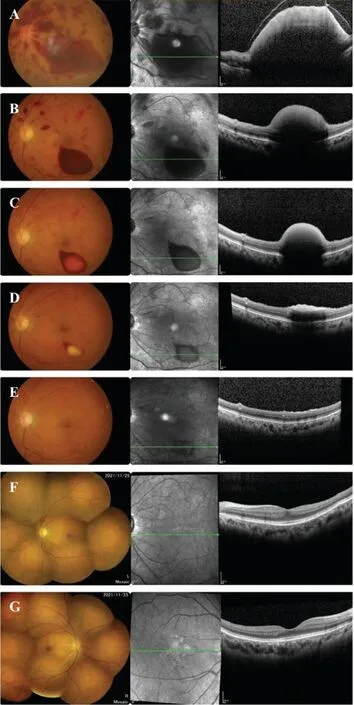
Figure 2 The optical coherence tomography (OCT) results at different stages after surgery A: Postoperative day 1; B:Postoperative month 1; C: Postoperative month 2; D: Postoperative month 3; E: Postoperative month 5; F: The second hospitalization in 2021, lefteye; G: The second hospitalization in 2021, right eye.
ODR manifests as diffuse retinal hemorrhages following an acute lowering of the IOP[1].Studies have revealed that the mean IOP decrease in ODR is 33.2±15.8 mm Hg (range,4-57 mm Hg), with 82% of ODR events occurring on the first postoperative day[4].In our case, the postoperative IOP was 16 mm Hg lower than the preoperative IOP.Unlike other surgeries or procedures commonly associated with ODR,such as trabeculectomy, glaucoma drainage implantation,and iridotomy, phacoemulsification, which was performed in this case, is rarely associated with ODR[1].In this patient,the hemorrhage occurred in the intraretinal and preretinal areas.Fundus examination did not reveal venous tortuosity or dilation consistent with central retinal vein occlusion.After excluding other possible causes of fundus hemorrhage, such as diabetic retinopathy, Terson syndrome, and other diseases caused by coagulation disorders, we considered ODR the most plausible diagnosis.Phacoemulsification combined with goniosynechialysis was an established management option for this patient who had PACG with senile cataract and uncontrolled IOP[5].However, during phacoemulsification,the IOP can fluctuate because of the relatively closed surgical environment.It was reported that the actual intraoperative IOP often exceeds 70 mm Hg and may sometimes drop precipitously to close to 0[6].The decreased IOP after surgery and the large intraoperative fluctuations in IOP may increase the blood perfusion of the retina and expand the retinal vessels[7-8], therefore, we suspected that the sudden lowering of IOP damaged the patient’s retinal capillaries.
Moreover, the patient had a history of neoadjuvant chemotherapy and had been administered paclitaxel and cisplatin, both commonly used for cervical cancer.Chemotherapy with paclitaxel can reportedly damage the integrity of the vascular endothelium and adversely affect endothelial function[9], as evidenced by a previous case report of bleeding gums caused by paclitaxel[10].Moreover, cisplatin can damage microvascular endothelial cells[11]and is associated with endothelial toxicity[9].As the preoperative examination did not reveal a systemic contraindication for surgery, we hypothesize that the fundus hemorrhage in our case might have been related to the toxicity of chemotherapeutic drugs to blood vessels.However, the specific mechanism of action of chemotherapeutic drugs on retinal hemorrhage is unknown, and further verification is required.
In addition, the patient had a history of hypertension for more than 20y, and prolonged, elevated blood pressure can lead to stenosis of the small vessel lumens and vessel wall degeneration[12-13].Combined with damage from chemotherapeutic drugs, we suspect that this factor led to the rupture of the small vessels and the occurrence of ODR.
The patient was followed up at our hospital for 6mo, revealing satisfactory outcomes.When the patient was readmitted for a second procedure in November 2021 for the right eye, it had been 5y since her last chemotherapy.Given the lack of hemorrhage in the right eye after cataract surgery, ODR and the toxicity of chemotherapeutic drugs to the retinal vessels were deemed a plausible explanation for the hemorrhages after the first surgery.
In summary, the iatrogenic lowering of IOP with the use of certain chemotherapeutic agents may cause ODR after cataract surgery for PACG, which can affect visual function.Therefore,physicians must be vigilant for postoperative ocular adverse events.Our results may help clinicians deal with potential complications in the treatment of patients with medical histories similar to the patient in our case.This study should alert them to the importance of perioperative IOP management during phacoemulsification.Slowly reducing IOP to normal levels before surgery might be helpful.
ACKNOWLEDGEMENTS
Authors’ contributions:Huo LJ diagnosed and treated this case; Chen YL wrote the manuscript; Chen YL, Liu YL, and Li WT collected data; Huo LJ and Yang XN reviewed the manuscript.All authors have read and approved the final version of the manuscript.
Conflicts of Interest: Chen YL,None;Yang XN,None;Liu YL,None;Li WT,None;Huo LJ,None.
 International Journal of Ophthalmology2024年2期
International Journal of Ophthalmology2024年2期
- International Journal of Ophthalmology的其它文章
- Using choroidal thickness to detect myopic macular degeneration
- lmpact of multifocal gas-permeable lens designs on short-term choroidal response, axial length, and retinal defocus profile
- Baerveldt glaucoma implant with Supramid© ripcord stent in neovascular glaucoma: a case series
- Efficacy and safety of Usights UC100 illuminated microcatheter in microcatheter-assisted trabeculotomy
- Quantifying peripapillary vessel density and retinal nerve fibre layer in type 1 diabetic children without clinically detectable retinopathy using OCTA
- Nomogram to predict severe retinopathy of prematurity in Southeast China
