妊娠期血浆CRH、E2及 P与早产关系的研究
罗穗豫 王瑜
妊娠期血浆CRH、E2及 P与早产关系的研究
罗穗豫 王瑜
目的 探讨促肾上腺激素释放激素(corticotropin releasing hormone, CRH)、雌二醇(estradiol, E2)及孕激素(progesterone, P)在妊娠期间的浓度变化及其在早产中的预测作用。方法 选取正常妊娠组孕妇54例, 先兆早产组孕妇54例, 采集外周静脉血分离血浆, 用免疫化学发光法测定E2、P, 放射免疫法测定CRH水平。结果 ①正常妊娠血CRH均值28~33周组与>37周组比, 明显低于>37周组, 经t检验P<0.05;血E2各组间均值经t检验P>0.05, 差异无统计学意义;血P各组均值, 28~33周组明显高于>37周组, 经t检验P<0.05, 差异有统计学意义, 其余各组差异无统计学意义。②正常妊娠组和先兆早产组在妊娠28~33周血CRH分别为 (68.23±13.34)ng/L和(298.42±162.78 )ng/L;在34~36周分别为 (132.75±126.3) ng/L和(354.42±50.46) ng/L, 经t检验, P值均<0.05, 差异有统计学意义。正常妊娠组和先兆早产组血E2在28~33周分别为(128.72±50.83)μg /L和(152.94±31.7)μg/L;在34~36周分别为(136.24±62.41)μg /L和(173.58±92.3)μg/L, 两组均值经t检验, P值均<0.05, 差异无统计学意义。正常妊娠组和先兆早产组血P在28~33周分别为(523.52±105.43)μg/L和(353.21±52.21)μg/L, 34~36周(483.24±113.52)μg/L和(310.25±83.02)μg/L, 差异有统计学意义。结论 血P在妊娠晚期各孕周组间变化较为明显, 妊娠>37周之后明显下降。妊娠晚期正常妊娠组中的血浆CRH值随着孕周增加而逐渐升高,而血E2值无明显变化。
促肾上腺皮质激素释放激素;雌二醇;孕酮;早产
早产占整个妊娠的7% ~10%, 早产儿死亡率为15%, 是围生期新生儿死亡的首要原因。探讨促肾上腺激素释放激素(corticotropin releasing hormone, CRH)、雌二醇(estradiol, E2)及孕激素(progesterone, P)在妊娠期间的浓度变化及其在早产中的预测作用。
1 资料与方法
1.1 一般资料 研究对象选自2012年1月~2012年12月,在河南省人民医院进行产前检查的108例孕妇。排除心脏病、高血压、糖尿病等妊娠合并症及并发症。
1.1.1 实验分组 正常妊娠组54例:根据孕周分为28~33周、34~36周组、大于37周组, 每组各18例, 平均年龄28.2岁。先兆早产组54例:根据孕周分为小于33周组和34~36周组,每组各27例, 平均年龄28.5岁。
1.1.2 诊断标准 早产、先兆早产的诊断标准参照乐杰主编的《妇产科学》[1]。
1.2 实验方法 收集孕妇肘静脉血2 ml, 正常妊娠组于上午10时在门诊采血, 先兆早产组于入院时采血, 采血后, EDTA抗凝, 3500 r/min离心10 min, 分离血浆, -20℃保存备用。
主要试剂:CRH放射免疫分析试剂盒(上海锐聪科技公司)。E2免疫化学发光试剂盒, P免疫化学发光试剂盒( 上海江莱生物科技有限公司)。
1.3 统计学方法 用SPSS19.0统计软件处理。所得数据均数用( x-±s)示。均数比较采用独立样本t检验。P<0.05为差异有统计学意义。
2 结果
2.1 正常妊娠组血CRH、E2、P变化
2.1.1 CRH 妊娠28~33周孕妇血CRH(68.23±13.34)ng/L, 34~36周(132.75±126.30) ng/L, >37周(352.12±166.05) ng/L。妊娠晚期正常妊娠组血CRH浓度随着孕周增加而逐渐升高。妊娠28~33周组与34~36周组血CRH均值比较P=0.0383,差异有统计学意义;28~33周组与>37周组均值经t检验P= 0.0001, 差异有统计学意义。
2.1.2 E2、P: 妊娠28~33周正常孕妇血E2(128.72±50.83)μg /L, 34~36周 (136.24±62.41) ug /L, >37周(125.37±52.25)μg /L。各孕周组间血E2均值经t检验, P>0.05, 各组间差异无统计学意义。妊娠28~33周正常孕妇血P (523.52±105.43)μg /L, 34~36周(483.24±113.52)μg /L, >37周(423.23±121.62)μg /L。血P在28~33周为(523.52±105.43) μg /L, 34~36周(483.24±113.52)μg /L, >37周(423.23±121.62)μg /L, 均值经t检验, 28~33周组与>37周组P=0.0123, 差异有统计学意义, 其余各组差异无统计学意义。见表1。
2.2 先兆早产组血CRH、E2、P变化 妊娠晚期先兆早产组血CRH、E2浓度随妊娠周数缓慢升高, 血P>37周显著下降。28~33周血CRH (298.42±162.78) ng/L, 34~36周血CRH (354.42±50.46)ng/L, P>0.05, 两组差异无统计学意义。28~33周血E2(152.94±31.7) μg /L, 34~36周血E2(173.58±92.3) μg /L, P>0.05, 两组差异无统计学意义。28~33周组血P (353.21±52.21) μg/L, 34~36周血P (310.25±83.02)μg/L, P<0.05, 两组差异有统计学意义。见表2。
2.3 正常妊娠组与先兆早产组血CRH、E2、P的比较 正常妊娠组与先兆早产组在28~33周、34~36周血CRH均值经t检验, P<0.05, 差异有统计学意义。见表3。
在28~33周和34-36周两组血E2均值经t检验, P值分别为0.0551、0.1409差异无统计学意义。见表4。
在28~33周和34~36周, 两组血P均值经t检验, P值均<0.05, 差异有统计学意义。见表5。

表1 正常妊娠组不同孕期血CRH、E2和P的均值(x-±s)

表2 先兆早产组血CRH和E2、P的变化(x-±s)
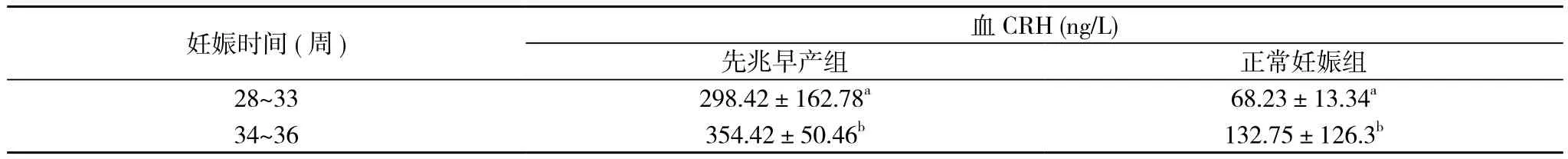
表3 正常妊娠组与先兆早产组血CRH的比较(-x±s)

表4 正常妊娠组与先兆早产组血E2的比较( x-±s)

表5 正常妊娠组与先兆早产组血P的比较( x-±s)
3 讨论
3.1 CRH、E2和P在妊娠过程的作用 促肾上腺激素释放激素(CRH)是一种41个氨基酸的下丘脑多肽, 近年来发现胎盘CRH的分泌量远远超过下丘脑的分泌量, 成为妊娠期母体外周血CRH的主要来源[2]。
胎盘CRH作用在胎儿垂体-肾上腺轴, 刺激肾上腺产生雄激素、皮质醇并且同时直接通过受体作用在子宫平滑肌细胞上。CRH在孕16~20周开始升高, 它像定时器一样控制着妊娠的时限, 调控着胎盘的功能, 而且, 分娩并不是分娩的那一刻的结果, 而是在孕早期就注定的一个过程[3]。本文正常分娩组血CRH随妊娠周数增加逐渐上升, 与报道一致。
妊娠期血浆中CRH水平呈指数性升高, 然而, 相比足月分娩的妇女, 在先兆早产的妇女中升高的幅度大, 过期分娩的妇女中幅度小。本研究中先兆早产组CRH在各孕周组的浓度都显著高于正常妊娠组, 可以认为CRH可能在早产的发病中起重要作用, CRH的异常升高可能决定了分娩时间的提前。因此, 在临床上监测孕妇CRH的变化有望成为预测早产的可靠指标。
本研究中血E2在正常妊娠组与早产组各妊娠阶段值波动不大, 而血P变化明显, 与谭春英[4]的研究结果一致, 认为E2、P在正常妊娠的发动中是以P为主, 在分娩晚期质量浓度明显下降,不能维持子宫的相对静止状态,使得子宫平滑肌敏感性加强,最终导致分娩发动。P还作为免疫调节剂控制着许多孕期的免疫反应, 它的撤退会抑制免疫反应。有效的孕激素撤退发生在分娩的开始, 机体通过孕激素的分解代谢、受体结合和抵抗孕激素的分子结构变化等方法使游离孕激素浓度减少[5]。子宫平滑肌也由静息状态向敏感状态转化。本文血P在33周后逐渐下降, 与报道一致。
3.2 CRH、E2和P的相互作用 在分娩时胎盘 CRH在血浆中呈指数升高, 刺激胎盘产生雌激素, 抑制胎盘合成孕激素。胎盘CRH也释放到胎儿循环, 刺激胎儿肾上腺产生脱氢表雄酮。脱氢表雄酮是胎盘雌激素合成的前体[6]。孕激素对于妊娠的维持是非常重要的, 产生于肾上腺、黄体、脑和胎盘,在怀孕期间使子宫处于静止期, 它的撤退会导致分娩期子宫平滑肌的收缩[7]。孕激素对胎盘CRH的分泌有抑制作用,其通过与滋养细胞内糖皮质激素受体结合而发挥作用[8]。临床试验显示预防性使用孕激素可以减少早产的发生[9]。然而, 因CRH像定时器一样控制着妊娠的时限, 所以孕激素治疗不会减少自发性早产的发生[10], 而CRH拮抗剂可以通过PKC-依赖途径介导使孕激素升高, 减低早产的风险[11], 联合治疗比单药治疗也许能更好的改善早产[12]。
将来, 以P 、CRH以及炎性免疫应答为基础的临床应用可能会对预防早产有益, 这是目前导致新生儿致病和致死的重要原因。
[1] 乐杰.妇产科学.第7版.北京:人民卫生出版社, 2008:113.
[2] Ruth V, Hallman M, Laatikai nen T, et al.Corticotropin-releasing hormone and cortisol in cord plasma in relation t gestational age, labor and fetal distress.Am J Perinae-co, 1993, 10(2): 115-118.
[3] McLean M, Bisits A, Davies J, et al.A placental clock controlling the length of human pregnancy.Nature medicine, 1995, 1(5): 460-463.
[4] 谭春英,蔺莉.E2、P、CRH在早产发病中的作用.首都医科大学学报, 2005,26(5):620-623.
[5] Vrachnis N, Malamas F M, Sifakis S, et al.Immune aspects and myometrial actions of progesterone and CRH in labor.Clinical and Developmental Immunology, 2011:2012.
[6] YouX, Yang R, Tang X, et al.Corticotropin-releasing hormone stimulates estrogen biosynthesis in cultured human placental trophoblasts.Biol Reprod, 2006,74(6):1067-1072.
[7] E.Karteris, D.Markovic, J.Chen, et al.Identification of a novel corticotropin-releasing hormone type 1β-like receptor variant lacking exon 13 i n human pre gnant myometrium regulated by estradiol-17β and progesterone.Endocrinology, 2010, 151(10): 4959- 4968.
[8] Karalis K, Majzoub JA.Regulation of placental corticotrophin releasing hormone by s teroids: possible implication in labour initiation.Ann NY Acad Sci ,1995,771(1):551-555.
[9] Mackenzie R, Walker M, Armson A, et al.Progesterone for the prevention of preterm birth among women at increased risk: A systematic review and meta-analysis of randomized controlled trials.Am J Obstet Gynecol, 2006,194(5):1234-1242.
[10] Da Fonseca EB, Bittar RE, Carvalho MH, et al.Prophylactic administration of progesterone by vaginal suppository to reduce the incidence of spontaneous preterm birth in women at increased risk: A randomized placebo-controlled double-blind study.Am J Obstet Gynecol , 2003,188(2):419-424.
[11] Keller PA, Kirkwood K, Morgan J, et al.The prevention of preterm labour-corticotrophin releasing hormone type 1 receptors as a target for drug design and development.Mini reviews in Medicinal Chemistry, 2003,3(4):295-303.
[12] Foteini Stamatelou, Efthimios Deligeoroglou,Georgios Farmakides, et al.Abnormal progesterone and corticotropin releas ing hormone levels are associated with preterm labour.Annals of the Academy of Medicine, 2009, 38(11):1011.
Study on the relationships between the plasma CRH, E2and P during pregnancy and premature delivery
LUO Sui-yu, WANG Yu.Department of obstetrics and Gynetology,People’s Hospital of Zhengzhou University (Henan People’s Hospital), Zhengzhou 450003, China
Objective To discuss the concentration changes of Corticotropin Releas ing Hormone(CRH), Estradiol (E2), and Progesterone (P) during the third trimester and analyze its predictive role in preterm.Methods 54 pregnant women of threatened prematurity were enrolled as the threatened prematurity group, 54 normal pregnant women were selected as normal pregnant group.Three milliliters of venous blood were taken from all of the women.The levels of E2, P were detected by chemiluminescence immunoassay (CLIA), CRH by radioimmunoassay (RIA).Results The mean plasma CRH of 28~33 weeks group was significantly lower than > 37 weeks group in the normal pregnant group (P<0.05).There was no significant deference in each groups about the E2(P>0.05). The mean plasma P of 28~33 weeks group was significantly higher than > 37 weeks group (P<0.05).In 28~33 weeks the plasma CRH were respectively (68.23±13.34)ng/L and (298.42±162.78 ) ng/ L in the group of normal pregnant and the group of threatened prematurity.The same as (132.75±126.3) ng/ L and (354.42±50.46) ng/L in 34~36 weeks.There was a significant difference in the plas ma CRH in the two groups (P<0.05).In 28~33 weeks the plasma CRH were res pectively (68.23±13.34)ng/L and (298.42±162.78 ) ngl/L in the group of normal pregnant and the group of threatened prematurity.The same as (132.75±126.3) ng/L and (354.42±50.46) ng/L in 34-36 weeks.There was a significant difference in the plasma CRH in the two groups (P<0.05).In 28~33 weeks the plasma E2were respectively (128.72±50.83)μg/L and (152.94±31.7) μg/L in the group of normal pregnant and the group of threatened prematurity.The same as (136.24±62.41)μg/L and (173.58±92.3)μg/L in 34~36 weeks.There was no significant difference in the plasma E2in the two groups(P>0.05).In 28-33 weeks the plasma P were respectively (523.52±105.43)μg/L and (353.21±52.21)μg/L in the group of norm al pregnant and the group of threatened prem aturity.The same as (483.24±113.52)μg/L and (310.25±83.02)μg/L in 34~36 weeks.There was a significant difference in the plasma E2in the two groups (P<0.05).Conclusion The plasma P changed obviously in the third trimester.It was declined significantly after the 37th weeks.In the trimester the plasma CRH gradually increased with the increasing gestational age.But there was no significant changes in E2. CRH may be an important factor in onset of delivery.
Corticotropin releasing hormone (CRH);Estradiol (E2);Progesterone (P);Premature delivery
450003 郑州大学人民医院暨河南省人民医院妇产科
王瑜