Assessment on self-care, mobility and social function of children with spina bi fi da in Turkey
Hulya Sirzai, Beril Dogu, Selamet Demir, Figen Yilmaz, Banu Kuran
1 Ankara Physical Medicine and Rehabilitation Education and Research Hospital, Ankara, Turkey
2 Department of Physical Medicine and Rehabilitation, Sisli Etfal Education and Research Hospital, Istanbul, Turkey
Assessment on self-care, mobility and social function of children with spina bi fi da in Turkey
Hulya Sirzai1, Beril Dogu2, Selamet Demir2, Figen Yilmaz2, Banu Kuran2
1 Ankara Physical Medicine and Rehabilitation Education and Research Hospital, Ankara, Turkey
2 Department of Physical Medicine and Rehabilitation, Sisli Etfal Education and Research Hospital, Istanbul, Turkey
The aim of the study was to investigate the functional performance in children with spina bi fi da, using the Pediatric Evaluation of Disability Inventory (PEDI) to look into capacity of twenty-eight children with spina bi fi da with lesions at different levels in different dimensions of selfcare, mobility and social function. Mean age of the patients was 3.5 ± 2.3 (1-10) years. In the muscle test carried out, 13 patients (44.8%) had no movements including pelvic elevation in lower extremity muscles and they were at level 5. Sixteen patients (54%) were non-ambulatory according to the Hoofer ambulation classi fi cation. Raw and scale scores in the self-care, mobility and social function domains both in the functional skill scale and in the caregiver scale were found to be lower compared to the data of the normal population. A statistically significant correlation was observed in the self-care values of the Functional Skills Scales and the Caregiver Assistance Scale measurements, which was positive for age and negative for Functional Ambulation Scale and muscle test (P < 0.05). A positive relation was found between the Functional Skills Scales-mobility area and age while a negative relation was observed between Functional Ambulation Scale and muscle test (P < 0.005). A negative relation was also found between Caregiver Assistance Scale-mobility and Functional Ambulation Scale and muscle test (P < 0.005). In our study, the functional performance of the children was found to be low. Low-level lesions, encouraging muscular strength and independence in mobility are all very important factors for functional independence.
nerve regeneration; spina bifida; myelomeningocele; disability evalutatıon; self-care; mobility; muscular energy; child; social function; neural regeneration
Sirzai H, Dogu B, Demir S, Yilmaz F, Kuran B. Assessment on self-care, mobility and social function of children with spina bifida in Turkey. Neural Regen Res. 2014;9(12):1234-1240.
Introduction
Spina bi fi da (SB) is a complex congenital central nervous system disease that is caused by the incomplete closing of the neural tubes between the 22ndand 28thweeks of gestation (Tarazi et al., 2008). The worldwide incidence rate of the disease is 1 in every 1,000 live births (Alfarra et al., 2011). In Turkey, this rate is about 3% (Ulus et al., 2012). Many children born with this disease died before the development of shunt operations in 1960’s. In today’s advanced medical world, 75-80% of children born with SB were expected to survive until adulthood (Dicianno et al., 2008). Another longitudinal cohort study done on 117 SB cases reported the life expectancy as 40 years (Davis et al., 2005). In contrast with these advancements in lifespan, many patients have varying degrees of spasticity, urinary and fecal incontinence and neurocognitive retardation. Such problems decrease the patients’ functional independence and their quality of life. In these children, there is a decrease in cognitive functions and fi ne motor skills as well as retardation in movement quality (Vinck et al., 2010).
There are many studies that review the functional independence in the daily lives of both children and adults with SB. Buran et al. (2004) reviewed 66 adolescent SB patients’ functional independence using Functional Independence Measure for Children (WeeFIM). They found out that the most dependent areas for these adolescents were bladder and bowel management, toilet transfer and stair mobility. Andren and Grimby (2000) measured this functional independence in 20 adult SB patients using FIM. They reported that patients were completely independent in eating, social and cognitive areas meanwhile they are partially dependent on the others. Müller-Godeffroy et al. (2008) performed a study on children and adolescents with myelomengocele using KINDL-R and found out that there is a decrease in all aspects in patient’s quality of life when compared with the other people in their age group. This decrease was signi fi cant in self-esteem and emotional well-being areas. The relationship between high lesion levels and decreased functional independence was reported in many studies (Padua et al., 2002; Schoenmakers et al., 2003; Verhoef et al., 2006).
The aim of the study is to investigate the functional performance in children with SB, using the Pediatric Evaluation of Disability Inventory (PEDI) to look into their capacity in different dimensions of self-care, mobility and social function.
Participants and Methods
Participants
Twenty-eight children with different types of SB, aged 6 months-10 years, lived in Turkey and were included in this study. Non-Turkish speaking patients or families were excluded. All these participants applied to our clinic were patients. After talking with their patients, written informed consent regarding involvement of these patients and subsequent examination was obtained before starting. Data on age, sex, mode of delivery, lesion and neurological level, existence of spasticity, joint contractures, presence of hip dislocation, spinal deformity, mental status, functional capacity of the bladder and intestinal system, ambulation level and muscular strength were collected and recorded during clinical examination. The neurological level of each subject was determined by one of the authors in a clinical neurological examination. Clinical assessments were done by trained and certi fi ed rehabilitation physicians with at least 1 year of experience in examination of patients with spinal cord injury. Neurological levels were de fi ned as “high” in mid-lumbar and thoracic level lesions and “low” in sacral and lumbosacral lesions (Bartonek et al., 1999).
The children were divided into fi ve classes of muscle function according to their lower limb muscle strengths. The classes had the following properties: (1) Weakness of intrinsic foot muscles; good to normal foot plantar fl exion (grade 4-5); (2) fair or less foot plantar fl exion (grade 3 or less); fair or better knee fl exion (grade 3 or more); poor to fair or better hip extension and/or hip abduction (grade 2-3 or more); (3) good to normal hip fl exion and knee extension (grade 4-5); fair or less knee fl exion (grade 3 or less); trace of hip extension, hip abduction and below-knee muscles; (4) no knee extension activity; poor or less hip fl exion (grade 2 or less); fair or good pelvic elevation; (5) no muscle activity in the lower limbs; no pelvic elevation (Danielsson et al., 2008).
Presence of spasticity in ankle, knee, and hip joint was documented. Presence of spasticity was assumed based on the presence of symptoms including clonus, claps-knife response, resistance throughout passive range of motion, and static abnormal posturing with increased muscle tension despite full passive motion. Modi fi ed Aswhort Scale (MAS) was used to evaluate spasticity. According to MAS staging, the classi fi cation is as follows: 0, no increase in the muscular tonus; 1, feeling of minimal resistance at the end of the range of motion (ROM) when the affected parts are moved in fl exion and extension or presence of catch-and-release feeling; 1+, feeling of traction during the movement, resistance felt within less than half of the ROM; 2, resistance is felt within most of the ROM, but it is easy to move the affected part; 3, passive movement is difficult throughout the ROM; 4, the affected part is rigid in fl exion or extension (Bohannon and Smith, 1987).
ROM in lower extremity was measured in a standardized way with a two-legged 360-degree goniometer and compared with reference values for children. Thomas test was used to measure hip flexion. Test was conducted by measuring the fl exion ROM while the patient lay in the supine position and the other leg was fully extended. Lumbar area was stabilized with a hand to compensate lumbar lordosis. In order to differentiate gracilis contracture from other adductor muscle contractures, hip abduction was measured while both knees were in 90 degrees and hip in 90 degrees fl exion and also while the both legs are in full extension. Knee joint contracture is identified if knee extension is limited with the hip in extension (to relax the hamstrings) and the ankle relaxed in a position of equinus (to relax the gastrocnemius). Popliteal angle was measured for hamstring tension in the knee. Duncan-Ely test was performed to determine rectus femoris spasticity. To measure ankle dorsiflexion and differentiate gastrocnemius and soleus spasticity, ROM was measured while the knee and hip were in 90 degrees fl exion and in total extension.
Joint contractures of the lower limbs were de fi ned for the ankle if ≥ 15 degrees of fi xed equinus foot, for knee if ≥ 20 degrees of extension contracture or for hip if ≥ 20 degrees of extension contracture were observed (Danielsson et al., 2008). All contractures were measured in the supine position. We used the Hoofer classi fi cation to describe ambulation (Hoofer et al., 1973). (1) Normal ambulators: Patients without any mobility problems, not using any devices for mobility at all. (2) Community ambulators: Patients who walk indoors and outdoors for most of their activities may need crutches, braces or both. They use a wheelchair only for long trips out of community. (3) Household ambulators: Patients who walk only indoors and with apparatus. They may use Wheelchair for some indoor activities at home and school and for all activities in community. (4) Non-functional ambulators: Patients, who are able to walk in a therapy session, but use their wheelchair afterwards. (5) Non-ambulators: Patients who are wheelchair bound.
Scoliosis was reviewed in physical examination. The patient was checked for asymmetry in the spine, shoulders, trunk and pelvis. Paravertebral or rib elevations were noted. If the patient was positive in these areas, we diagnosed scoliosis in those patients. Patients were also asked to bring their previous scoliosis X-rays if they had one. Scoliosis presence was enough for our study, so we did not research the degree of scoliosis in our patients. Hip dysplasia was diagnosed based on clinical examination and patient history. Mental retardation was reviewed through patient history and patient fi le.
Information on bladder and bowel management was obtained by the patient history review. Incontinence was defi ned as “loss of control that results in spoilage with urine or feces that requires a change of diaper or clothes at least once a month (with or without the use of condom-type, urethral or suprapubic catheters)”.
Instrument
PEDI is a scale that determines the level of independency in daily living activities. It was developed by Haley and his colleagues to evaluate functional statuses of children between 6.5 months and 7 years of age with congenital or acquired disabilities (Haley et al., 1999). PEDI consists of three scales: Functional Skills, Caregiver Assistance, and Modifications. The Functional Skills Scales (FS) were designed to samplemeaningful sub-tasks of a set of complex functional activities. The Caregiver Assistance Scale (CA) is a measure of the extent of help the caregiver provides in typically daily situations. The Modi fi cations Scale is a measure of environmental modifications and equipment used by the child in routine daily activities. Each individual scale is designed to capture a different aspect of the child’s function in self-care (SC), mobility (MO) and social function (SF) domains. PEDI consists of 197 functional skill items, and 20 items of them assess caregiver assistance and modifications (Haley et al., 1999). We used only the functional skill scale and the caregiver scale. Its validity, reliability and adaptation to various societies have been shown through several studies (Nordmark et al., 1999; Feldman et al., 2001; Gannotti et al., 2001; Wassenberg-Severijnen et al., 2003; Srsen et al., 2005). Its adaptation to, and validity and reliability for the Turkish society have been shown by Erkin et al. (2007). It was used to determine the functional statuses of children with disabilities including cerebral palsy and SB (Tsai et al., 2002; Ostensjo et al., 2003; Kothari et al., 2003; Sirzai et al., 2008). It was used to determine the functional status of children with disabilities such as cerebral palsy and SB. PEDI is a useful test to classify motor functions (Bartonek et al., 2001). We de fi ned patients with normal functional skills and caregiver assistance scores as being functional independent. Internal consistency, overall reliability and test-retest reliability of the Turkish translation of the PEDI were all encouraging. ICC of 0.99 for FS-SC, FS-MO and FS-SF. Values of ICC were found as 0.98 for CA-SC subscale, 0.97 for CA-MO and 0.96 for CA-SF subscales.
PEDI was administered to the parents of all children in this study interview form as a parent-report questionnaire. Interviews were scheduled to take 40-50 minutes and were conducted by one of the investigators. In the present study, the PEDI software program was used for data storage and for the generation of individual score pro fi les. Six subscale raw scores were obtained as follows: FS-SC, FS-MO, FS-SF, CASC, CA-MO and CA-SF. The raw scores and scale score of these six subscales were used in the statistical analyses. Only raw and scale scores were used since there are no studies on validity and reliability of normative values.
The study was approved by the Ethical Committee Sisli Etfal Training and Research Hospital with registration No. 132.
Statistical methods
The number of patients to be included in the present study was determined by a statistical analysis in order to enable the examination of the statistical relations with a significance level of 95%. Using the NCSS software, the number of individuals to be included in the study was found 25 in order to allow the relations between the variables to be statistically analyzed with 95% confidence, with 75% power and with the level of relation r2= 0.5. A total of 28 patients were enrolled in the study with a margin of approximately 2% for the potential patient loss.
As regards the summary statistics of the measurements on the 28 children enrolled in the study, the qualitative variables were expressed as frequencies and percentage values, and the quantitative measurements were summarized in mean ± standard deviation (SD), and in median and minimum-maximum values. The relations to be examined were analyzed using the Spearman’s correlation coef fi cient, which is a nonparametric relation test. Results were considered statistically signi fi cant when P < 0.05. Statistical evaluations were carried out at 95% con fi dence level and were calculated using the SPSS for Windows version18.00 statistical software (SPSS Inc., Chicago, IL, USA).
Results
General data
General data and clinical characteristics of the subjects are listed inTable 1. Eighteen of the patients enrolled in our study were females (64%) and 10 were males (36%). Seventeen of the patients (61%) were given birth with a caesarian section. Mean age of the patients was 3.5 ± 2.3 (1-10) years. In the muscle test performed, 13 patients (44.8%) had no movements in their lower extremity muscles including the pelvic elevation and they were at level 5. Sixteen of the patients (54%) were non-ambulatory according to Hoofer ambulation classi fi cation. The lesion levels examined in the study were divided into two groups, namely the low lesion levels to include lumbosacral lesions, and the high lesion levels to include the mid-lumbar, high lumbar and thoracic lesions. Clinical properties of the patients are shown inTable 1.
Correlation between functional capacity and clinical features
Distribution of the mean raw and scale scores of SC, MO and SF fi elds of PEDI FS and CS according to the lesion level groups for the patients are respectively given inFigures 1, 2. The raw and scale scores in the three fi elds of both the functional skills scale and caregiver scale were found lower compared to the normal population data. The relation between the sub-scales of PEDI and spasticity, joint contractures, hip dislocation, spinal deformity and presence of mental retardation and the relations between the ambulation level and muscle tests are presented inTable 2.
Statistically significant relations were observed between the SC values of the FS and CA measurements, which were positive with age and negative with FAS and muscle test (respectively, for FS-SC, age: r = 0.628, P = 0.001, FAS: r = -0.506, P = 0.008, muscle test: r = -0.438, P = 0.025; for CA, age: r = 0.455, P = 0.019, FAS: r = -0.477, P = 0.014, muscle test: r = -0.498, P = 0.010) (Figures 3, 4). A positive relation was found between FS-MO area and age (r = 0.413, P = 0.036), a negative relation with FAS (r = -0.447, P = 0.022), and a negative relation was found for muscle test (r = -0.448, P = 0.022) (Figure 5). A negative relation was found between CA-MO and FAS (r = -0.414, P = 0.036), and a negative relation with the muscle test (r = -0.600, P = 0.001) (Figure 6). A significant relation was observed between FS and CA SF values and age (FS, r = -0.605, P = 0.001; CA, r = -0.536, P = 0.005). With the exception of the scores in CAMO fields, these relations show in general that FS and CAmeasurements signi fi cantly increased with age, and FAS and muscle test results improve with increased SC and MO values in FS and CA measurements. A positive, statistically significant relation was observed between the scores obtained for FS-SC values and the spinal deformity (r = 0.454, P = 0.020). The SC values in FS measurements also increased with the increasing spinal deformity. A negative relation was observed between the scores obtained for CA-SC values and mental retardation (r = -0.476, P = 0.014). The SC values in CA measurements decreased with the presence of mental retardation.
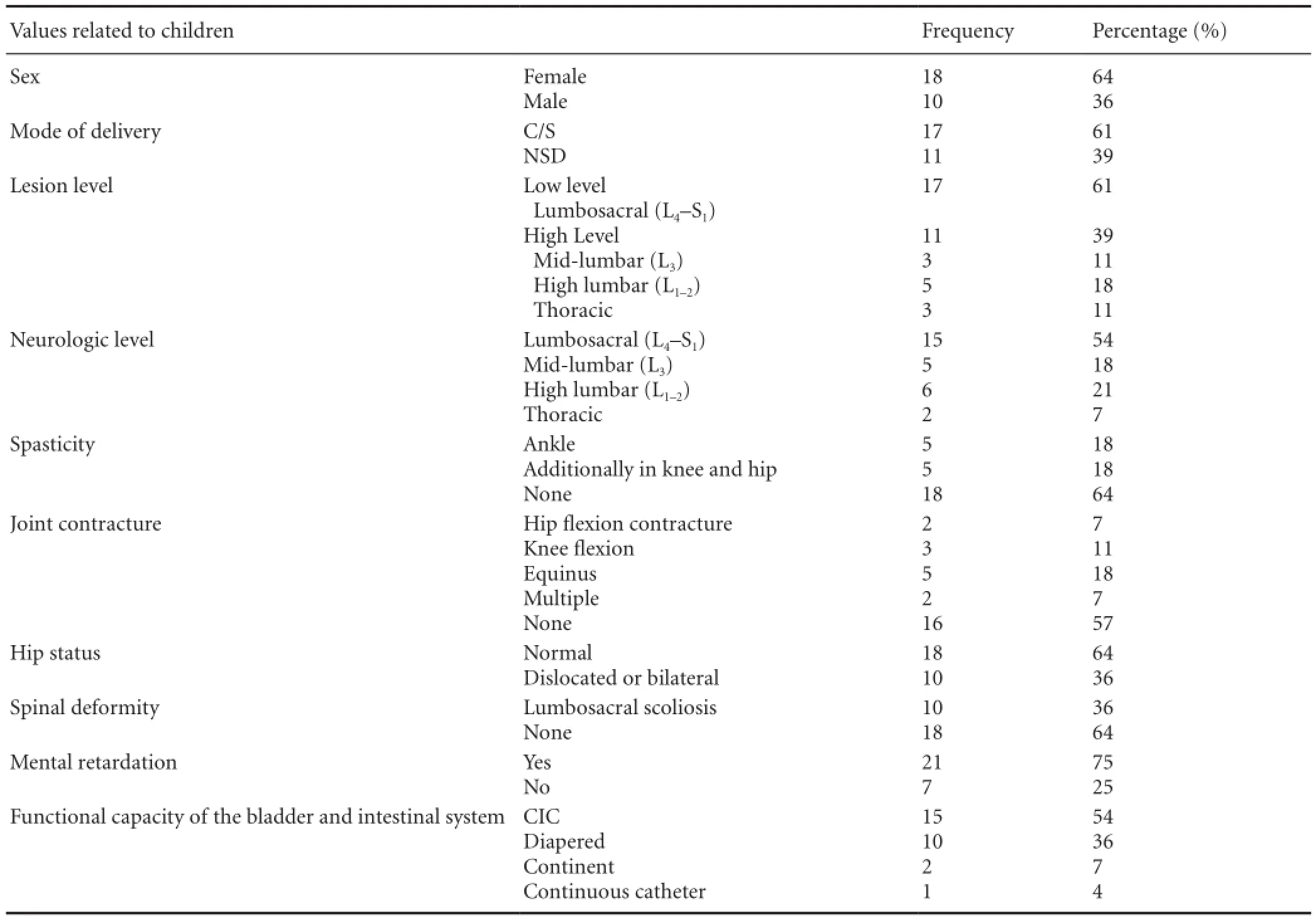
Table 1 General data and clinical characteristics of involved children
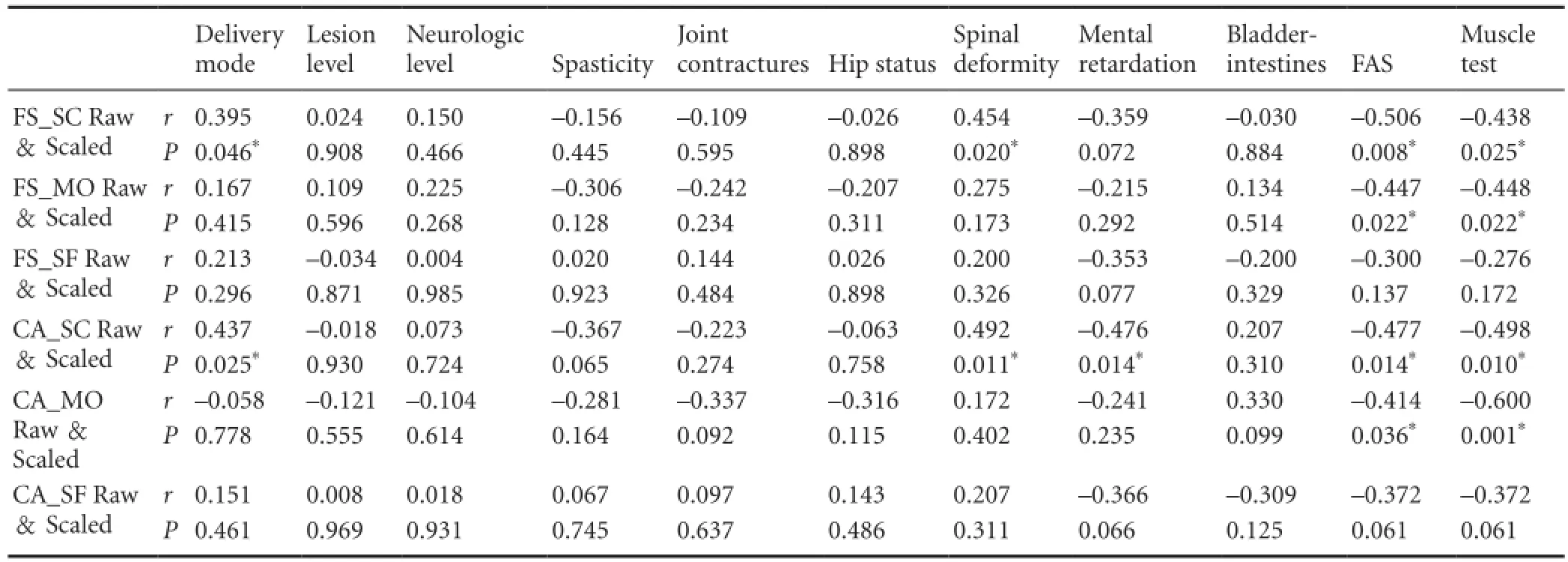
Table 2 Qualitative variable relation analysis with FS and CA measurements
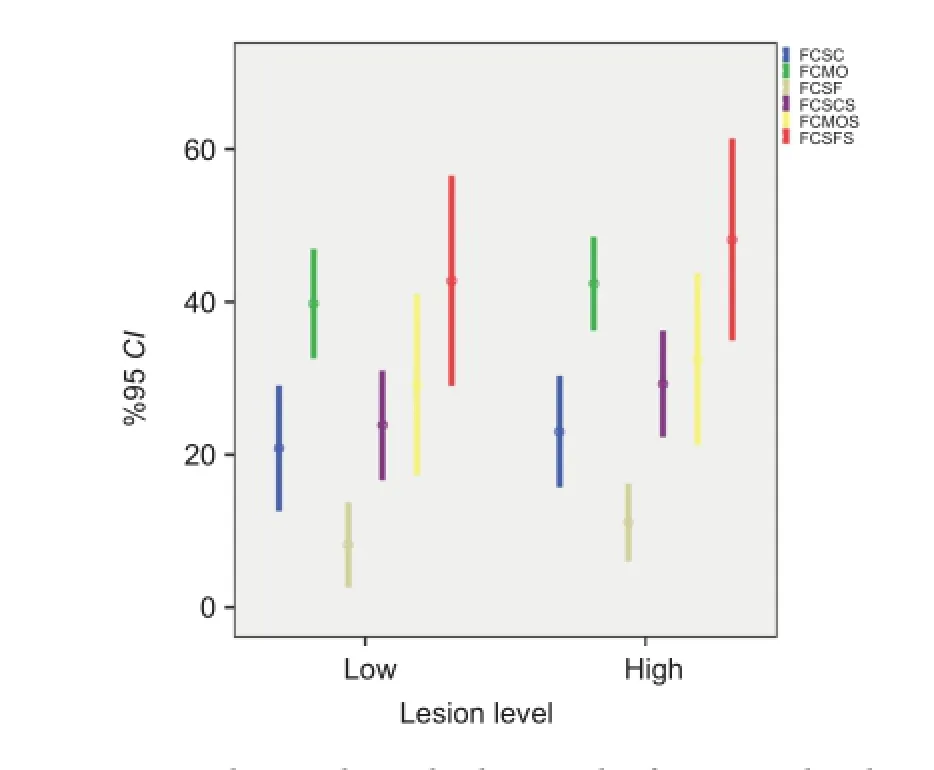
Figure 1 Mean values and standard error plot for raw and scale scores for Functional Ambulation Scale measurements of the lesion level.
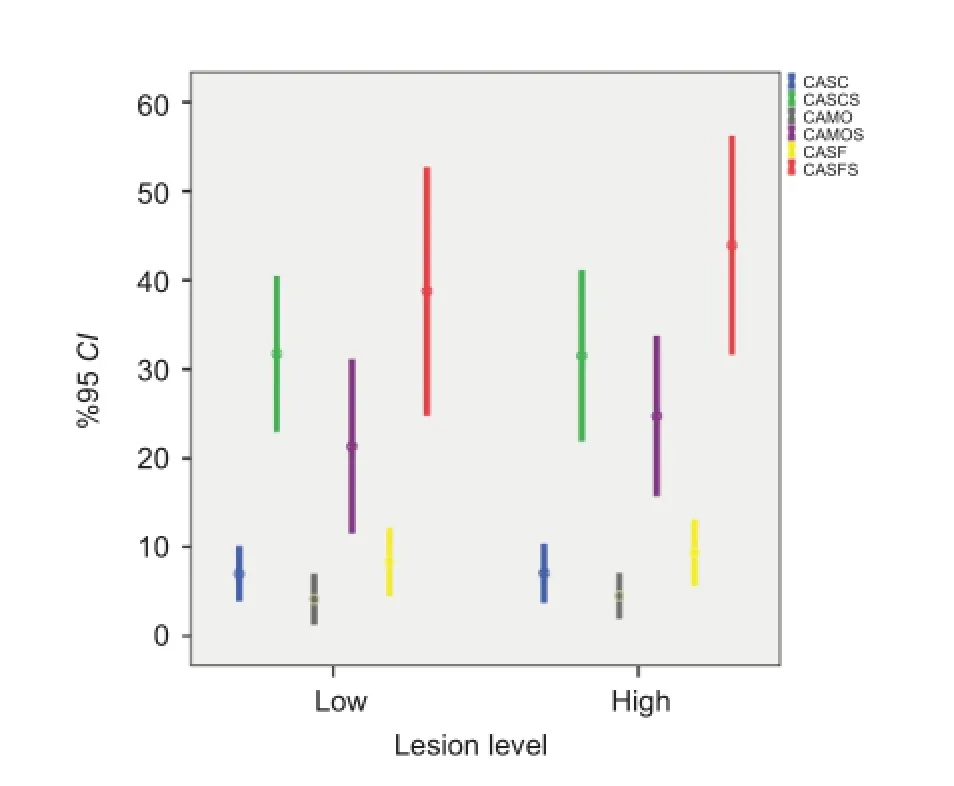
Figure 2 Mean values and standard error plot for raw and scale scores of the lesion levels.
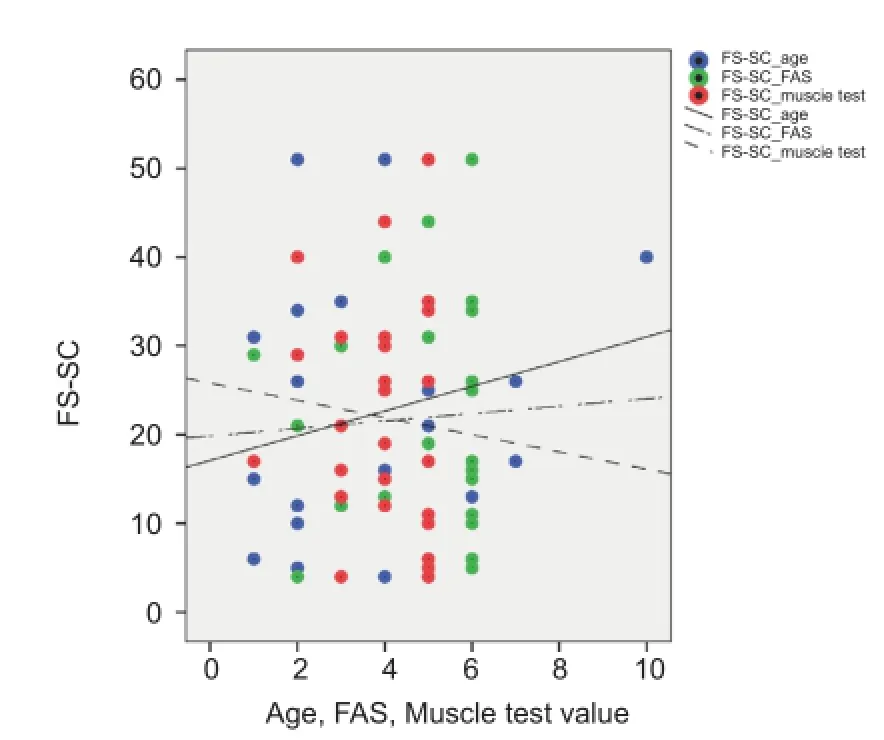
Figure 3 Statistically signi fi cant relations were observed between the self-care (SC) values of the Functional Skills Scales (FS) measurements which were positive with age and negative with Functional Ambulation Scale (FAS) and Muscle test.
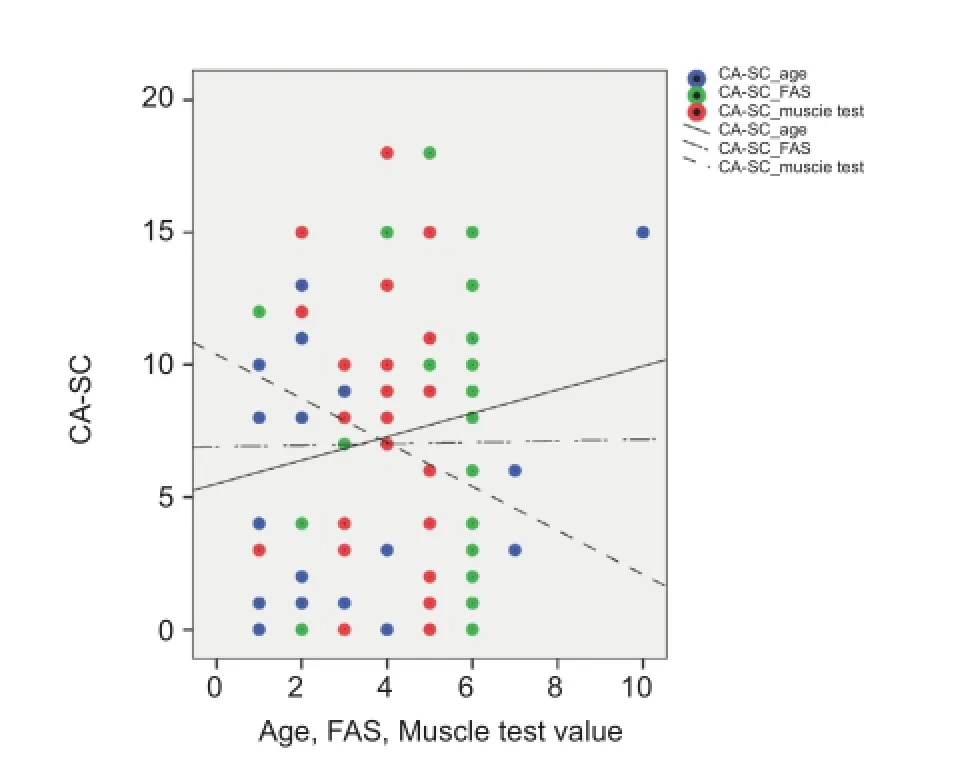
Figure 4 Statistically signi fi cant relations were observed between the self-care (SC) values of the Caregiver Assistance Scale (CA) measurements which were positive with age and negative with Functional Ambulation Scale (FAS) and Muscle test.
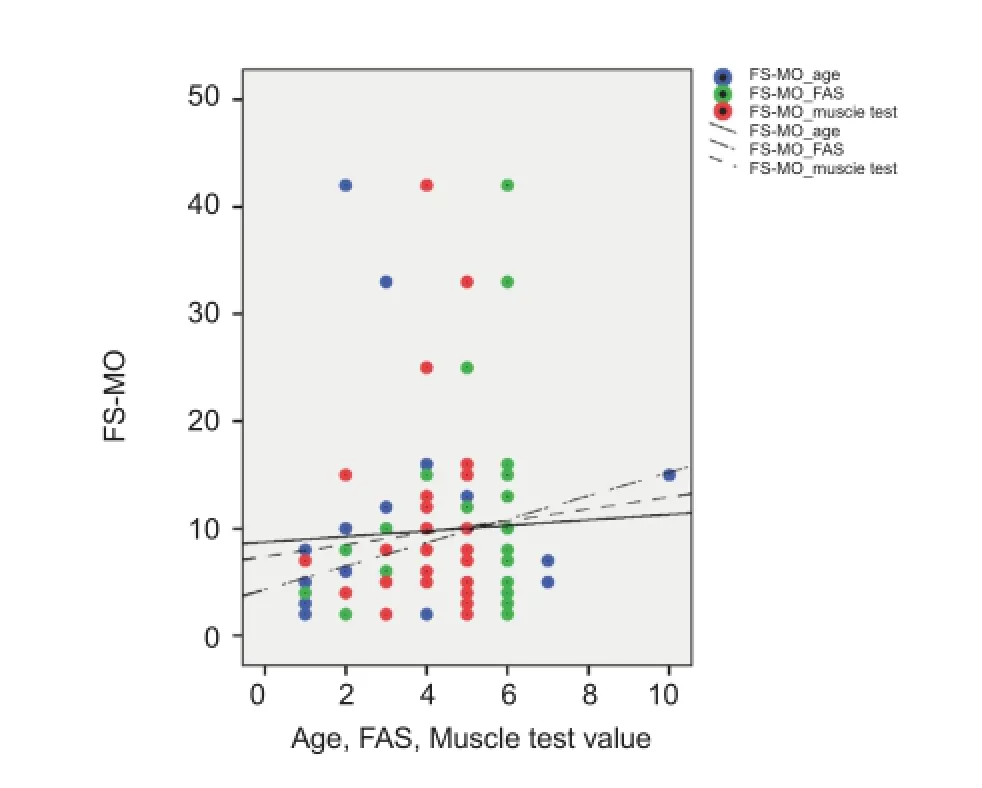
Figure 5 A positive relation was found between the mobility (MO) values of the Functional Skills Scale (FS) measurements and age, a negative relation with Functional Ambulation Scale (FAS), and a negative relation was found for muscle test.
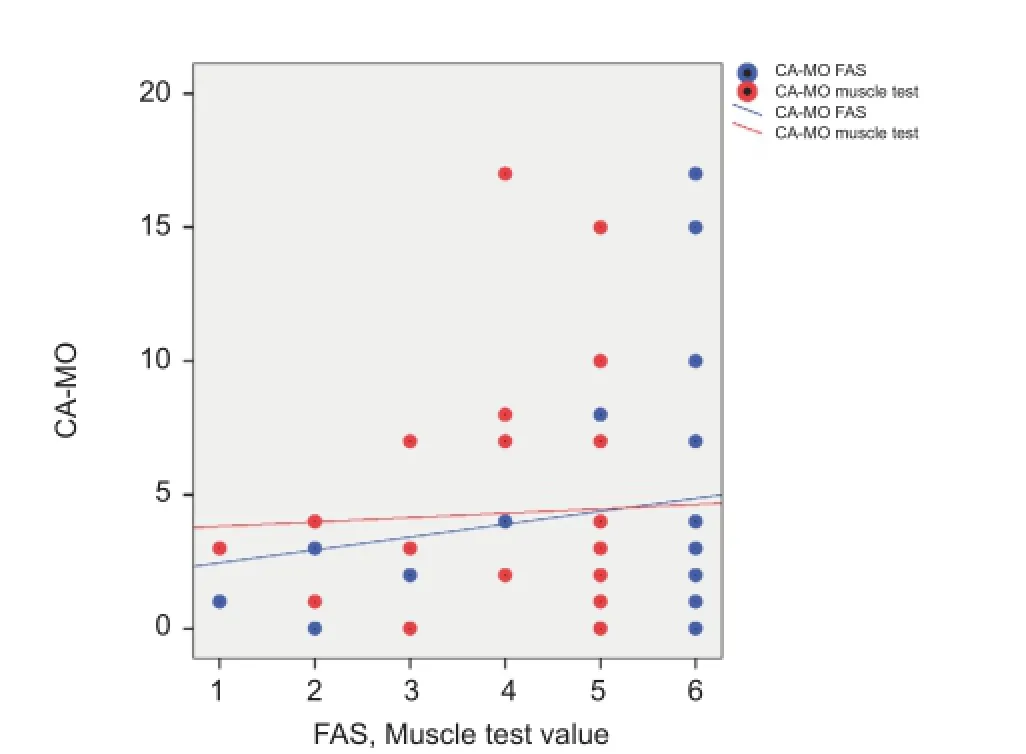
Figure 6 A negative relation was found between the mobility (MO) values of the Caregiver Assistance Scale (CA) measurements and Functional Ambulation Scale (FAS), and a negative relation with the muscle test.
Discussion
We detected an increase in caregiver dependency and an insuf fi ciency in functional skills in children with SB when we reviewed the results of PEDI daily life activity test of these children in our study. This increased dependency was signi ficantly higher in the group with high level lesions in comparison with low level lesion groups. The relation between the lesion levels and daily living activities has been investigated in many studies, and it was emphasized that the dependence in daily living activities increased with the increasing lesion levels (Padua et al., 2002; Schoenmakers et al., 2005; Verhoef et al., 2006). Dahl et al. (2000) studied self-care skills in 35 young children with myelomeningocele. They found that many of these children were slow in the development of independence in self-care; 60% needed moderate or maximal caregiver assistance.
Deformities that may cause functional disability, inadequacy of mobility, neurogenic bladder and intestinal problems, and pulmonary problems appear in patients with SB, at the early or late stages depending on lesion levels. Damages in those areas all negatively affect the functional independence. Since these problems mostly cause functional restrictions in the adolescent group, the adolescent group was included in many studies carried out to evaluate the daily living activities of the SB patients (Cate et al., 2002; Verhoef et al., 2006; Barf et al., 2010; Flanagan et al., 2011). We used PEDI in our study to evaluate the daily living activities of children with SB. As PEDI is mostly used for disabled children between 6 months to 7.5 years of age, the ages of our subjects in our study were selected in this range, with the mean of 3.5 ± 2.3 (1-10) years. There are also studies in which PEDI was used for patients older than 7.5 years (Steenbeek et al., 2011; Elad et al., 2012). We found out that functional independence increases with age in our study. This is natural, since as the child grows older, functional independence increases with the physical status.
In the present study, patients with inadequate ambulation levels and inadequate lower extremity muscular strength obtained lower points in both the functional skills scale and caregiver assistance fi elds of PEDI mobility domain. Tsai et al. (2002) evaluated the functional performances of children with MMC and lipomeningomyeleocele using PEDI. Results showed that there was a signi fi cant correlation between the neurologic level and walking skills with the self-care and mobility fi elds of PEDI in children with MMC. Danielsson et al. (2008) showed in their study that patients with higher muscular strengths in their lower extremities were mostly ambulatory, and all the ambulatory patients had quadriceps muscle strength at the level of 4 to 5. Our fi ndings were also consistent with other studies (Mazur et al., 1991; McDonald et al., 1991; Schoenmakers et al., 2005). Bartonek et al. (2001) divided their 53 MMC patients into fi ve groups according to muscular strength based on manual fi ndings. They employed the mobility domains of PEDI for the functional mobility, and they stated that the use of PEDI would be appropriate to show the decreased functional mobility. Other studies showed that the muscle weakness in lower extremities is a better diagnostic symptom in comparison with lesion levels in measuring independence in mobility. Muscular strength of knee extensors is especially important in functions such as stair climbing, indoor and outdoor ambulation and independence in transfers (Schoenmakers et al., 2005). In another study, lower extremity muscle weakness and impairment was shown to have a strong relationship with the functional loss and therefore, the decreased quality of life (Padua et al., 2004).
Spasticity is also an important factor for walking. Presence of spasticity around the hip and knee is an important factor for the formation of contractures and for the inadequacy of the walking function (Bartonek and Saraste, 2001). Like spasticity, contracture is also an effective condition for walking and functional performance (Schoenmakers et al., 2005). We determined no statistical relation in our study between spasticity/contracture and the subgroups of PEDI. The small mean age of our patients may indicate a period during which the negative effects of spasticity have not emerged yet and the effects of contractures in the daily life have not started yet. However, determining the presence of spasticity is an important factor when planning the rehabilitation program and when evaluating paralysis (Bartonek et al., 1999). In other studies, contracture was found to be an important factor of measuring independence on mobility. Preventing contracture development or treating the existing contracture by rehabilitation or surgery was shown to increase the mobility independence (Schoenmakers et al., 2005).
One of the limitations of our study was the review of mental status. We used only the patient history and patient fi le for review. No other tests were performed. We found that in patients with mental retardation, functional skills were low and caregiver assistance need was high. In another study (Schoenmakers et al., 2005), IQ test (WISC-R) was used to review the mental status of the children older than 4 years of age. The children were de fi ned as “normal” when the IQ was higher than 80. Similar to our results, these authors also reported that low intelligence is an important factor in functional independence. The main limitation of the study is the small sample size, which in fl uences the precision of the results and the statistical power of the tests.
Taken together, the functional performance of the children was found to be low and the children have an increased need of caretaker assistance. Low-level lesions, encouraging muscular strength, no mental retardation and independence in mobility are all very important factors for functional independence.
Acknowledgments:We wish to express our thanks to all our patients with myelomeningocele who were enrolled in our study and to their families. We also thank to the members of the Spina Bifida Council for their contribution.
Author contributions:Sirzai H designed the study, collected the data, analyzed and interpreted the data, performed statistical analysis, wrote and revised the paper. Dogu B designed the study and collected the data. Demir S collected the data. Yilmaz F and Kuran B provided administrative and technical support and supervised this study. All authors approved the final version of this paper.
Con fl icts of interest:None declared.
Alfarra HY, Alfarra SR, Sadiq MF (2011) Neural tube defects between folate metabolism and genetics. Indian J Hum Genet 17: 126-131.
Andrén E, Grimby G (2000) Dependence and perceived difficulty in activities of daily living in adults with cerebral palsy and spina bi fi da. Disabil Rehabil 22:299-307.
Barf HA, Post MW, Verhoef M, Gooskens RH, Prevo AJ (2010) Is cognitive functioning associated with subjective quality of life in young adults with spina bi fi da and hydrocephalus? J Rehabil Med 42:56-59.
Bartonek A, Saraste H, Knutson LM (1999) Comparison of different systems to classify the neurological level of lesion in patients with myelomeningocele. Dev Med Child Neurol 41:796-805.
Bartonek A, Saraste H (2001) Factors in fl uence ambulation in myelomeningocele: a cross-sectional study. Dev Med Child Neurol 43:253-260.
Bohannon RW, Smith MB (1987) Interrater reliability of a modified Ashworth scale of muscle spasticity. Phys Ther 67:206-207.
Buran CF, Sawin KJ, Brei TJ, Fastenau PS (2004) Adolescents with myelomeningocele: activities, beliefs, expectations, and perceptions. Dev Med Child Neurol 46:244-252.
Cate IM, Kennedy C, Stevenson J (2002) Disability and quality of life in spina bi fi da and hydrocephalus. Dev Med Child Neurol 44:317-222.
Custers JW, Wassenberg-Severijnen JE, Van der Net J, Vermeer A, Hart HT, Helders PJ (2002) Dutch adaptation and content validity of the‘Pediatric Evaluation Of Disability Inventory (PEDI)’. Disabil Rehabil 24:250-258.
Dahl M, Ahlsten G, Butler A, Norrlin S, Strinnholm M, Winberg A (2000) Self-care skills in young children with myelomeningocel. Eur J Pediatr Surg 10:52-53.
Danielsson AJ, Bartonek A, Levey E, McHale K, Sponseller P, Saraste H (2008) Associations between orthopaedic finding, ambulation and health-related quality of life in children with myelomeningocele. J Child Orthop 2:45-54.
Davis BE, Daley CM, Shurtleff DB, Duguay S, Seidel K, Ellenbogan RG (2005) Long-term survival of individuals with myelomeningocele. Pediatr Neurosurg 41:186-191.
Dicianno BE, Kurowski BG, Yang JMJ, Chancellor MB, Bejjani GK, Fairman AD, Lewis N, Sotirake J (2008) Rehabilitation and medical management of the adult with spina bi fi da. Am J Phys Med Rehabil 87:1026-1050.
Elad D, Barak S, Eisenstein E, Bar O, Herzberg O, Brezner A (2012) Reliability and validity of Hebrew Pediatric Evaluation of Disability Inventory (PEDI) in children with cerebral palsy -- health care professionals vs. mothers. J Pediatr Rehabil Med 5:107-115.
Erkin G, Elhan AH, Aybay C, Sirzai H, Ozel S (2007) Validity and reliability of the Turkish translation of the Pediatric Evaluation of Disability Inventory (PEDI). Disabil Rehabil 29:1271-1279.
Feldman AB, Haley SM, Coryell J (1990) Concurrent and construct validity of the Pediatric Evaluation of Disability Inventory. Phys Ther 70:602-610.
Flanagan A, Gorzkowski M, Altiok H, Hassani S, Ahn KW (2011) Activity level, functional health, and quality of life of children with myelomeningocele as perceived by parents. Clin Orthop Relat Res 469:1230-1235.
Gannotti ME, Cruz C (2001) Content and construct validity of a Spanish translation of the Pediatric Evaluation of Disability Inventory for children living in Puerto Rico. Phys Occup Ther Pediatr 20:7-24.
Haley SM, Coster WJ, Ludlow LH, Haltiwanger JT, Andrellos PJ (1999) Pediatric Evaluation of Disability Inventory: Development, Standardization, and Administration Manual. Boston, MA: New England Medical Center Inc., and PEDI Research Group.
Hoofer MM, Feiwell E, Perry R, Perry J, Bonnet C (1973) Functional ambulation in patients with myelomeningocele. J Bone Joint Surg Am 55:137-148.
Kothari DH, Haley SM, Gill-Body KM, Dumas HM (2003) Measuring functional change in children with acquired brain injury (ABI): Comparison of generic and ABI-specific scales using the Pediatric Evaluation of Disability Inventory (PEDI). Phys Ther 83:776-785.
Mazur JM, Menelaus MB (1991) Neurologic status of spina bi fi da patients and the orthopedic surgeon. Clin Orthop Relat Res 264:54-64.
McDonald CM, Jaffe KM, Mosca VS, Shurtleff DB (1991) Ambulatory outcome of children with myelomeningocele: effect of lower-extremity muscle strength. Dev Med Child Neurol 33:482-490.
Müller-Godeffroy E, Michael T, Poster M, Seidel U, Schwarke D, Thyen U (2008) Self-reported health-related quality of life in children and adolescents with myelomeningocele. Dev Med Child Neurol 50:456-461.
Nordmark E, Orban K, Hägglund G, Jarnlo GB (1999) The American Paediatric Evaluation of Disability Inventory (PEDI). Applicability of PEDI in Sweden for children aged 2.0-6.9 years. Scand J Rehabil Med 31:95-100.
Ostensjo S, Carlberg EB, Vollestad NK (2003) Everyday functioning in young children with cerebral palsy: Functional skills, caregiver assistance, and modi fi cations of the environment. Dev Med Child Neurol 45:603-612.
Padua L, Rendeli C, Rabini A, Girardi E, Tonali P, Salvaggio E (2002) Health-related quality of life and disability in young patients with spina bi fi da. Arch phys Med Rehabil 83:1384-1388
Padua L, Rendeli C, Ausili E, Aprile I, Caliandro P, Tonali P, Salvaggio E (2004) Relationship between the clinical-neurophysiologic pattern, disability, and quality of life in adolescents with spina bi fi da. J Child Neurol 19:952-957.
Rendeli C, Ausili E, Tabacco F, Caliandro P, Aprile I, Tonali P, Salvaggio E, Padua L (2005) Assessment of health status in children with spina bi fi da. Spinal Cord 43:230-235.
Schoenmakers MA, Uiterwaal CS, Gulmans VA, Gooskens RH, Helders PJ (2005) Determinants of functional independence and quality of life in children with spina bi fi da. Clin Rehabil 19:677-685.
Sirzai H, Erkin G, Culha C, Ozel S. (2008) Measuring Functional Change in Turkish Children with Cerebral Palsy Using the Pediatric Evaluation of Disability Inventory (PEDI) Turk J Med Sci 38:555-560.
Srsen KG, Vidmar G, Zupan A (2005) Applicability of the pediatric evaluation of disability inventory in Slovenia. J Child Neurol 20:411-416.
Steenbeek D, Gorter JW, Ketelaar M, Galama K, Lindeman E (2011) Responsiveness of Goal Attainment Scaling in comparison to two standardized measures in outcome evaluation of children with cerebral palsy. Clin Rehabil 25:1128-1139.
Tarazi RA, Zabel TA, Mahone EM (2008) Age-related differences in executive function among children with spina bi fi da/hydrocephalus based on parent behavior ratings. Clin Neuropsychol 22:585-602.
Tsai PY, Yang TF, Chan RC, Huang PH, Wong TT (2002) Functional investigation in children with spina bi fi da-measured by the Pediatric evalutation of Disability Inventory (PEDI). Child’s Nerv Syst 18:48-53.
Ulus Y, Tander B, Akyol Y, Ulus A, Tander B, Bılgıcı A, Kuru, Akbas S (2012) Functional disability of children with spina bi fi da: It’s impact on parents’ psychological status and family functioning. Dev Neurorehabil 15:322-328.
Verhoef M, Barf HA, Post MW, van Asbeck FW, Gooskens RH, Prevo AJ (2004) Secondary impairments in young adults with spina bi fi da. Dev Med Child Neurol 46:420-427.
Verhoef M, Barf HA, Post MW, van Asbeck FW, Gooskens RH, Prevo AJ (2006) Functional independence among young adults with spina bifi da, in relation to hydrocephalus and level of lesion. Dev Med Child Neurol 48:114-119.
Vinck A, Nijhuis-van der Sanden MW, Roeleveld NJ, Mullaart RA, Rotteveel JJ, Maassen BA (2010) Motor pro fi le and cognitive functioning in children with spina bi fi da. Eur J Paediatr Neurol 14:86-92. Wassenberg-Severijnen JE, Custers JW, Hox JJ, Vermeer A, Helders PJ (2003) Reliability of the Dutch Pediatric Evaluation of Disability Inventory (PEDI). Clin Rehabil 17:457-462.
Copyedited by Hwang CH, Li CH, Song LP, Zhao M
10.4103/1673-5374.135332
Hulya Sirzai, M.D., Ankara Physical
Medicine and Rehabilitation Education and Research Hospital, Ankara, Turkey, hsirzai@gmail.com.
http://www.nrronline.org/
Accepted: 2014-05-24
- 中国神经再生研究(英文版)的其它文章
- Recovery of the corticospinal tracts injured by subfalcine herniation: a diffusion tensor tractography study
- Prolonged electrical stimulation causes no damage to sacral nerve roots in rabbits
- Autophagy: a double-edged sword for neuronal survival after cerebral ischemia
- Diffuse axonal injury after traumatic cerebral microbleeds: an evaluation of imaging techniques
- Implanting iodine-125 seeds into rat dorsal root ganglion for neuropathic pain: neuronal microdamage without impacting hind limb motion
- Overexpression of microRNA-124 promotes the neuronal differentiation of bone marrow-derived mesenchymal stem cells

