低水平高密度脂蛋白胆固醇是经皮冠脉介入术后急性肾损伤的危险因素
陈永利 许静 刘园园 杨世诚 丛洪良 付乃宽

DOI:10.3760/cma.j.issn.1671-0282.2014.09.016
基金項目:天津市卫生局科技基金重点攻关项目(10KG122)
作者单位:300051 天津,天津市胸科医院心内科
通信作者:付乃宽,Email:drfnk2013@163.com
【摘要】目的 探讨低水平高密度脂蛋白胆固醇(high-density lipoprotein cholesterol, HDL-C)与冠心病患者经皮冠状动脉介入术(percutaneous coronary intervention, PCI)后对比剂诱导的急性肾损伤(contrast induced-acute kidney injury, CI-AKI)的关系。
方法 选取天津市胸科医院心内科2009年1月至2011年5月行PCI术的冠心病患者共1500例,于术前及术后72 h内测定其血肌酐水平。入选标准:均为汉族人群,年龄及性别不限;排除标准:既往有恶性肿瘤、泌尿系统感染、肾脏切除手术、腹膜或血液透析治疗或术前两周内曾应用过对比剂。CI-AKI定义为应用对比剂后24~72 h血清肌酐水平较原有基础升高超过25%或绝对值升高44.2 μmol/L以上,并排除其他影响肾功能的原因。低水平HDL-C定义为HDL-C< 1.04 mmol/L。应用单因素分析及多元Logistic回归分析确定CI-AKI及低水平HDL-C的危险因素。
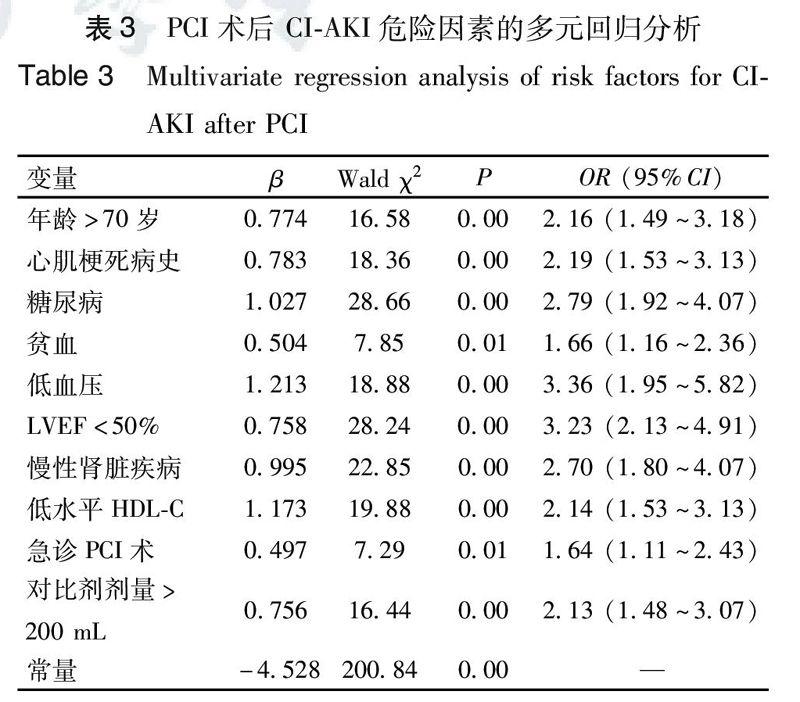
结果 在1500例行PCI术的冠心病患者中,共有246例(16.4%)发生了CI-AKI,低水平HDL-C组与正常水平HDL-C组的CI-AKI发病率分别为21.5%和13.3%(P<0.01)。进一步分析发现,伴有慢性肾脏疾病者,CI-AKI发病率在低水平HDL-C组与正常水平HDL-C组分别为39.8% 和26.5%(P<0.05),而在不伴有慢性肾脏疾病者分别为9.7% 和17.7%(P<0.01),差异均具有统计学意义。多元Logistic回归分析显示,低水平HDL-C是冠心病患者PCI术后CI-AKI发生的危险因素,超重、吸烟及贫血是该类患者低水平HDL-C的预测因子。
结论 与HDL-C水平正常者相比,低水平HDL-C者PCI术后CI-AKI的发病率显著升高。无论是否伴有慢性肾脏疾病,低水平HDL-C均是冠心病患者PCI术后发生CI-AKI的危险因素。超重、吸烟及贫血是低水平HDL-C的预测因子。
【关键词】 高密度脂蛋白胆固醇;经皮冠状动脉介入治疗;急性肾损伤;对比剂
Low level of high-density lipoprotein cholesterol predicts contrast induced-acute kidney injury after percutaneous coronary interventions in patients with coronary heart disease
Chen Yongli,Xu Jing,Liu Yuanyuan,Yang Shicheng,Cong Hongliang, Fu Naikuan.Department of Cardiology,Tianjing Chest Hospital,Tianjing 300051,China
Corresponding author: Fu Naikuan, Email: drfnk2013@163.com
【Abstract】Objective To investigate the relationship of low level of high-density lipoprotein cholesterol to contrast induced-acute kidney injury(CI-AKI)after percutaneous coronary intervention (PCI) in patients with coronary heart disease.Methods A total of 1500 consecutive patients,who underwent PCI from January 2009 to May 2011,were enrolled in this study. There was no limit on age or sex, and all patients were self-identified as Han ethnic group. Patients were excluded from this study, however, if they had a history of malignant tumor, urinary tract infection, nephrectomy operation, chronic peritoneal or hemodialysis, or if they had been exposed to contrast media within the past 14 days. CI-AKI was defined as an absolute increase in serum creatinine ≥44.2 μmol/L or a relative ≥25% increase in serum creatinine within 72 hours after procedure. Low level of HDL-C was defined as <1.04 mmol/L. Monofactorial and multivariate analysis was performed to identify risk factors for CI-AKI and low level of HDL-C in these patients. Results Among the 1500 patients with coronary heart disease, CI-AKI occurred in 246 patients after PCI and the overall incidence of CI-AKI was 16.4%. The patients with low level of HDL-C had a higher incidence of CI-AKI than those without it(21.5% vs. 13.3% in total,P<0.01),no matter that they had suffered from chronic kidney disease(39.8% vs. 26.5%,P<0.05)or not(17.7% vs. 9.7%,P<0.01). By multivariate analysis, low level of HDL-C was identified as an independent risk factor for CI-AKI and smoke, great BMI as well as anemia were considered as prediction factors for low level of HDL-C. Conclusion The patients with low level of HDL-C have a higher incidence of CI-AKI after PCI. Low level of HDL-C is one of risk factors for CI-AKI after PCI in patients either with chronic kidney disease or not. Great BMI,smoking as well as anemia are independent predictors for low HDL-C level in these patients.
【Key words】 High-density lipoprotein cholesterol; Percuta neous coronary intervention; Acute kidney injury; Contrast
对比剂诱导的急性肾损伤(contrast induced-acute kidney injury, CI-AKI)是指应用对比剂后24~72 h血清肌酐水平较原有基础升高超过25%或绝对值升高44.2 μmol/L以上,并排除其他影响肾功能的原因[1]。文献报道,CI-AKI已成为继外科手术及药物之后院内获得性肾损害的第三大原因[2]。一旦发生CI-AKI,患者的住院时间、住院费用、心脏不良事件及病死率将显著增加,生活质量也将受到严重影响[3]。有研究表明,高密度脂蛋胆固醇(high-density lipoprotein cholesterol, HDL-C)不但具有显著的心血管保护作用,还可明显改善缺血所致的急性肾损伤[4-6]。遗憾的是,HDL-C与冠心病患者经皮冠状动脉介入术(percutaneous coronary intervention, PCI)后CI-AKI关系如何,国内外鲜有报道。因此,本研究将就低水平HDL-C是否为CI-AKI的危险因素进行探讨。
1 资料与方法
1.1 一般资料
选取天津市胸科医院心内科2009年1月至2011年5月行PCI术的冠心病患者共1500例,于术前及术后72 h内测定其血肌酐水平。入选标准:均为汉族人群, 年龄及性别不限;排除标准:既往有恶性肿瘤、泌尿系统感染、肾脏切除手术、腹膜或血液透析治疗或术前两周内曾应用过对比剂。
1.2 治疗方案
入选患者接受如下标准水化治疗方案:PCI术前12 h及术后以1 mL/(kg·h)静脉点滴0.9%生理盐水各持续约12 h。对于左室射血分数(left ventricular ejection fraction, LVEF)< 50%者,则减为0.5 mL/(kg·h)。行急诊PCI术者入院时即应用水化治疗。同时,所有患者PCI术中应用的对比剂均为碘克沙醇320(商品名 visipaque, 瑞典安盛公司)。术前均给予阿司匹林300 mg、氯吡格雷300 mg作为负荷剂量;PCI后给予低分子肝素0.4~0.6 mL/12 h,皮下注射5~7 d,阿司匹林100 mg/d、氯吡格雷75 mg/d,服用1年。
1.3 资料收集
1.3.1 临床资料 年龄、性别、体质量指数、吸烟史、心肌梗死病史、糖尿病、贫血、LVEF、PCI术类型(急诊或择期)、慢性肾脏疾病(chronic kidney disease, CKD)、利尿剂、钙离子拮抗剂、β受体阻滞剂、ARB/ACEI等药物的应用及对比剂剂量等。
1.3.2 生化指标 术前及术后24~72 h 血肌酐、术前肾小球滤过率(estimated glomerular filtration rate, eGFR)、血常规、血糖、纤维蛋白原、血尿酸及血脂等。
1.4 诊断标准
1.4.1 CI-AKI 使用对比剂后24~72 h内,血肌酐水平较原有基础升高25%或者绝对值升高44.2 μmol/L以上,并排除其他影响肾功能原因。
1.4.2 低水平HDL-C HDL-C <1.04 mmol/L;CKD:eGFR<60 mL/(min·1.73 m2),eGFR[mL/(min·1.73 m2)]= 186.3×(血肌酐/88.4)-1.154×年龄-0.203×(1 男性;0.742 女性);糖尿病:具有典型症状,空腹血糖>7.0 mmol/L或餐后血糖>11.1 mmol/L;超重:体质量指数>25 kg/m2;高尿酸血症:入院时血尿酸含量测定在男性或绝经后女性>420 μmol/L或在未绝经女性>350 μmol/L。
1.5 统计学方法 采用SPSS 10.0统计软件进行统计学分析。计量资料采用(x±s)表示,计数资料采用例(%)表示。计量资料间比较采用独立样本t检验,计数资料采用χ2检验。应用多元Logistic回归分析确定CI-AKI及低水平HDL-C的危险因素,以P<0.05为差异具有统计学意义。
2 结果
2.1 低水平HDL-C组与正常水平HDL-C组基本资料比较
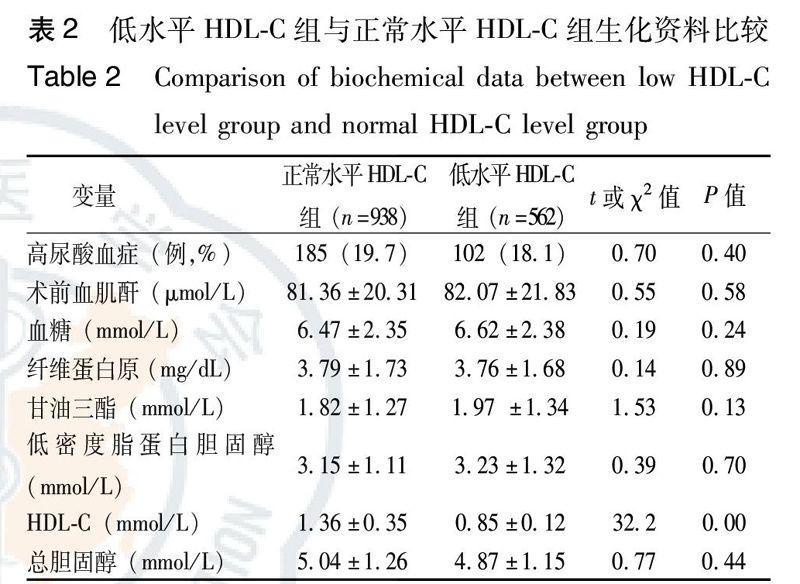
与正常水平HDL-C组相比,低水平HDL-C组在超重、吸烟史、心肌梗死病史、LVEF< 50%、贫血等方面具有较高比例,差异具有统计学意义(P<0.05)。而在年龄、性别、糖尿病、CKD、急诊PCI、钙离子拮抗剂、β受体阻滞剂、ARB/ACEI、对比剂应用剂量、高尿酸血症、术前血肌酐、血糖、纤维蛋白原、甘油三酯、低密度脂蛋白胆固醇以及总胆固醇等方面,两组间差异无统计学意义(P>0.05),结果见表1、表2。
3 讨论
冠心病患者PCI术后CI-AKI的发生并不少见,其发病率在普通人群约为15% [3,7],而肾功能不全者则可高达27%[8]。本研究入選了1500例行PCI术的冠心病患者,其发病率为16.4%,提示CI-AKI在该类患者中普遍存在,需引起临床医生高度重视。目前,对于PCI术后CI-AKI的发生尚无特殊有效的治疗方法。因此,探明其危险因素、筛选高危人群并进行积极预防以降低发病率则显得至关重要。
HDL-C是一类由多种载脂蛋白、脂质成分、相关酶类等组成的异质性脂蛋白颗粒,主要介导细胞胆固醇逆向转运,可直接抑制动脉粥样硬化形成。近期研究表明,HDL-C还具有抗炎、抗氧化作用,在缺血/再灌注引起的急性肾损伤中也具有肾保护作用[6,9]。本研究发现,在行PCI术的冠心病患者中,低水平HDL-C组与正常水平HDL-C组相比CI-AKI发病率显著增高。进一步分析发现,伴有CKD者,CI-AKI发病率在低水平HDL-C组与正常水平HDL-C组分别为39.8%和26.5%(P<0.05),而在不伴有CKD者分别为17.7%和9.7%(P<0.01),差异均具有统计学意义。可见,无论是否伴有CKD,低水平HDL-C组PCI术后CI-AKI的发生率均显著增高。经多元回归分析证实,同年龄>75岁、心肌梗死病史、糖尿病、贫血、心功能不全、CKD及对比剂剂量 >200 mL等致病因素一样,低水平HDL-C也是PCI术后CI-AKI发生的危险因素。另外,从表1不难发现,低水平HDL-C组与正常水平HDL-C组相比,有心肌梗死病史、LVEF<50%及贫血者比例较高,而这些因素经多元回归分析证实或文献报道均为CI-AKI的危险因素[10-12]。由此可见,危险因素的增多也是低水平HDL-C组CI-AKI发病率增高的重要原因[13-15]。
实验研究显示,HDL-C可以如下途径改善肾功能:(1)通过胆固醇的逆转运来抑制肾血管的动脉粥样硬化及脂质对肾细胞的直接毒性作用;(2)阻止脂蛋白的累积以减少低密度脂蛋胆固醇与肾小球系膜细胞受体的结合以及肾间质的生成[16];(3)抗氧化作用[17];(4)抑制细胞反应性氧基团的生成[18];(5)抑制黏附因子的表达以减少多形核白细胞对肾组织的浸润及氧化应激反应[19]。不难理解,由于低水平HDL-C可造成其肾保护作用下降,CI-AKI发生率可显著增高。
据报道,在普通人群,吸烟者的血浆HDL-C水平明显减低,吸烟是低水平HDL-C的独立预测因子[20-21]。本研究显示,吸烟也是冠心病患者低水平HDL-C的预测因子。除了吸烟以外,超重及贫血也是低水平HDL-C的预测因子。Lo等[22]也发现,无论是否伴有CKD,血浆HDL-C水平均与体质量指数负相关,体质量指数越高发生低水平HDL-C的可能性越大。至于贫血与低水平HDL-C的关系,尚需进一步深入探究。
总之,与HDL-C水平正常者相比,低水平HDL-C者PCI术后CI-AKI的发病率显著升高。回归分析表明,无论是否伴有CKD,低水平HDL-C均是冠心病患者PCI术后CI-AKI发生的危险因素。超重、吸烟及贫血是该类患者低水平HDL-C的预测因子。
参考文献
[1] McCullough PA.Contrast induced-acute kidney injury[J]. J Am Coll Cardiol,2008,51(15):1419-1428.
[2] Nash K, Hafeez A, Hou S. Hospital-acquired renal insufficiency[J]. Am J Kidney Dis,2002,39 (5):930-936.
[3] McCullough PA, Wolyn R, Rocher LL, et al. Acute renal failure after coronary intervention: incidence, risk factors, and relationship to mortality[J]. Am J Med,1997,103(5):368-375.
[4] Rallidis LS, Tellis CC, Lekakis J, et al. Lipoprotein-associated phospholipase A(2) bound on high-density lipoprotein is associated with lower risk for cardiac death in stable coronary artery disease patients: a 3-year follow-up[J]. J Am Coll Cardiol,2012,60(20):2053-2062.
[5] Sbrana F, Puntoni M, Bigazzi F, et al. High density lipoprotein cholesterol in coronary artery disease: when higher means later[J]. J Atheroscler Thromb,2013,20(1):23-31.
[6] Christoph T, Hristoph T, Espen K,et al. High density lipoprotein reduces renal ischemia/reperfusion injury[J]. J Am Soc Nephrol,2003,14 (7):1833-1843.
[7] Gao F, Zhou YJ, Zhu X, et al. C-reactive protein and the risk of contrast-induced acute kidney injury in patients undergoing percutaneous coronary intervention[J]. Am J Nephrol,2011,34(3):203-210.
[8] 嚴红,张黔桓,靳立军,等. 碘克沙醇与碘帕醇用于肾功不全患者行冠状动脉介入术的肾毒性对比[J]. 中华急诊医学杂志, 2008,17(1):72-75.
[9] Ansell BJ, Navab M, Watson KE, et al. Anti-inflammatory properties of HDL[J]. Rev Endocr Metab Disord,2004,5(4):351-358.
[10]Abe M, Kimura T, Morimoto T, et al. Incidence of and risk factors for contrast-induced nephropathy after cardiac catheterization in Japanese patients[J]. Circ J,2009,73 (8):1518-1522.
[11] 何飞,张均,卢中秋,等. 冠状动脉支架植入术后急性肾损伤的危险因素和预后分析[J]. 中华急诊医学杂志,2012,21(5):514-518.
[12] Nikolsky E, Mehran R, Lasic Z, et al. Low hematocrit predicts contrast- induced nephropathy after percutaneous coronary interventions[J]. Kidney Int,2005,67 (2):706-713.
[13] Mehran R, Aymong E, Nikolsky E, et al. A simple risk score for prediction of CIN after percutaneous coronary intervention: Developmen and innitial Validation[J]. J Am Coll Cardiol,2004,44(7): 1393-1399.
[14] Maioli M, Toso A, Gallopin M et al. Preprocedural score for risk of contrast induced nephropathy in elective coronary angiography and intervention[J]. J Cardiovasc Med (Hagerstown), 2010,11 (6):444-449.
[15] Fu N, Lia X, Yang S, et al. Risk Score for the Prediction of contrast-induced nephropathy in elderly patients undergoing percutaneous coronary intervention[J]. Angiology,2012,64 (3):188-194.
[16] Rader DL.Molecular regulation of HDL metabolism and function and implications for novel therapies[J].J Clin Invest,2006,116 (12):3090-3100.
[17] Abrass CK. Cellular lipid metabolism and the role of lipids in progressive renal disease[J]. Am J Nephrol,2004,24(1):46-53.
[18] Robbesyn F, Auge N, Vindis C, et al. High-density lipoproteins prevent the oxidized low-density lipoprotein-induced epidermal [corrected] growth factor receptor activation and subsequent matrixmetalloproteinase-2 upregulation[J]. Arterioscler Thromb Vasc Biol,2005, 25 (6):1206-1212.
[19] Athyros VG, Kakafika AI, Papageorgiou AA, et al. Statin-induced increase in HDL-C and renal function in coronary heart disease patients[J]. Open Cardiovasc Med J,2007,1 (28) :8-14.
[20] Schuitemaker GE, Dinant GJ, van der Pol GA, et al. Relationship between smoking habits and low-density lipoprotein-cholesterol, high-density lipoprotein-cholesterol, and triglycerides in a hypercholes terolemic adult cohort, in relation to gender and age[J]. Clin Exp Med, 2002,2 (2):83-88.
[21] Mizoue T, Ueda R, Hino Y, et al. Workplace exposure to Environmental tobacco smoke and high density lipoprotein cholesterol among nonsmokers[J]. Am J Epidemiol,1999,150 (10):1068-1072.
[22] Lo JC, Go AS, Chandra M, et al. GFR, body mass index, and low high-density lipoprotein concentration in adults with and without CKD[J]. Am J Kidney Dis,2007,50(4):552-558.
(收稿日期:2014-04-15)
(本文編辑:邵菊芳)
P1018-1022

