肘关节“恐怖三联征”的手术治疗:附14例报告
孟亚轲 刘岩 叶添文 欧阳跃平 陈爱民 郭永飞
肘关节“恐怖三联征”的手术治疗:附14例报告
孟亚轲 刘岩 叶添文 欧阳跃平 陈爱民 郭永飞
目的 回顾分析手术治疗肘关节“恐怖三联征”的疗效及策略。方法 我院骨科从2010年7月至2013年10月手术治疗并完整随访的14例肘关节“恐怖三联征”患者,其中尺骨冠突骨折按照Regan-Morrey分型:Ⅰ型2例,Ⅱ型10例,Ⅲ型2例;桡骨头骨折按照Mason 分型:Ⅰ型4例,Ⅱ型7例,Ⅲ型3例;本组病例中均合并有肘关节内、外侧副韧带的损伤。采取常规肘关节内、外侧联合入路,给予患肘关节复位,然后由深至浅依次固定冠状突骨折和桡骨头骨折,修复外侧副韧带。冠状突骨折采用微型钢板、拉力螺钉、缝合锚钉及套索缝合技术固定;桡骨头骨折采用克氏针、微型螺钉或微型钢板固定;所有患者给予编织非吸收性缝线缝合或锚钉修复外侧副韧带(lateral collateral ligaments,LCL),2例使用非吸收性编织缝线缝合、锚钉修复内侧副韧带(medical collateral ligaments,MCL),1例放置外侧铰链式外固定支架,余13例患者术后给予肘关节屈曲90°、前臂中立位石膏固定,术后积极进行康复功能锻炼。结果 平均随访18个月(10~37个月)。所有病例实现骨折愈合,平均愈合时间为12.4周。术后6个月,肘关节屈位(0°~20°),伸位(130°~145°),平均活动范围为116.5°;旋前(60°~85°),旋后(45°~75°),平均旋转范围为126°。1例患者出现肘关节僵硬;2例患者术后6个月在影像学上出现异位骨化,但不影响肘关节功能。结论 肘关节“恐怖三联征”通过积极有效的手术治疗,大多患者能够得到满意的结果。对于该类损伤,我们应尽可能通过有效的内固定重建骨及韧带的稳定结构,恢复肘关节的稳定性,及早配合正规的功能锻炼,最大程度恢复肘关节的功能。
肘关节;恐怖三联征;骨折;脱位;固定
肘关节“恐怖三联征”是指肘关节后脱位合并尺骨冠状突骨折和桡骨头骨折,常伴有肘关节内、外侧副韧带的损伤。轴向应力作用于前臂旋后、肘关节外展产生的压缩剪切力是主要的损伤机制[1]。我科自2010年7月至2013年10月手术治疗并完整随访了14例肘关节“恐怖三联征”患者,治疗效果较好,现报道如下。
资 料 与 方 法
一、一般资料
本组患者14例,男性11例,女性3例,年龄23~48岁,平均35.4岁。左侧5例,右侧9例,均为闭合性损伤。无相关神经血管损伤。致伤原因:高处坠落5例,交通事故3例,跌倒损伤4例,运动损伤2例。入院后常规行肘关节X线正侧位片、肘关节CT扫描及三维重建以判断骨折的类型及移位情况(图1、2)。尺骨冠突骨折Regan-Morrey分型[2],Ⅰ型2例,Ⅱ型10例,Ⅲ型2例;桡骨头骨折按照Mason 分型[3],Ⅰ型4例,Ⅱ型7例,Ⅲ型3例;其中1例合并有同侧桡骨远端骨折,1 例合并有同侧尺骨干骨折;本组病例均合并有肘内、外侧副韧带的损伤。
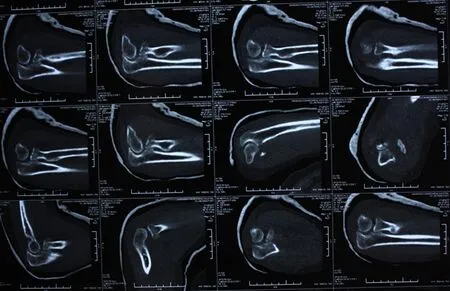
图2 肘关节CT平扫
二、手术方法
患者平卧于手术台上,患肢近端上充气性止血带。在臂丛神经阻滞麻醉下,常规使用肘关节内、外侧联合入路,给予患肘关节复位,然后由深至浅依次修复冠状突骨折,前关节囊,桡骨头骨折,外侧副韧带,伸肌总腱起点。冠状突骨折采用微型钢板、拉力螺钉、缝合锚钉或套索缝合技术固定;桡骨小头骨折采用克氏针、微型螺钉、微型钢板固定;所有患者使用非吸收性编织缝线缝合或锚钉给予修复外侧副韧带(lateral collateral ligaments,LCL)。闭合切口前行肘关节伸直位内外翻试验及外翻过载试验判断肘关节稳定性的恢复情况。其中3例肘关节被动屈曲过程中同心圆稳定性欠佳,其中2例使用非吸收性编织缝线缝合、锚钉修复内侧副韧带(medical collateral ligaments,MCL),1例放置外侧铰链式外固定支架,术中保持肘关节屈曲90°固定铰链,另12例稳定性尚可维持。术后13例患者给予肘关节屈曲90°、前臂中立位石膏固定。

图1 术前肘关节正侧位X线片
三、功能锻炼及随访
13例石膏固定患者做手指活动及肱二头肌、肱三头肌等长收缩训练;术后48 h开始进行肘关节被动屈伸活动,及前臂旋转活动。1例辅以外固定架固定的患者术后1~2周开始进行功能锻炼,术后第1周,调整铰链支架中心的旋钮,指导患肘做屈伸功能锻炼,术后6~8周拆除外固定支架。康复过程中避免肘关节过伸。 术后分别于第1天, 2周,1、3、6、12个月随访时拍摄患肘关节正侧位X线片。术后2个月肘关节正侧位X线片见图3。观察骨折块愈合及异位骨化、骨关节炎等术后并发症的发生情况;了解肘关节功能改善情况,指导患者进行功能锻炼。随访结束时按Mayo肘关节功能评分标准进行疗效评价。

图3 术后2个月肘关节正侧位X线片
结 果
本组随访14例,平均随访18个月(10~37个月)。骨折达临床愈合时间为术后10~15周,平均12.4周。术后6个月,肘关节屈位(0°~20°),伸位(130°~145°),平均活动范围为116.5°;旋前(60°~85°),旋后(45°~75°),平均旋转范围为126°。1例出现肘关节僵硬;2例患者术后6个月在影像学上出现异位骨化,但不影响肘关节功能。Mayo评分标准评价:优6例,良4例,一般2例,差1例。
讨 论
1996年Hotchkiss[4]首次将肘关节后脱位合并尺骨冠突和桡骨头骨折命名为肘关节“恐怖三联征”,该类患者多合并有周围韧带的损伤,属于严重类型的肘关节损伤。肘关节三维结构复杂,治疗不当会导致疼痛、僵硬、异位骨化、创伤性关节炎等并发症。肘关节“恐怖三联征”的主要治疗目标[5]是重建重要的骨性关节及软组织结构,恢复运动关节的稳定性,为术后早期功能锻炼提供条件。大多数学者[6]建议对所有骨折的桡骨头和冠突给予牢固固定,修复外侧副韧带,实现肘关节的解剖稳定性。在少数情况下,对于残存的不稳定性可通过修复内侧副韧带或加用铰链式外固定架固定治疗。
目前肘关节“恐怖三联征”常用的手术入路有外侧入路、外内侧联合入路和后侧入路。国内林国叶等[7]学者使用肘关节后方尺骨鹰嘴截骨入路治疗了8例肘关节“恐怖三联征”患者,该手术入路扩大了手术视野,减少了对正常组织的进一步损伤,可完成尺骨冠状突骨折、桡骨小头骨折及肘关节内外侧软组织的修复。
尺骨冠突是尺骨近端干骺部向前方的延伸部分,具有维持肘关节轴向稳定,后内侧、后外侧旋转稳定及防止肘内翻的重要作用,是维持肘关节前方稳定性最主要的骨性阻挡结构,也是防止肘关节后脱位、后外侧半脱位的第一位因素[8]。冠突骨折主要的手术固定方法有套索缝合技术、微型螺钉、微型钢板、锚钉等,具体的治疗方案要根据骨折块的大小、骨折类型及医师的偏好来决定。Garrigues等[9]发现在冠突骨折中,经骨套索缝合固定技术优于螺钉或锚钉固定,其治疗效果佳且并发症少。Jeon等[10]尸检发现在桡骨头及韧带完整的情况下(尤其是桡骨头)冠突缺少40%(Ⅱ型骨折)不会发生肘关节不稳定,认为Ⅱ型冠突骨折属于稳定性骨折。最近, Papatheodorou等[11]治疗了12例冠突Ⅰ型和Ⅱ型的肘关节“恐怖三联征”患者,所有患者给予肱尺关节复位,桡骨头的修复或假体置换,修复外侧副韧带,但冠突及前侧关节囊未予修复处理,术中所有病例获得稳定,未修复内侧副韧带及使用外固定架,术后患者患肢结构及功能恢复良好。此外,Alolabi等[12]在缺少40%的冠突骨折的尸体模型中,发现同侧尺骨鹰嘴尖部取骨植骨是重建冠突恢复正常运动力学的有效的方法,虽然这项技术仅适用于单纯性冠突骨折,且还处于研究阶段,但论证了冠突骨折缺损导致肘关节的不稳定。毫无疑问,冠突在肘关节稳定性中发挥关键性作用,我们建议对冠突骨折给予积极的内固定治疗,尤其是骨折块较大的Ⅱ型、Ⅲ型骨折(Regan-Morrey),而有些可能引起肘关节不稳定的Ⅰ型骨折也应该给予有效的内固定治疗。
桡骨头具有维持肘关节轴向及内外翻稳定的作用,在MCL损伤情况下其抗外翻作用尤为重要,在运动中可通过拉紧LCL间接提供抗内翻阻力。在肘关节“恐怖三联征”中,桡骨头骨折可使用钢板固定或桡骨头置换进行治疗。使用钢板固定骨折块时,需注意钢板应放置在“安全区”-桡骨头的非关节面,以防术后影响前臂的旋转功能[13]。桡骨头置换在桡骨头骨折中(尤其是在存在复杂类型的肘关节损伤中如:肘关节“恐怖三联征”)的应用一直是研究的热点。Watters等[14]发现在肘关节“恐怖三联征”中,与切开复位内固定病例组相比,桡骨头置换病例组患者的术中、术后及短期随访中肘关节的稳定性优于内固定治疗组,但桡骨头置换组的术后关节炎发生率高于内固定组。Ring 等也推荐肘关节“恐怖三联征”患者采用桡骨头置换治疗。此外,Acevedo等[3]认为当尺骨冠突骨折<50%时,肘关节“恐怖三联征”可以通过单纯的桡骨头关节置换和外侧尺骨副韧带修复手术进行治疗。也有学者认为Mason Ⅲ型的桡骨头骨折是无法重建的。因此,可对其进行桡骨头切除加桡骨头置换[15]。尽管桡骨头置换在材料、类型及技术方面都得到了快速的发展,但桡骨头置换之后带来的并发症及远期疗效仍然困扰着众多学者,其中假体松动作为桡骨头置换的一个远期并发症,是令众多学者担忧的问题,尤其是青年患者[13]。在我们的病例治疗组中,大多数桡骨头骨折能够通过内固定获得治疗,桡骨头置换不仅增加了患者的经济负担,而且远期疗效不明。因此,我们不主张进行桡骨头置换。
外侧副韧带是抗内翻应力的主要稳定结构,有利于支撑桡骨头、防止肘关节发生半脱位。在肘关节“恐怖三联征”中外侧副韧带复合体,通常自肱骨远端的起点处发生撕脱,可用不可吸收缝线或以带线“锚钉”缝合固定在肱骨远端,此时检查肘关节的稳定性,肘关节由伸直位到屈曲位,如果屈曲未达30°~40°时即发生脱位,可以运用同样的方法修复损伤的内侧副韧带[16]。 一直以来对于“恐怖三联征”中肘关节内侧副韧带损伤的处理存在着争议,有学者认为在治疗后残存不稳定的患者可给予修复内侧副韧带,也有学者认为修补内侧韧带结构是手术程序中的重要环节一,仲飙等[17]认为术前应通过MRI检查予充分评估肘关节内侧软组织损伤情况,对于前束轻度撕裂而完整性存在者无需处理,但对于严重的起、止点撕脱或体部断裂者,应常规采用内侧入路探查修补。外侧副韧带是维持肘关节稳定性的重要结构之一,可能是肘关节脱位时是第一个被破坏的结构[1],因此我们应对所有的外侧副韧带给予积极有效的修复治疗,同时也应重视内侧副韧带的损伤情况,做出恰当的处理。
随着人们对肘关节“恐怖三联征”认识的加深及内固定技术的发展,铰链式外固定架的运用相对减少,但有限内固定结合铰链支架治疗肘关节“恐怖三联征”既能保持肘关节的稳定性,又能早期进行功能锻炼,减少并发症的发生[18]。
总之, 肘关节“恐怖三联征”通过积极有效的手术治疗,大多数患者能够得到满意的结果。对于该类损伤,我们应尽可能通过有效的内固定重建骨及韧带的稳定结构,恢复肘关节的稳定性,及早配合正规的功能锻炼,最大程度恢复肘关节的功能。
[2] Butler DP, Alsousou J, Keys R. Isolated anterolateral fracture of the coronoid process of the ulna: a case report[J]. J Shoulder Elbow Surg, 2011, 20(2): e1-e4.
[3] Acevedo DC, Paxton ES, Kukelyansky I, et al. Radial head arthroplasty: state of the art[J]. J Am Acad Orthop Surg, 2014, 22(10): 633-642.
[4] Hotchkiss RN. Fractures and dislocations of the elbow//Rockwood CA Jr, Green DP, Bucholz RW, et al. Rockwood and Green′s Fractures in Adults[M].4th ed. Philadelphia, PA: Lippincott-Raven, 199:929-1024.
[5] Pugh DM, Wild LM, Schemitsch EH, et al. Standard surgical protocol to treat elbow dislocations with radial head and coronoid fractures[J]. J Bone Joint Surg Am, 2004, 86-A(6): 1122-1130.
[6] Zeiders GJ, Patel MK. Management of unstable elbows following complex fracture-dislocations—the terrible triad′ injury[J]. J Bone Joint Surg Am, 2008,90(Suppl 4):75-84.
[7] 林国叶,刘航涛,黄玉栋,等.肘关节后方+尺骨鹰嘴截骨入路治疗肘关节恐怖三联症[J].中国伤残医学,2014,22(2):58-60.
[8] Manidakis N, Sperelakis I, Hackney R, et al. Fractures of the ulnar coronoid process[J]. Injury, 2012, 43(7): 989-998.
[9] Garrigues GE, Wray WH, Lindenhovius AL, et al. Fixation of the coronoid process in elbow fracture-dislocations[J]. J Bone Joint Surg Am, 2011, 93(20): 1873-1881.
[10] Jeon IH, Sanchez-Sotelo J, Zhao K, et al. The contribution of the coronoid and radial head to the stability of the elbow[J]. J Bone Joint Surg Br, 2012, 94(1): 86-92.
[11] Papatheodorou LK, Rubright JH, Heim KA,et al.Terrible triad injuries of the elbow: does the coronoid always need to be fixed? [J].Clin Orthop Relat Res,2014 ,472(7):2084-2091.
[12] Alolabi B, Gray A, Ferreira LM, et al. Reconstruction of the coronoid process using the tip of the ipsilateral olecranon[J]. J Bone Joint Surg Am, 2014, 96(7): 590-596.
[13] Bohn K, Ipaktchi K, Livermore M, et al. Current treatment concepts for"terrible triad. injuries of the elbow[J].Orthopedics, 2014, 37(12): 831-837.
[14] Watters TS, Garrigues GE, Ring D, et al. Fixation versus replacement of radial head in terrible triad: is there a difference in elbow stability and prognosis?[J]. Clin Orthop Relat Res, 2014, 472(7): 2128-2135.
[15] El Sallakh S. Radial head replacement for radial head fractures[J]. J Orthop Trauma, 2013, 27(6): e137-e140.
[16] 陈辉,郭庆山,刘华渝,等. 肘关节“恐怖三联征”的诊断和治疗[J].创伤外科杂志,2014,16(3):222-225.
[17] 仲飙,张弛,罗从风,等.肘关节“恐怖三联征”中内侧副韧带及合并损伤的治疗策略[J].中华骨科杂志,2013, 33(5):534-540.
[18] 温晓东,李玉茂,张玉九.有限内固定结合铰链式外固定架治疗肘关节[J].疑难病杂志,2013,(8):627-629.
(本文编辑:胡桂英)
孟亚轲,刘岩,叶添文,等.肘关节“恐怖三联征”的手术治疗:附14例报告[J/CD]. 中华肩肘外科电子杂志,2015,3(3):151-155.
Operative treatment of elbow joint "terrible triad":attached with report on 14 cases
MengYake,LiuYan,YeTianwen,OuyangYueping,ChenAimin,GuoYongfei.
DepartmentofOrthopaedics,theSecondMilitaryUniversityAffiliatedChangzhengHospital,Shanghai200003,China
GuoYongfei,Email:cz-gyf@163.com
Background Elbow joint "terrible triad" refers to posterior dislocation of elbow joint combined with ulna coracoid process fracture and radius head fracture, often accompanied with injuries of medial collateral ligament and/or lateral collateral ligament of elbow joint. Distal clavicular fracture combined with coracoclavicular ligament rupture frequently behave as unstable fracture, with the opportunity for fracture non-union in conservative therapy being as high as 21%. During the period from July 2010 to October 2013, our department performed operative treatment for 14 cases of elbow joint "terrible triad" with complete follow-up, and achieved satisfactory therapeutic effects. The specific process is hereby reported as follows.Method I. General materials:This group includes 14 cases (11 male cases and 3 female cases), aged 23-48 years, with an average age of 35.4 years; 5 cases in the left side, 9 cases in the right side, all suffer from closed injury. No one case suffers from related neurovascular injury. Injury causes: High falling accident 5 cases, traffic accident 3 cases, falling injury 4 cases and sport injury 2 cases. After hospital admission, according to the routine procedure, we performed elbow joint X-ray anterioposterior and lateral film, elbow joint CT scanning and three-dimensional reconstruction to judge the type of fracture and the fracture displacement condition. Ulna coronoid fracture Regan-Morrey typing , 10 cases of type Ⅲ, and 2 cases of type Ⅲ; According to Mason typing of radius head fracture, 7 cases of type Ⅲ, and 3 cases of type Ⅲ, of which 1 case is combined with ipsilateral distal radius fracture,And 1 case is combined with ipsilateral ulnar fracture; All the cases in this group are combined with injuries of medial collateral ligament and/or lateral collateral ligament of elbow joint.Ⅱ. Operative method:Allow the patient to lie flat on operating table, and place inflatable tourniquets on the proximal ends of affected limbs. Under brachial plexus block anesthesia, conventionally use elbow joint medial and lateral combined approaches, perform reduction of affected elbow joint, then in the sequence from the shallower to the deeper repair the ulna coracoid process fracture, the anterior joint capsule, the radius head fracture, the lateral collateral ligament and the starting point of common extensor tendon. The ulna coracoid process fracture is fixed by using mini-plate, lag screw, stitching anchor or rope stitching technique; radial head fracture is fixed by using kirschner wire, mini-screw and mini-plate; For all the cases, we use non-absorbable braided suture or anchor to repair their lateral collateral ligaments (LCL). Prior to incision closure, perform varus-valgus rotation test on straight position of elbow joint and cubitus valgus overload test to judge the recovery of elbow joint stability. In the process of passive flexion of elbow joint, 3 cases show poor concentric circle stability, for 2 cases of them, we use non-absorbable braided suture and anchor to repair their medial collateral ligaments (MCL); For 1 case, place lateral articulated type external fixation support, and keep elbow joint flexion 90°fixed hinge during operation; the other 12 cases can still maintain stability. After operation, 13 cases are provided with elbow joint flexion 90°and plaster fixation at neutral position of fore arms.Ⅲ. Functional exercise and follow-up:13 cases in plaster fixation perform finger movement as well as Biceps brachii muscle/Triceps brachii muscle isometric contraction training; At postoperative 48h, start passive elbow joint flexion and extension activity as well as fore arm rotation activity. At operative 1-2 week, 1 case assisted with external fixation started functional exercise; in the 1st week post operation, adjust the knob at the center of hinge support, instruct the affected elbows to perform flexion and extension function exercise; At post-operative 6th-8thweek, remove external fixation support. In the process of rehabilitation, avoid hyperextension of elbow joint. After operation, respectively in the follow-up on the 1stday, at the 2ndweek, 1stmonth, 3rdmonth, 6thmonth and 12thmonth, take X-ray anterioposterior and lateral film of affected elbow joints. Observe the healing condition of fracture fragments as well a s the occurrence of postoperative complications such as heterotopic ossification and Osteoarthritis; Investigate the improvements in elbow joint function, and instruct the patients to perform functional exercise. Upon completion of follow-up, perform evaluation of therapeutic effect according to Mayo elbow joint function scoring standard.Results 14 cases in this group obtained follow-up, with an average follow-up time of 18 months (10-37 months). The clinical fracture union time is postoperative 10-15 weeks, with an average time of 12.4 weeks. In postoperative 6 months, elbow joint flexion position (0°-20°), extension position (130°-145 °), with an average range of joint motion being 116.5°; pronation (60°-85°)supination (45°-75°), with an average rotation range of 126°. 1 case has stiff elbow joint; 2 cases show heterotopic ossification in imageological examination at the 6thmonth after operation, which, however do not affect the functions of elbow joint. Evaluation according to Mayo scoring standard: Excellent 6 case, good 4 cases, general 2 cases and poor 1 case.Conclusion Through active and effective operative treatment for elbow joint "terrible triad", most of the patients can obtain satisfactory results. For such type of injuries, we should make every effort to reconstruct stable structure of bone and ligament through effective internal fixation and recover the stability of elbow joint in combination with timely and normal functional exercise, so as to recover the functions of elbow joint to the maximum extent.
Elbow joint;Terrible triad;Fracture;Dislocation;Fixation
10.3877/cma.j.issn.2095-5790.2015.03.005
国家自然基金青年项目(31100988)
200003上海,第二军医大学附属长征医院骨科
郭永飞,Email:cz-gyf@163.com
2015-01-01)