外环下显微外科精索静脉结扎术对精索静脉曲张患者精液质量的影响
符红霞 梁培育 周治彦


【摘要】目的:探讨外环下显微外科精索静脉结扎术对精索静脉曲张患者精液质量的影响,并观察和分析其安全性。方法:选择本院2012年10月至2014年3月精索静脉曲张患者104例,根据手术方法分为对照组51例和观察组53例,对照组患者采用腹腔镜下精索静脉结扎术,观察组患者采用外环下显微外科精索静脉结扎术。记录两组患者手术时间、出血量、术后住院天数,检测治疗前后精液质量及畸形率,观察术后并发症及复发状况。结果:观察组出血量和住院时间分别为(24.58±4.93)mL和(5.13±1.24)d,均低于对照组,差异有统计学意义(P<0.05);观察组患者治疗后精子数量、精子活力和精子活动率分别为(43.76±7.22)×106/mL、(48.66±5.93)%和(55.28±7.50)%,均高于对照组治疗后(34.53±5.28)×106/mL、(37.83±6.36)%和(52.15±7.12)%,差异具有统计学意义(P<0.05)。观察组患者治疗后精子畸形率为(12.42±3.86)%,低于对照组治疗后(16.21±5.08)%,差异具有统计学意义(P<0.05)。观察组患者不良反应及复发总计4例(7.55%),低于对照组10例(19.61%),差异具有统计学意义(P<0.05)。结论:外环下显微镜精索静脉结扎术创伤小、恢复较快,能够显著提高患者精子数量和质量,术中可有效保护睾丸动脉及淋巴管,减少术后并发症及复发率。
【关键词】显微外科;精索静脉结扎术;精索静脉曲张;精液质量
Impact on semen quality of varicocele patients with spermatic vein ligation under the outer ring microsurgeryFU Hongxia, LIANG Peiyu, ZHOU Zhiyan. Department of Urology,The Hospital Affiliated to Hainan Medical University, Haikou 570102, Hainan, China
【Abstract】Objectives: To explore the impact on semen quality of varicocele patients with spermatic vein ligation under the outer ring microsurgery, and to observe and analyze its security. Methods: 104 varicocele patients were selected in the hospital from October in 2012 to March in 2014 and according to the operation method, were divided into the control group (51 cases) and the observation group (53 cases). The control group was treated by laparoscopic ligation of spermatic vein, while the observation group was treated by microsurgery under the outer ring ligation of spermatic vein. The operation time, blood loss, postoperative hospitalization time of two groups was recorded; the semen quality and malformation rate before and after the treatment was detected; the postoperative complications and recurrence was observed. Results: The blood loss and hospitalization time of the observation group respectively were (24.58±4.93) ml and (5.13±1.24) d, lower than the control group, with statistically significant difference (P<0.05). The sperm amount, sperm motility and sperm activity respectively of the observation group after treatment were (43.76±7.22)×106/ml, (48.66±5.93) % and (55.28±7.50) %, higher than the control group (34.53±5.28)×106/ml, (37.83±6.36) % and (52.15±7.12) %, with statistically significant difference (P<0.05). The sperm malformation rate of the observation group after treatment was (12.42±3.86) %, lower than the control group (16.21±5.08) %, with statistically significant difference (P<0.05). The total adverse reaction and recurrence in the observation group were 4 cases and 7.55%, lower than the control group (10 cases, 19.61%), with statistically significant difference (P<0.05). Conclusions: For outer ring ligation of spermatic vein under the microscope, it causes little injury and pain with rapid recovery, which can also significantly improve the sperm count and quality. During the operation it can effectively protect the testicular artery and lymphatic vessels, while reduce the postoperative complications and the recurrence rate.
【Key words】Microsurgery; Spermatic vein ligation; Varicocele; Semen quality
【中图分类号】R697+.24【文献标志码】A
精索静脉曲张是精索静脉因多种原因回流受阻、不畅,精索蔓状静脉丛扩张、迂曲、伸长,在阴囊里形成蚯蚓形状的团块,易引起患者睾丸的功能进行性衰退。主要表现为疼痛、阴囊坠胀不适、精液异常、男性不育等。临床治疗以精索静脉结扎手术为主,以有效阻止血液的返流[1,2]。近年来,显微镜外科精索静脉结扎术逐渐得到广泛应用,已成为治疗VC的主要术式。本研究旨在探讨外环下显微外科精索静脉结扎术对精索静脉曲张患者精液质量的影响,并观察和分析其安全性。
1资料与方法
1.1一般资料
随机选择本院2012年10月至2014年3月精索静脉曲张患者104例,纳入病例:均进行阴囊彩超显示精索静脉曲张并伴反流、Valsalva 实验阳性。排除病例:继发性精索静脉曲张患者。入选患者年龄24~49岁,平均(31.75±7.80)岁,根据手术方法分为对照组51例和观察组53例,对照组患者采用腹腔镜下精索静脉结扎术;观察组患者采用外环下显微外科精索静脉结扎术。两组患者年龄、病变部位、程度和病程比较,差异无统计学意义(P>0.05),具有可比性。见表1。
1.2方法和指标
1.2.1治疗方法观察组患者采用外环下显微外科精索静脉结扎术,在股沟外环下阴囊外上方作长约2~3cm 的斜形切口,逐层切开,露出精索、提起后牵出,将睾丸提出切口外,切断结扎扩张的睾丸引带静脉,显微镜下分离精索内外静脉、提睾肌静脉,双重结扎后切断,术中保护睾丸动脉、淋巴管及相关神经。还纳精索,逐层关闭切口。如为双侧病变,采取同样的术式进行处理。对照组患者采用腹腔镜(Olympus 腹腔镜系统)下精索静脉结扎术,距离内环口2~3cm处精索血管外侧,切开后腹膜,游离整束精索血管,分离精索内动、静脉,双重丝线结扎精索静脉并离断[3,4]。本研究经医院伦理委员会批准,患者及家属的同意签署知情同意书。
1.2.2主要指标记录两组患者手术时间、出血量、术后住院天数,术后并发症及6个月后复发状况,检测手术前后精液质量,包括精子密度、精子活力、巴氏染色计数精子畸形率。
1.3统计学处理
用SPSS11.0统计软件。计量资料采用均数±标准差(±s)表示,采用t检验,计数资料比较用χ2检验,P<0.05时差异有统计学意义。2结果
2.1两组患者手术状况结果比较
观察组出血量和住院时间分别为(24.58±4.93)mL和(5.13±1.24)d,均低于对照组,差异有统计学意义(P<0.05),两组手术时间比较,差异无统计学意义(P>0.05)。见表2。
2.2两组患者治疗前后精液质量结果比较
观察组患者治疗后精子数量、精子活力和精子活动率分别为(43.76±7.22)×106/mL、(48.66±5.93)%和(55.28±7.50)%,均高于对照组治疗后,两组治疗后均高于治疗前,差异具有统计学意义(P<0.05)。观察组患者治疗后精子畸形率为(12.42±3.86)%,低于对照组治疗后,两组治疗后均低于治疗前,差异具有统计学意义(P<0.05)。见表3。
2.3两组患者不良反应及复发情况比较
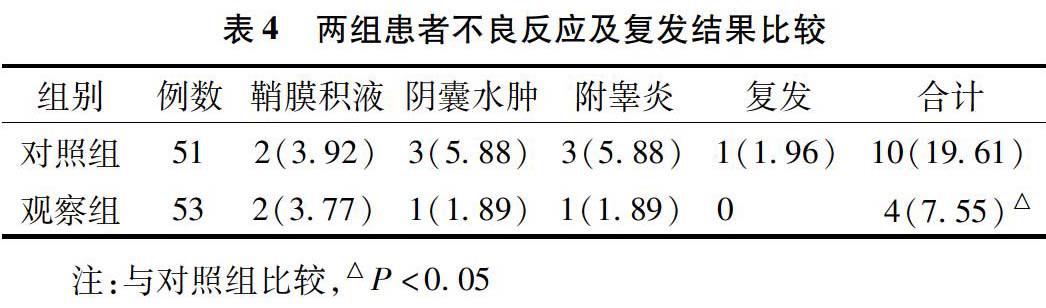
观察组患者不良反应及复发总计4例(7.55%),低于对照组,差异具有统计学意义(P<0.05)。见表4。
3讨论
精索静脉曲张是临床常见的一种男性疾病,也是引起不育的常见原因之一,多发生于青壮年。随着显微外科技术的发展,外环下显微外科精索静脉结扎术逐渐在临床上应用,逐渐成为较为理想的治疗方式[5-7]。
本次研究结果显示,观察组出血量和住院时间均低于对照组,差异有统计学意义(P<0.05),提示外环下显微外科精索静脉结扎术创伤小、恢复较快。外环下显微外科精索静脉结扎术麻醉简单、术中损伤小,有利于患者的康复。研究结果显示,观察组患者治疗后精子数量、精子活力和精子活动率均高于对照组,观察组患者治疗后精子畸形率低于对照组,差异具有统计学意义(P<0.05)。提示外环下显微外科精索静脉结扎术可显著提高患者精子数量和质量。精索内静脉、精索动脉和输精管分化成细小分支包绕睾丸动脉,参与构成精索,精索静脉血流淤滞能够影响睾丸的生精功能。显微镜手术的要点为结扎所有的精索静脉、提睾肌,可以有效阻止静脉反流,使患者的睾丸生长及功能获得恢复,精子产生过程趋于正常,精子数量和质量得以改善[8-10]。睾丸动脉对精液质量的改善起着重要的作用,显微镜下能够准确辨认睾丸动脉,有利于睾丸生精功能的恢复及精液质量及精子活力的提高[11-13]。
本次研究结果显示,观察组患者不良反应及复发率低于对照组,差异具有统计学意义(P<0.05)。提示外环下显微镜精索静脉结扎术可减少术后并发症及复发率。腹腔镜术手术时间较短,但对精索内静脉进行结扎难以对可能存在曲张情况的输精管和提睾肌静脉进行处理,易导致术后复发。在显微镜下能够准确辨认睾丸动脉、精索淋巴管,细致操作可充分保留精索淋巴管及睾丸动脉,能够有效降低术后因动脉损伤引起的睾丸萎缩,因结扎淋巴管引起阴囊水肿的风险,对精索静脉彻底结扎及显微镜下还可发现细小静脉分支并结扎以避免持续静脉曲张[14]。外环下显微镜精索静脉结扎术需要一定的熟练程度,尤其是显微镜下的操作技巧。本研究尚需进一步观察患者生育状况。
综上所述,外环下显微镜精索静脉结扎术创伤小、恢复较快,能够显著提高患者精子数量和质量,术中可有效保护睾丸动脉及淋巴管,减少术后并发症及复发率。
参考文献
[1]胡克清,战立龙,王静,等.外环下显微镜外科治疗精索静脉曲张的临床研究(附26例报告).泌尿外科杂志(电子版),2015,7(2):50-52.
[2]Guevara CJ,El-Hilal AH,Darcy MD.Percutaneous antegrade varicocele embolization via the testicular vein in a patient with recurrent baricocele after surgical repair.Cardiovascular and Interventional Radiology,2015,38 (5):1325-1329.
[3]卢永强,秦茂,张秀平,等.外环下显微外科精索静脉结扎术联合五子衍宗丸治疗精索静脉曲张不育症临床观察.中国性科学,2015,24(8):71-74.
[4]刘洁,石红林,陈国晓,等.腹腔镜 2 种术式治疗精索静脉曲张疗效观察.中华实用诊断与治疗杂志,2014,28(1):69-70.
[5]贾月峰,杨晓坤,王沛涛,等.手术治疗对精索静脉曲张性重度少精或无精患者的效果.中国医药导报,2014,11(32):55-59.
[6]尉媛,常征,徐凌忠.3种手术方法对精索静脉曲张疗效的比较.解放军预防医学杂志,2015,33(4):415-416.
[7]蔡伟飞,毛向明.腹膜后与腹股沟管切口显微镜下精索静脉结扎治疗精索静脉曲张的对比研究.现代诊断与治疗,2015,26(5):1131-1132.
[8]Guzel O,Aslan Y,Balci M,et al.Significant worsening sperm parameters are associated to testicular hypotrophy in patients with a high grade varicocele. Actas Urológicas Espaolas (English Edition),2015,39(6):392-395.
[9]来晓东,邵靖雯,郭刚,等.高选择性腹腔镜精索内静脉结扎术治疗精索静脉曲张的疗效研究.微创泌尿外科杂志,2015,4(3):140-142.
[10]苏晓程,王建,叶纯.外环下精索静脉显微解剖结扎术治疗精索静脉曲张的有效性研究.中国性科学,2015,24(7):17-20.
[11]Eid AA , Younan DN.Seminal Tumour necrosis factor-related apoptosis-inducing ligand and its relationship to infertility in Egyptian patients with varicocele. Andrologia,2015,47(9):1028-1033.
[12]Chen SS. Varicocele is associated with varicose veins: A population-based case-control study.International Journal of Urology,2015,22 (10 ):976-977.
[13]Tauber R, Schmolling K, Ulm K.Antegrade scrotal sclerosis therapy. Gold Standard of varicocele treatment.Der Urologe. Ausg. A,2015,54 (8):1121-1122.
[14]DAndrea S, Giordano AV, Carducci S,et al. Embolization of left spermatic vein in non-obstructive azoospermic men with varicocele: role of FSH to predict the appearance of ejaculated spermatozoa after treatment. Journal of Endocrinological Investigation,2015,38(7):785-790.

