高脂血症性与胆源性急性胰腺炎患者血脂、血淀粉酶、尿淀粉酶水平的比较
董永春
成都军区机关医院消化科,四川 成都 610011
高脂血症性与胆源性急性胰腺炎患者血脂、血淀粉酶、尿淀粉酶水平的比较
董永春
成都军区机关医院消化科,四川 成都 610011
目的 比较高脂血症性急性胰腺炎(hyperlipidemic acute pancreatitis, HLAP)与胆源性急性胰腺炎(biliary acute pancreatitis, BAP)患者的血脂、血淀粉酶(amylase, AMY)和尿淀粉酶(urine amylase, UAMY)含量水平。方法 选取2014年8月-2016年8月在成都军区机关医院就诊的急性胰腺炎(acute pancreatitis, AP)患者218例,其中HLAP患者117例,BAP患者101例,分析两组患者血脂、AMY、UAMY、血葡萄糖(Glu)、乳酸脱氢酶(LDH)、血红细胞压积(HCT)、C反应蛋白(CRP)、治疗及预后的情况。结果 HLAP组的甘油三酯(TG)、总胆固醇(TC)、高密度脂蛋白(HDL-C)、低密度脂蛋白(LDH-C)、平均载脂蛋白A(Apo-A)和平均载脂蛋白B(Apo-B)含量水平均高于BAP组,两组之间比较,差异有统计学意义(P<0.05)。HLAP组的AMY、UAMY和LDH含量水平低于BAP组,HLAP组的Glu、HCT和CRP含量水平高于BAP组,两组之间比较,差异有显著统计学意义(P<0.01)。HLAP组的复发、手术治疗和病死例数高于BAP组,两组之间比较,差异有统计学意义(P<0.05)。结论 HLAP患者的糖脂质含量水平高于BAP患者,AMY和UAMY含量水平低于BAP患者。
高脂血症性急性胰腺炎;胆源性急性胰腺炎;血淀粉酶;尿淀粉酶
急性胰腺炎(acute pancreatitis, AP)临床上属于常见病,发生该疾病的原因有酒精、高脂血症、饮食、内分泌、腹部创伤、遗传等,在我国比较多见的发病原因是胆道疾病[1]。发生胆源性急性胰腺炎(biliary acute pancreatitis, BAP)概率最高,超过1/2的AP是因为胆道疾病如胆结石、胆道蛔虫等引起的,发生AP的时候发展较快且急,有时候病情非常危险,病死率为6%~12%[2]。经常发作AP的患者大多数并发高脂血症,特别是升高非常明显的甘油三脂(TG),当血清浓度>11.3 mmol/L时发生AP的概率非常高,多年的研究证明高脂血症是发生AP的主要原因之一,称为高脂血症性急性胰腺炎(hyperlipidemic acute pancreatitis, HLAP)[3-4]。然而,脂质、血淀粉酶(amylase, AMY)和尿淀粉酶(urine amylase, UAMY)在HLAP与BAP患者的含量水平并不清楚。因此,本文主要对HLAP与BAP患者的糖脂质、AMY和UAMY含量水平进行比较,为临床治疗提供参考。
1 资料与方法
1.1 一般资料 选取2014年8月-2016年8月在成都军区机关医院就诊的AP患者218例,其中HLAP患者117例,男76例,女41例,年龄(40.91±9.54)岁;BAP患者101例,男45例,女56例,年龄(46.17±14.38)岁;男女比例、年龄在两组间比较,差异无统计学意义(P>0.05),具有可比性。
1.2 纳入及排除标准 纳入标准:参照2014版急性胰腺炎诊治指南进行诊断,HLAP诊断标准:具有AP的临床和影像学表现,入院时血TG>11.3 mmol/L或AP并静脉乳糜状血患者;BAP诊断标准:符合AP的临床诊断指标,根据B超、CT、MRCP或ERCP等影像学检查提示胆管、胆囊结石等疾病。排除标准:发病48 h内入院后未进行血脂检测,伴有结石、蛔虫等胆系疾病的HLAP患者。
1.3 研究方法 采集患者早晨空腹血液,提取血清进行检测。所有患者入院后均按照我国急性胰腺炎诊治指南进行规范化治疗,非手术治疗:包括禁食、胃肠减压、解痉、止痛、抑酸和胰酶抑制、液体复苏、保护器官功能、营养支持、抗炎等治疗;手术治疗:外科治疗主要针对胰腺局部并发症继发感染或产生压迫症状,如消化道梗阻、胆道梗阻、胰瘘等。
1.4 研究指标 分析两组患者血脂、AMY、UAMY、血葡萄糖(Glu)、乳酸脱氢酶(LDH)、血红细胞压积(HCT)、C反应蛋白(CRP)、治疗及预后的情况。
1.5 质量控制 所有患者样品均重复检测3次,取平均值。

2 结果
2.1 两组患者的血脂水平比较 结果显示,HLAP组中的TG、TC、Apo-B含量显著高于BAP组,差异有统计学意义(P<0.01)。HLAP组中的HDL-C、LDH-C、Apo-A含量高于BAP组,两组之间比较,差异有统计学意义(P<0.05,见表1)。


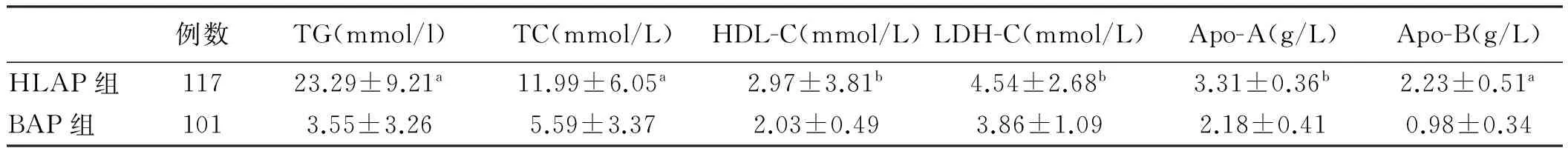
例数TG(mmol/l)TC(mmol/L)HDL-C(mmol/L)LDH-C(mmol/L)Apo-A(g/L)Apo-B(g/L)HLAP组11723.29±9.21a11.99±6.05a2.97±3.81b4.54±2.68b3.31±0.36b2.23±0.51aBAP组1013.55±3.265.59±3.372.03±0.493.86±1.092.18±0.410.98±0.34
注:与BAP组比较,aP<0.01,bP<0.05。
2.2 两组患者的生化指标比较 结果显示,HLAP组中的AMY、UAMY、LDH含量显著低于BAP组,差异有统计学意义(P<0.01);HLAP组中的Glu、HCT、CRP含量显著高于BAP组,两组之间比较,差异有显著统计学意义(P<0.01,见表2)。


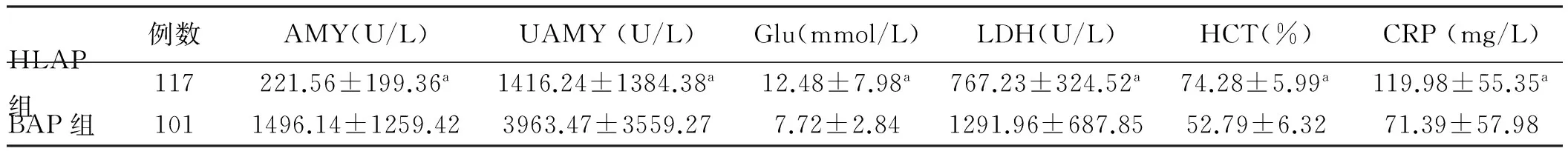
例数AMY(U/L)UAMY(U/L)Glu(mmol/L)LDH(U/L)HCT(%)CRP(mg/L)HLAP组117221.56±199.36a1416.24±1384.38a12.48±7.98a767.23±324.52a74.28±5.99a119.98±55.35aBAP组1011496.14±1259.423963.47±3559.277.72±2.841291.96±687.8552.79±6.3271.39±57.98
注:与BAP组比较,aP<0.01。
2.3 两组患者的治疗及预后分析 两组患者入院后均给予非手术治疗,经非手术治疗无效或病情急剧进展、胰腺局部并发症继发感染或产生压迫症状时,及时给予外科手术干预治疗。通过对两组患者的治疗及预后比较分析,结果显示,HLAP组的复发病例数高于BAP组,HLAP组的手术治疗例数高于BAP组,HLAP组的病死例数高于BAP组,两组之间比较,差异有统计学意义(P<0.05,见表3)。
表3 两组患者的治疗及预后比较[例数(%)]
Tab 3 Comparison of treatment and prognosis between two groups [n(%)]
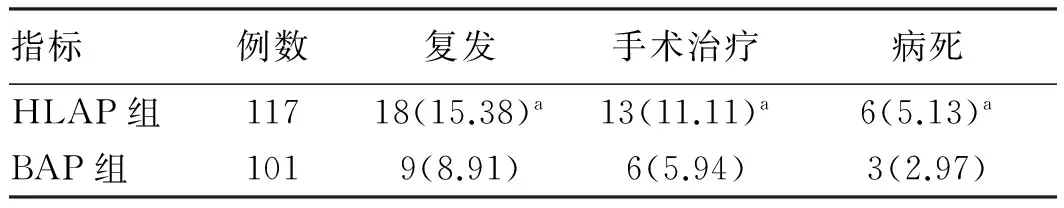
指标例数复发手术治疗病死HLAP组11718(15.38)a13(11.11)a6(5.13)aBAP组1019(8.91)6(5.94)3(2.97)
注:与BAP组比较,aP<0.05。
3 讨论
随着对HLAP患者的研究,我国学者提出关于此疾病的规范治疗标准,拟定提出了关于AP的治疗标准,还对AP的分类进行修改,详细概述了局部及全身性的AP并发症,及评估疾病严重程度的指标,包括对治疗诊断等方面的标准,第一次确定血脂对AP的影响(TG血液含量>11.3 mmol/L发生AP概率增加,降低血脂到<5.65 mmol/L可以降低风险)及逐年上升的发病趋势[5-7]。AP患者中并发高脂血症的占8.9%,目前认为影响的原因可以归为3种:(1)直接产生的损伤,通常情况下存在胰腺内或四周的TG会被胰脂肪酶水解成游离的脂肪酸,这时会有白蛋白结合这些游离的脂肪酸,但是当游离脂肪酸量超过能够结合的白蛋白量时过多的游离脂肪酸就会损伤胰腺泡细胞还有血管内皮细胞;(2)血液循环障碍,TG含量过高会抑制纤溶酶原、AMY、UAMY及Ⅶ因子活性,并且血清中血脂过高容易出现血栓堵在微血管,导致胰腺中的血液循环异常,组织得不到充足的血液供应出现坏死;(3)胰蛋白酶原被激活,当患者发生AP时,游离脂肪酸增多会刺激机体产生更多的蛋白酶原,这样会加重对胰腺泡细胞的损伤[8-9]。对于HLAP出现的临床特征还在进一步的研究,多数学者认为HLAP患者会出现明显升高的TG水平,并且血液出现脂浊样,没有明显升高AMY或UAMY,不断地反复发作,并发脂肪肝、糖尿病等[10]。Göçmen等[11]研究认为HLAP会导致更多的并发症及加重病情。Xu等[12]研究认为TG血症不会直接影响AP的严重程度及引发并发症。
一旦身体中有组织被损伤或炎症反应时,单核细胞和免疫细胞会被刺激活化释放出能够让肝脏上皮细胞释放急性应激炎症蛋白的因子,这种应急炎症反应蛋白叫作CRP,属于组织损伤炎症反应的标志物[13]。很多临床试验证明,整个AP过程中CRP起关键作用,在血液中的含量直接关系到AP的病情还有发生并发症的概率[14]。经过不断地分析AP患者发病原因数据,现在可以将诊断AP的病情程度量化为CRP>150 mg/L这一阈值进行判断[15-17]。内科治疗HLAP当下主要为保守治疗,除了常规的治疗之外还考虑到血脂对病情的影响所以配合降血脂药物进行治疗[18]。Kruszyna等[19]研究认为治疗过程中做到净化血液,静脉注射胰岛素、低分子量肝素等是比较关键的治疗措施,其中最核心的就是降低血液中TG的含量。
本研究结果显示HLAP组的TG、TC、HDL-C、LDH-C、Apo-A和Apo-B含量水平高于BAP组,两组之间比较,差异有统计学意义。HLAP组的AMY、UAMY和LDH含量水平低于BAP组,HLAP组的Glu、HCT和CRP含量水平高于BAP组,两组之间比较,差异有显著统计学意义。HLAP组的复发、手术治疗和病死例数高于BAP组,两组之间比较,差异有统计学意义。这表明HLAP患者中,血清中TG水平增加的更多,它能显著干扰AMY活性的检测,同时该抑制因子还可以通过肾脏进入尿液,抑制UAMY活性从而使其检测值下降。此外,AMY和UAMY不升高,伴有糖尿病、脂肪肝等伴随疾病,容易合并局部或全身并发症,从而增加产生复发、手术治疗和病死的概率。
综上所述,HLAP患者的糖脂质含量水平高于BAP患者,AMY和UAMY含量水平低于BAP患者。
[1]Kusnierz K, Nowakowska-Dulawa E, Pilch-Kowalczyk J, et al. Biliary cast syndrome in a non-transplant patient with acute pancreatitis [J]. Dig Liver Dis, 2012, 44(6): 534-535.
[2]Dubravcsik Z, Hritz I, Fejes R, et al. Early ERCP and biliary sphincterotomy with or without small-caliber pancreatic stent insertion in patients with acute biliary pancreatitis: better overall outcome with adequate pancreatic drainage [J]. Scand J Gastroenterol, 2012, 47(6): 729-736.
[3]Saraswat VA, Sharma BC, Agarwal DK, et al. Biliary microlithiasis in patients with idiopathic acute pancreatitis and unexplained biliary pain: response to therapy [J]. J Gastroenterol Hepatol, 2014, 23(1): 1910-1918.
[4]Kruszyna T, Zajac A, Karcz D. Sphincter of Oddi manometry in patients with acute biliary pancreatitis: evidence for sphincter of Oddi dysfunction in acute biliary pancreatitis [J]. Scand J Gastroenterol, 2004, 39(7): 696-697.
[5]Billi P, Barakat B, D’Imperio N, et al. Relapses of biliary acute pancreatitis in patients with previous attack of biliary pancreatitis and gallbladder in situ [J]. Dig Liver Dis, 2003, 35(9): 653-655.
[6]de Madaria E. Pancreas and biliary tract. Which is the right moment for cholecystectomy in a patient with previous acute pancreatitis of biliary origin complicated by intraabdominal collections [J]. Gastroenterol Hepatol, 2008, 31(7): 464-465.
[7]张铁英, 马彬. 高脂血症急性胰腺炎患者C反应蛋白水平及影响因素研究[J]. 宁夏医学杂志, 2016, 38(5): 428-430. Zhang TY, Ma B. The study of CRP and related risk factor in acute pancreatitis patients with hyperlipidemia [J]. Ningxia Med J, 2016, 38(5): 428-430.
[8]Noel RA, Braun DK, Patterson RE, et al. Increased risk of acute pancreatitis and biliary disease observed in patients with type 2 diabetes: a retrospective cohort study [J]. Diabetes Care, 2009, 32(5): 834-838.
[9]Nebiker CA, Frey DM, Hamel CT, et al. Early versus delayed cholecystectomy in patients with biliary acute pancreatitis [J]. Surgery, 2009, 145(3): 260-264.
[10]Martínez JF. Pancreas and biliary tree. In patients with acute pancreatitis, what monitoring measures and treatment are essential in the first 72 h after onset? [J]. Gastroenterol Hepatol, 2008, 31(9): 616-617.
[11]Göçmen E, Klc YA, YoldaO, et al. Comparison and validation of scoring systems in a cohort of patients treated for biliary acute pancreatitis [J]. Pancreas, 2007, 34(1): 66-69.
[12]Xu HM, Qiu YF, Wang WM. Diagnoses and treatment of 125 patients with biliary acute pancreatitis [J]. Zhong Xi Yi Jie He Xue Bao, 2006, 4(5): 537-538.
[13]Saraswat VA, Sharma BC, Agarwal DK, et al. Biliary microlithiasis in patients with idiopathic acute pancreatitis and unexplained biliary pain: response to therapy [J]. J Gastroenterol Hepatol, 2004, 19(10): 1206-1211.
[14]陈微微. 高脂血症性急性胰腺炎患者的临床特征(28例)[J]. 医疗装备, 2016, 29(15): 13-14. Chen WW. Clinical characteristics of 28 cases with hyperlipidemic acute pancreatitis [J]. Medical Equipment, 2016, 29(15): 13-14.
[15]Dubravcsik Z, Hritz I, Fejes R, et al. Early ERCP and biliary sphincterotomy with or without small-caliber pancreatic stent insertion in patients with acute biliary pancreatitis: better overall outcome with adequate pancreatic drainage [J]. Scand J Gastroenterol, 2012, 47(6): 729-736.
[16]Pezzilli R, Billi P, Barakat B, et al. Ultrasonographic evaluation of the common bile duct in biliary acute pancreatitis patients: comparison with endoscopic retrograde cholangiopancreatography [J]. J Ultrasound Med, 1999, 18(6): 391-394.
[17]Mistiri S, Hadjsalah H, Achour H. Letter: acute pancreatitis in patients with biliary microlithiasis [J]. Nouv Presse Med, 1976, 5(14): 930.
[18]Guo L, Zheng T, Hu G, et al. Continuous renal replacement therapy in successful treatment of a patient with hyperlipidemic acute pancreatitis [J]. Ther Apher Dial, 2015, 19(5): 518-521.
[19]Kruszyna T, Zajac A, Karcz D. Sphincter of oddi manometry in patients with acute biliary pancreatitis: evidence for sphincter of oddi dysfunction in acute biliary pancreatitis [J]. Scand J Gastroenterol, 2004, 39(7): 696-697.
(责任编辑:马 军)
Comparison of glycolipid, amylase and urine amylase levels in patients with hyperlipidemia and biliary acute pancreatitis
DONG Yongchun
Department of Gastroenterology, the Institution Hospital of Chengdu Military Command, Chengdu 610011, China
Objective To compare the levels of glycolipid, amylase (AMY) and urine amylase (UAMY) in hyperlipidemic acute pancreatitis (HLAP) and biliary acute pancreatitis (BAP) patients. Methods Two hundred and eighteen cases of acute pancreatitis (AP) patients were selected in the Institution Hospital of Chengdu Military Command from Aug. 2014 to Aug. 2016, and divided into HLAP group (n=117) and BAP group (n=101). The blood lipid, serum amylase (AMY), urine amylase (UAMY), blood glucose (Glu), lactate dehydrogenase (LDH), blood hematocrit (HCT), C reactive protein (CRP) of patients with treatment and prognosis between two groups were analyzed. Results
The levels of TG, TC, HDL-C, LDH-C, Apo-A and Apo-B in the HLAP group were higher than those in BAP group, and there was statistical difference between two groups (P<0.05). The levels of AMY, UAMY and LDH in the HLAP group were lower than those in BAP group, the levels of Glu, HCT and CRP in the HLAP group were higher than those in BAP group, and there was significant difference between two groups (P<0.01). Recurrence, surgical treatment and death cases of HLAP group were higher than those in BAP group, there was statistical difference between two groups (P<0.05). Conclusion The level of serum lipid in HLAP patients is higher than the patients with BAP, the levels of AMY and UAMY in HLAP patients are lower than the patients with BAP.
Hyperlipidemic acute pancreatitis; Biliary acute pancreatitis; Serum amylase; Urine amylase
10.3969/j.issn.1006-5709.2017.07.012
R576
A
1006-5709(2017)07-0761-04
2017-06-05

