单孔胸腔镜手术在结核性脓胸治疗中的应用
邓高焱 王永利 范明 何超 王勋 吴郁美 石自力
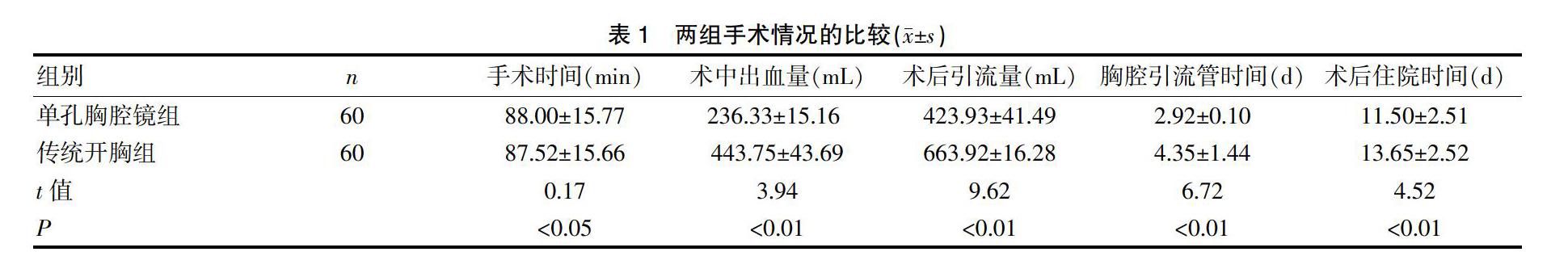
[摘要] 目的 探讨单孔胸腔镜手术治疗结核性脓胸的应用价值,并总结相关临床经验。 方法 回顾性分析我院胸外科2015年1月~2017年12月住院手术治疗的120例结核性脓胸患者。依据纳入、排除的相关标准,在知情同意下将纳入患者随机分为研究组(单孔胸腔镜手术组,60例)和对照组(传统开胸手术组,60例),比较两组患者的手术时间、术中出血量、术后引流量、胸腔引流管时间、术后住院时间及术后并发症。 结果 两组患者围术期均无死亡病例,中转开胸3例,中转开胸率为5%(3/60)。单孔胸腔镜组与传统开胸组相比较,手术时间分别为(88.00±15.77)min、(87.52±15.66)min,术中出血量分别为(236.33±15.16)mL、(443.75±43.69)mL,术后引流量分别为(423.93±41.49)mL、(663.92±16.28)mL,胸腔引流管时间分别为(2.92±0.10)d、(4.35±1.44)d,术后住院时间分别为(11.50±2.51)d、(13.65±2.52)d,两组患者的术中出血量、术后引流量、胸腔引流管时间及术后住院时间相比,差异均有统计学意义(P均<0.05)。比较两组的手术时间,差异无統计学意义(P>0.05)。单孔胸腔镜组术后并发症的总的发生率为6.67%(4/60),传统开胸组术后并发症的总发生率为13.33%(8/60)。 结论 单孔胸腔镜手术治疗结核性脓胸创伤小、并发症少、住院时间短,患者恢复快,在临床应用中值得推广。但在临床实际中应根据患者病情合理选择手术方式。
[关键词] 单孔胸腔镜;脓胸;结核性;手术
[中图分类号] R521.7 [文献标识码] B [文章编号] 1673-9701(2020)04-0050-04
Application of single-port thoracoscopic surgery in the treatment of tuberculous empyema
DENG Gaoyan WANG Yongli FAN Ming HE Chao WANG Xun WU Yumei SHI Zili
Department of Thoracic Surgery, Hunan Chest Hospital, Changsha 410013, China
[Abstract] Objective To investigate the application value of single-port thoracoscopic surgery for tuberculous empyema and to summarize relevant clinical experience. Methods 120 patients with tuberculous empyema who underwent surgical treatment from January 2015 to December 2017 in the Department of Thoracic Surgery of Hospital were retrospectively analyzed. According to the relevant criteria of inclusion and exclusion, the patients were randomLy divided into the study group (single-port thoracoscopic surgery group, 60 cases) and the control group (traditional thoracotomy group, 60 cases) with informed consent. Surgical time, intraoperative blood loss, postoperative drainage, chest drainage time, postoperative hospital stay, and postoperative complications between two groups were compared. Results There were no deaths in the perioperative period, and 3 cases were converted to thoracotomy. The conversion rate of thoracotomy was 5%(3/60). In the single-port thoracoscopic surgery group and the traditional thoracotomy group, the operation time was (88.00±15.77) min and (87.52±15.66) min, respectively; the intraoperative blood loss was (236.33±15.16) mL and (443.75±43.69) mL, respectively; the post-drainage was (423.93±41.49) mL and (663.92±16.28) mL, respectively; the chest drainage time was(2.92±0.10)d,(4.35±1.44) d, respectively; the postoperative hospital stay was (11.50±2.51)d, (13.65±2.52)d. There were significant differences in the intraoperative blood loss, postoperative drainage, chest drainage time and postoperative hospital stay(P<0.05). There was no significant difference in the operation time between the two groups(P>0.05). The overall incidence of postoperative complications in the single-port thoracoscopic surgery group was 6.67%(4/60), and the overall incidence of postoperative complications in the traditional thoracotomy group was 13.33%(8/60). Conclusion Single-port thoracoscopic surgery in the treatment of tuberculous empyema has less trauma, fewer complications, shorter hospital stay, and faster recovery. It is worthy of promotion in clinical application. However, in clinical practice, the surgical method should be reasonably selected according to the patient's condition.
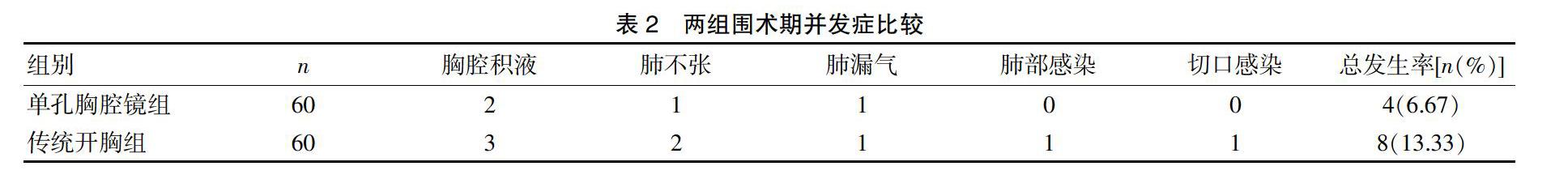
2.2 两组围术期并发症比较
围术期并发症主要包括胸腔积液、肺不张、肺漏气、肺部感染、切口感染,单孔胸腔镜组围术期出现胸腔积液2例,肺不张1例,肺漏气1例,无肺部感染及切口感染病例,总的并发症发生率为6.67%(4/60)。传统开胸组围术期出现胸腔积液3例,肺不张2例,肺漏气1例,肺部感染1例,切口感染1例,总的并发症发生率为13.33%(8/60)。见表2。
3 讨论
结核病严重影响人类的健康,目前我国的结核疫情形式严峻,世界卫生组织(World Health Organization,WHO)把印度、中国、俄罗斯、南非等22个国家列为结核病高负担、高危险性国家,中国居世界第二位[4]。目前结核治疗方案包括药物、手术、免疫、营养等多种手段的综合治疗[5]。对结核病及时、正确的诊断、治疗,不仅有利于患者康复,而且对消除传染源、控制结核疫情至关重要。
空洞型肺结核,早期胸膜炎未及时或规范治疗,耐药结核菌,胸壁、脊柱旁结核脓肿破溃或直接蔓延等多种因素是结核性脓胸形成原因,结核性脓胸的病理过程包括渗出期、纤维素期及机化期[6]。美国胸科协会(AST)将结核性脓胸分为渗出期脓胸(Ⅰ期),纤维素期脓胸(Ⅱ期),机化期脓胸(Ⅲ期)[7]。早期结核性脓胸未经规范化治疗可出现胸廓塌陷、支气管胸膜瘘、胸壁破溃流脓、心肺功能受损等并发症。积极的外科手术干预对Ⅰ、Ⅱ期结核性脓胸患者康复具有良好的临床效果,国内外对结核性脓胸的手术适应证及术式仍未形成统一的共识,目前手术方式主要包括传统开胸手术、电视胸腔镜手术及胸腔镜辅助小切口手术[8]。胸腔镜手术相比于传统开胸手术的主要优势为创伤小、出血量少、术后疼痛较轻、并发症少,主要劣势为操作空间小、病灶难以彻底清除[7]。本研究对比分析两组手术患者的术中出血量、术后引流量、胸腔引流管时间及术后住院时间,单孔胸腔镜手术较传统开胸手术具有明显的优势,与相关文献的观点接近[9]。比较分析两组患者的手术时间,两组患者无明显差异,本研究认为单孔胸腔镜暴露视野不如传统开胸手术,操作空间小,操作难度较大,同时也与手术医师的操作技能有关。
本研究中有3例患者术中中转开胸,其中2例为术中大出血,1例胸腔脏壁粘连严重。1例术中出现大出血的患者为Ⅲ期脓胸患者,胸膜纤维板增厚及部分胸膜钙化,分界不清,不易剥离。机化期脓胸(Ⅲ期)常出现胸廓塌陷,肋间隙狭窄,脊柱侧弯,手术操作难度大,术中容易损伤肺组织导致大出血,增厚胸膜分界不清使膈肌破裂,误伤腹腔脏器,术后出现支气管胸膜瘘或肺瘘的风险增加[10-11]。1例为术中损伤肺静脉,出血量大,从手术安全角度考虑中转开胸。1例为全胸腔粘连,病程超过3个月,操作难度大。笔者认为单孔胸腔镜治疗结核性脓性最好选取Ⅰ、Ⅱ期患者,胸腔镜下易完整剥离纤维板,术中肺组织牵拉少,出血量少,肺复张好。部分Ⅲ期初期如胸腔粘连轻亦可尝试选择,操作者需具备娴熟的胸腔镜操作技能,盲目的追求微创手术容易导致胸膜纤维板剥离不彻底、创面渗血增多、肺组织破损多及术后瘘气时间长等并发症的增加,此类患者胸腔镜辅助小切口手术可作为备选项[8]。结核性脓胸胸腔粘连较重,掌握好粘连分离的原则可减少手术时间、减少出血量、降低操作难度。本研究认为一般而言应先分离粘连较轻处,再分离粘连较重處,或先分离视野暴露好、易分离处,先易后难。
与传统开胸手术相比,胸腔镜手术并发症少[12]。Marks DJB等[13]研究认为胸腔镜脓胸剥脱术在肺功能保护、快速康复、减少疼痛等方面较传统开胸手术具有明显优势。本研究中主要并发症包括胸腔积液、肺不张、肺漏气、肺部感染、切口感染,胸腔积液的原因包括胸腔引流管位置较高、术后伤口疼痛、术后营养差等,单孔胸腔镜组有2例出现胸腔积液,传统开胸组有3例,本研究认为单孔胸腔镜组术后引流管在操作孔下缘,相比于传统开胸组引流管位置较高,引流效果较差。传统开胸组术后出现肺不张、肺部感染的概率较单孔胸腔镜组高,主要考虑为手术创面大,疼痛难忍,患者术后咳嗽、吹气球等依从性差。如患者术后伤口疼痛难忍可使用止痛药,鼓励患者咳嗽、咳痰。对于术后伤口疼痛难忍患者待胸腔引流液减少后可尽早拔除胸腔引流管,减轻患者疼痛,在CT或彩超引导下置入胸腔微管(一般使用中心静脉导管),或术中常规留置胸腔微管,术后间断予以尿激酶胸腔冲管,引流效果佳。本研究中出现术后持续漏气2例,均为胸腔粘连重,术中剥离面大,出现较大的肺破口,均采用持续留置胸腔引流管,嘱患者加强营养,保守治疗后痊愈,此外部分文献报道对于持续性漏气可以使用高渗葡萄糖和(或)自体血胸腔注射效果良好[14-15]。结核性脓胸为Ⅲ类切口,术后出现切口感染的概率较Ⅰ、Ⅱ类切口高,术前规律抗结核6~8周可降低术后切口感染发生率。本研究中传统开胸组出现切口感染1例,患者合并2型糖尿病,术前血糖控制欠佳,主要与手术创面大及术后血糖控制欠佳有关。围术期血糖控制在6.0~10.0 mmol/L能有效的减少切口感染发生率[16]。
总之,与传统的开胸手术相比,单孔胸腔镜手术治疗Ⅰ、Ⅱ期结核性脓胸创伤小、并发症少、住院时间短,在临床应用中值得推广,但对于Ⅲ期的结核性脓胸患者应慎重,在临床实际中的应根据具体情况合理选择手术方式。
[参考文献]
[1] 张运曾,金锋,王成.电视辅助胸腔镜手术在结核性脓胸治疗中的应用及进展[J].中国防痨杂志,2017,39(5):525-528.
[2] 李向红,李万志.结核性脓胸126例临床分析[J].中国现代医生,2010,48(8):118-119.
[3] Kumar A,Asaf BB,Lingaraju VC,et al. Thoracoscopic decortication of stage Ⅲ tuberculous empyema is effective and safe in selected cases.[J]. Annals of Thoracic Surgery,2017,104(5):S0003497517309207.
[4] Biritwum RB,Minicuci N,Yawson AE,et al. Prevalence of and factors associated with frailty and disability in older adults from China,Ghana,India,Mexico,Russia and South Africa[J]. Maturitas,2016,91:8-18.
[5] 崖宇翔.伴合并症的肺结核治疗研究进展[J].心理医生,2016,22(34):3-4.
[6] Terzi A,Bertolaccini L,Gorla A,et al. Surgery for the treatment of the tuberculosis-destroyed lung:To protect or not to protect the bronchial stump?[J]. European Journal of Cardio-Thoracic Surgery:Official Journal of the European Association for Cardio-thoracic Surgery,2013, 43(1):201.
[7] Lee SF,Lawrence D,Booth H,et al. Thoracic empyema:Current opinions in medical and surgical management[J].Current Opinion in Pulmonary Medicine,2010,16(3):194.
[8] Barbetakis N,Paliouras D,Asteriou C,et al. Comment:The role of video-assisted thoracoscopic surgery in the management of tuberculousempyemas[J]. Interactive Cardiovascular & Thoracic Surgery,2009,8(3):337.
[9] 徐宁,汤磊,朱峰,等.电视胸腔镜手术治疗结核性脓胸的临床疗效分析[J].中国防痨杂志,2017,39(5):459-463.
[10] Kundu S,Mitra S,Mukherjee S,et al. Adult thoracic empyema:A comparative analysis of tuberculous and nontuberculous etiology in 75 patients[J]. Lung India Official Organ of Indian Chest Society,2010,27(4):196-201.
[11] 鄧勇军,刘焕鹏,喻应洪,等.改良胸腔镜下胸膜纤维板剥脱术治疗慢性脓胸31例[J].中国微创外科杂志,2016, 16(11):1009-1012.
[12] Zhao L,Cao S,Zhu C,et al. Application of thoracoscopic hybrid surgery in the treatment of stage III tuberculous empyema[J].Ann Thorac Cardiovasc Surg,2015,21(6):523-528.
[13] Marks DJB,Fisk MD,Koo CY,et al. Thoracic Empyema:A 12-Year study from a UK Tertiary Cardiothoracic Referral Centre[J]. Plos One,2012,7(1):e30074.
[14] Oliveira FHS,Cataneo DC,Ruiz RL,et al. Persistent pleuropulmonary air leak treated with autologous blood:Results from a university hospital and review of literature[J].Respiration,2010,79(4):302-306.
[15] Fujino K,Motooka Y,Koga T,et al. Novel approach to pleurodesis with 50% glucose for air leakage after lung resection or pneumothorax[J].Surgery Today,2016,46(5):599-602.
[16] 彭海军,段小亮,李建行,等.肺结核合并2型糖尿病患者行电视胸腔镜手术治疗的临床分析[J].医学理论与实践,2014,(16):2109-2111.
(收稿日期:2019-10-12)