头低截石位与Trendelenburg位对妇科腹腔镜手术患者心排血量影响的比较
沈富毅 宋玉洁 赵青松 李 江 刘志强 徐振东
(上海市第一妇婴保健院麻醉科 上海 201204)
The use ofthe laparoscopic proceduresin gynecological surgery has increased in popularity in recent years and has been demonstrated to be safe[1].The major advantages of laparoscopic surgery are less trauma,less post-operative pain and disability,with short hospital period and improved cosmetic effect when compared with conventionalopen procedures[2].Despite these advantages,gynecological laparo-scopies may be associated with some complications due to the physiological changes during the procedure.For example,pneumoperitoneum with carbon dioxide insufflation have potential adverse effects on hemodynamics[3-5].Most previous studies have noted significant decreases in cardiac output(CO)and increases in systemic vascular resistance(SVR),pulmonary vascular resistance(PVR),mean arterial pressure(MAP)and central venous pressure (CVP) when pneumoperitoneum established[6-7].The body position may also affect the hemodynamics[8-9]. Gynecological laparoscopy is usually performed in the head-down lithotomy position or the Trendelenburg position to induce gravitational displacement of viscera away from the surgical site[10].The Trendelenburg position is a supine position with bed angulation to achieve a headdown position,while in the head-down lithotomy group,the patient′s legs were in stirrups and then the bed was angulated to achieve a head-down position.These two positions can raise venous return.However,it is unclear whether these two positions have different effects on patient′s cardiac hemodynamics during the early period after pneumoperitoneum establishment.
The purpose of this study was to investigate the changes in cardiac output and other hemodynamic parameters in the head-down lithotomy position and in theTrendelenburg position.CO measurement involves arterialand centralvenous annulation.Continuous thermodilution using a pulmonary artery catheter(PAC-CCO)is the gold standard for the clinical evaluation of CO,but it is invasive and may cause complications.So this invasive technique may not seem appropriate to low-risk patients undergoing a relatively minorgynecologicalsurgery.Cardiac hemodynamics changes also can be determined by noninvasive techniques.NICOM®system(Cheetah Medical,USA)is a new noninvasive CO monitoring.It can continuously monitor stroke volume(SV)and CO based upon bioreactance technology[11],and has acceptable accuracy and precision,and faster responsiveness with compared to thermodilution[12].During laparoscopic surgery,NICOM brings many advantages:low risk,convenient to use,continuous measurement in real time, and inexpensive[13].Therefore,NICOM®wasusedtoevaluateCO changes in different positions in this study.
Materials and Methods
General informationAfter obtaining approval from the Institutional Review Board of Shanghai First Maternity and Infant Hospital(KS1656) and written informed consent,60 ASA women with physical status ofⅠandⅡscheduled for elective gynecological laparoscopy were enrolled during May 1st and 31st,2016.Exclusion criteria included patients with uncontrolled diseases such as hypertension,heart diseases,respiratory disease,history of drug abuse,patients aged<18 years or > 60 years;and patients with a body mass index(BMI)>30.Patients were randomly allocated into head-down lithotomy group and Trendelenburg group using a random number table,each group containing 30 patients.
AnaesthesiaAfter arriving in the operating room,the patients were placed in the supine position or supine-lithotomy position according to the group to which they belonged.Then,noninvasive blood pressure, pulse oxygen saturation (SPO2) ,electrocardiogram (ECG) weremonitored.Four double electrode stickers were placed on the upper thorax and lateral subcostal regions and connected NICOM®continuously monitoring heart rate(HR),CO,total peripheral resistance(TPR)and SV.
General anaesthesia was induced with midazolam of 0.04 mg/kg ,sufentanil of 0.4 μg/kg,etomidate of0.3mg/kg and cisatracurium of0.2mg/kg.Patients were intubated and ventilated.They were volume-controlled with FiO21.0 with a tidal volume of 8 mL/kg.The inspiratory:expiratory ratio was 1:1.5.The respiratory rate(RR)was adjusted to keep normal end-tidal CO2(EtCO2) in the range of 35-45 mmHg.Anaesthesia was maintained with sevoflurane.
Pneumoperitoneum and patient positioningPneumoperitoneum was established by CO2insufflation.CO2was insufflated at a pressure limit of 12 mmHg.The insufflation rate was regulated at 7.5 L/min.After the establishment of pneumoperitoneum,the patients were placed in a 30°head-down tilt in the lithotomy position or the Trendelenburg position(30°head-down).
Hemodynamic monitoringFive minutes after the placement of patients in either lithotomy position or Trendelenburg position before the establishment of pneumoperitoneum,CO,HR,MAP,SV and TPR were recorded as baseline parameters(TB).All the variables mentioned above were recorded at the time when the patient was placed in the 30°head-down tilt position after pneumoperitoneum establishment(T0).Thereafter,the hemodynamic variables were recorded at 1-min intervals for 10 min (T1-T10)except for MAP and TPR,which were monitored every 5 min.All the parameters were acquired by NICOM®.The study design is presented in Fig 1.
Statistical analysesA priori power analysis was done for sample size calculation using the comparison of CO between both groups as the primary outcome of our study.In preliminary data,the response within each subject group was normally distributed with standard deviation 0.5.The minimum sample size was 27 patients in each group in order to detect a real difference of 0.5 L/min(CO)with 95%power at α=0.05 level using Student′st-test for independent samples.Sample size calculation was done using the PS Power and Sample Size Calculation version 3.0,Visual Components.
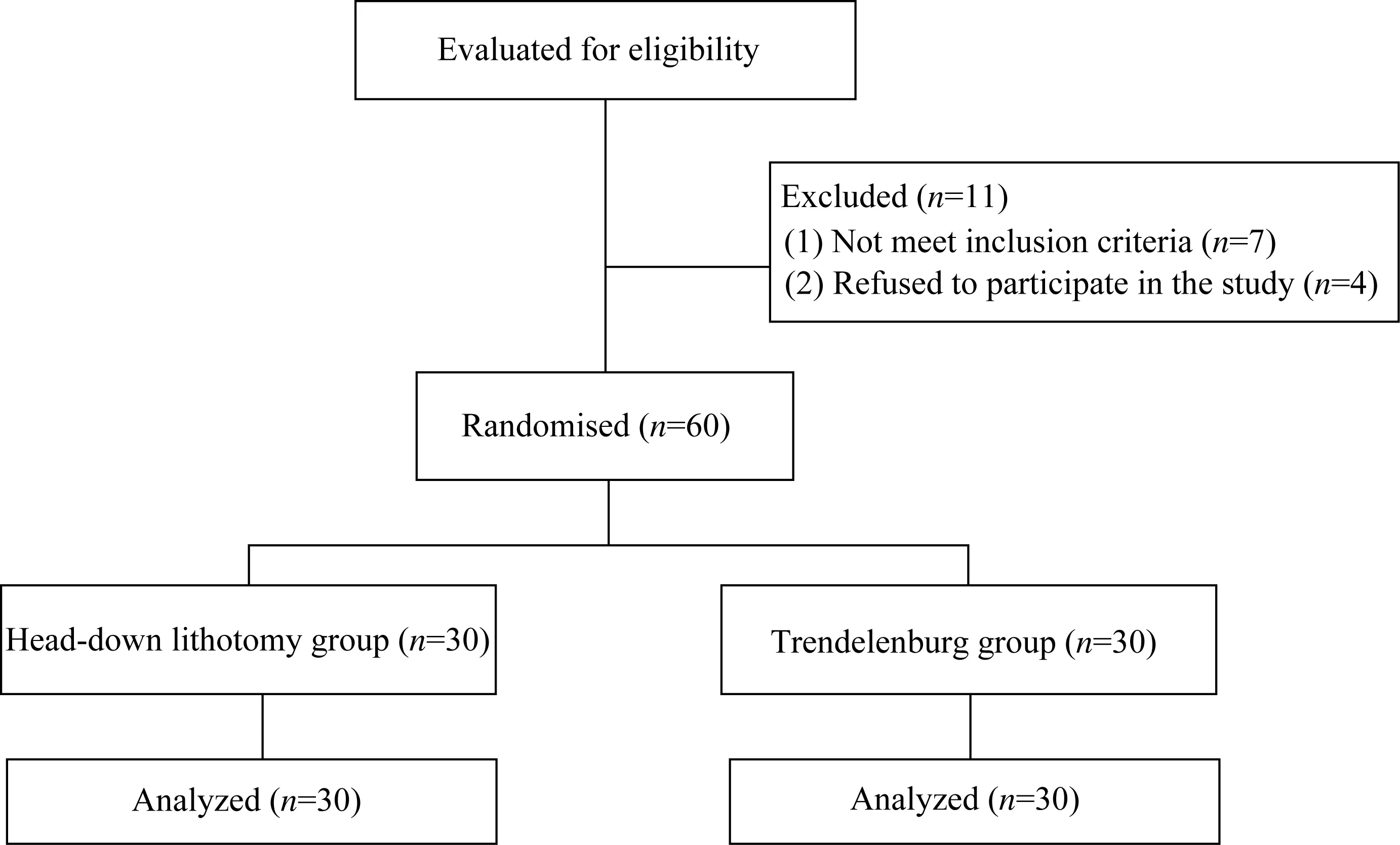
Fig 1 Flow chart of the study showing the number of patients who were screened,included and analyzed
Statistical analysis was performed using the SPSS 19 software.The results are presented as the±s.Analysis of variance with repeated-measures was used to compare the baseline values with values at any pre-defined time point.Unpairedt-test was used to compare repeated recordings of the same variable.Pvalue<0.05 was considered statistically significant.
Results
Demographic dataA total of 30 patients were enrolled in each group.The characteristics of the patients were presented in Tab 1.
Tab 1 Comparison of baseline characteristics between patients in different positions (±s)

Tab 1 Comparison of baseline characteristics between patients in different positions (±s)
There was no significant differences between the two groups.BSA:Body surface area.
Group Head-down lithotomy position(n=30)Trendelenburg position(n=30)BSA(m2)1.6±0.1 1.6±0.1 Age(y)39.0±9.2 34.4±9.4 Height(cm)161.3±5.3 162.6±4.2 Weight(kg)56.9±7.1 56.3±4.5 BMI(kg/m2)21.9±2.6 21.3±2.3
Hemodynamic evaluationBaseline values of the hemodynamic variables were similar between the two groups except for MAP and SV.Compared with Trendelenburg group,the MAP and SV values in head-down lithotomy group were higher at baseline[MAP:(97±11)mmHgvs.(85±6)mmHg;SV:(74.2±13.6)mmHgvs.(66.4±15.0)mmHg,bothP<0.05].All values of CO,HR,SV,MAP and TPR at different time points were shown in Tab 2 and Tab 3,respectively.
Tab 2 Comparison of hemodynamic parameters between patients in different positions at successive points of measurement(±s)

Tab 2 Comparison of hemodynamic parameters between patients in different positions at successive points of measurement(±s)
(1)vs.TB in the same group,P<0.05;(2)Compared between the two groups,P<0.05.A:Head-down lithotomy group;B:Trendelenburg group;TB:Baseline parameters;T0:After pneumoperitoneum establishment;T1-T10:At 1-min intervals for 10 min after T0.
T0 TB T1 T2 T3 T4 T5 T6 T7 T8 T9 T10 Group CO(L/min)A B 6.0±0.8 5.6±1.2 4.1±1.0(1)4.9±1.4(1)4.0±0.9(1)4.5±1.7(1)4.0±1.0(1)4.6±1.2(1)(2)4.0±1.1(1)4.6±1.3(1)4.1±1.1(1)4.7±1.7(1)4.2±1.0(1)4.6±1.6(1)4.1±1.1(1)4.6±1.4(1)4.1±1.1(1)4.4±1.6(1)4.3±1.0(1)4.3±1.6(1)4.2±0.9(1)4.4±1.5(1)4.2±0.8(1)4.3±1.4(1)SV(mL)A B 74.2±13.6 66.4±15.0(2)59.2±13.2(1)67.9±15.2(2)58.2±12.3(1)64.1±18.7 57.7±11.2(1)67.6±16.4(2)58.9±12.4(1)68.7±17.3(2)61.1±12.1(1)71.1±20.0(2)62.6±13.2(1)69.0±18.7 61.9±12.8(1)70.5±14.5(2)61.2±12.4(1)65.5±15.5 62.9±12.0(1)63.8±15.6 61.9±12.5(1)65.7±16.3 61.0±10.7(1)65.2±15.1 HR(bpm)70±12(1)66±9(1)A B 82±8 85±10 69±12(1)72±10(1)70±13(1)70±12(1)69±12(1)68±11(1)68±12(1)66±10(1)67±12(1)66±10(1)67±11(1)66±9(1)66±12(1)65±11(1)67±11(1)66±10(1)68±11(1)67±12(1)70±11(1)66±9(1)
The change in hemodynamic parameters were expressed as percent of depression from the baseline value(Fig 2).
CO showed a sustained and significantly downward trend compared with baseline in both groups(P<0.05,Tab 2).From T0 to T6,the decrease of CO in head-down lithotomy group was more significant compared to Trendelenburg group(T0:-31%±-19%vs.-9%±34%;T1:-32%±18%vs.-16%±38%;T2:-33%±19%vs.-16%±26%;T3:-32%±22%vs.-16%±28%;T4:-31%±18%vs.-12%±38%;T5:-30%±17%vs.-14%±37%;T6:-31%±17%vs.-14%±33%,allP<0.05,Fig 2A).
Stroke volumeSV showed a continuous and significantly decreasing trend compared with the baseline in head-down lithotomy group(P<0.05).No significantchanges ofSV were found in Trendelenburg group,although the SV values tended to increase(Tab 2).While the change in SV was more significant in head-down lithotomy group than in Trendelenburg group(Fig 2B).
Tab 3 Comparison of MAP and TPR between patients in different position at defined time points (±s)

Tab 3 Comparison of MAP and TPR between patients in different position at defined time points (±s)
(1)vs.TB in the same group,P<0.05;(2)Compared between the two groups,P<0.05.A:Head-down lithotomy group;B:Trendelenburg group;TB:Baselineparameters;T0:Afterpneumoperitoneum establishment;T1-T10:At 1-min intervals for 10 min after T0.
T0 TB T5 T10 Group MAP(mmHg)A B 97±11 85±6(2)88±11(1)81±13(2)97±15 92±10(1)98±12 94±13(1)TPR(dynes·s/cm5)1 929±377(1)1 850±492(1)A B 1 340±224 1 297±258 1 772±607(1)1 332±328(2)1 984±543(1)1 613±355(1)(2)
Heart rateHR showed a consistent decreasing trend with no significant difference compared with baseline in both groups(Tab 2),and the decline in head-down lithotomy group was similar to that in Trendelenburg group(Fig 2C).
Mean arterial pressureIn Head-down lithotomy group,MAP significantly decreased atT0 and returned to baseline values at T5(P<0.05).In Trendelenburg group,MAP significantly increased at T5 and T10 (Tab 3).ΔMAP was significantly different between the two groups(T5:0±15%vs.9%±15%,T10:1%±12%vs.12%±18%,bothP<0.05,Fig 3A).

Fig 2 The change of CO,SV and HR expressed as percent of depression from the baseline value

Fig 3 Comparison of ΔMAP and ΔTPR between head-down lithotomy group and Trendelenburg group
Total peripheral resistanceTPR was significantly higher at T0,T5 and T10 compared with baseline in head-down lithotomy group and at T5 and T10 compared with baseline in Trendelenburg group(P<0.05,Tab 3).Compared with Trendelenburg group,the increase of TPR in head-down lithotomy group was significantly higher at T0 and T5(T0:37%±55%vs.5%±28%,T5:52%±49%vs.28%±34%,P<0.05,Fig 3B).
Discussion
Clinically,Trendelenburg position is generally selected for ovarian benign tumor surgery on the premise of satisfying the conditions of laparoscopic surgery. For laparoscopic myomectomy and gynecological malignant tumor surgery,the chief surgeon can choose the surgical position according to the habit,including Trendelenburg position with two legs closed or separated and head-down lithotomy position.In this study,we aimed to investigate and compare the changes in cardiac output and other hemodynamic parameters in these two positions.
In the present study,we found that the 30°headdown tilt further decreases CO during the early period after pneumoperitoneum establishment,while the decrease is significant in the head-down lithotomy position than in the Trendelenburg position.
Influence of pneumoperitoneum and position on cardiac hemodynamics is excessively explored in many studies[5,8,14-15].However,to our knowledge,the hemodynamic effects of different position have not been compared especially during the early period of pneumoperitoneum.
A study analysed hemodynamic changes at 15 min after the creation of pneumoperitoneum,and showed that pneumoperitoneum produce a nonsignificant reduction in CO with a significant decrease in SV.Trendelenburg positioning increase the CO and SV after position changes,which may be related with the increase of venous return[9].An early reports,in which a Swan-Ganz catheter was used,demonstrated that Trendelenburg position increased the central venous pressure(CVP)and pulmonary capillary wedge pressure(PCWP)without changes in cardiac performance in awake patients or during anesthesia. CO2-insufflation in Trendelenburg position also produced no change in cardiac index(CI) at the beginning of the laparoscopy when compared with the same head-down position during anesthesia[14].It may be related to the increase of venous return which compensates the negative effect of pneumoperitoneum on cardiac output.
Unlike that study,we changed the position after the CO2-insufflation and focused on the continuously hemodynamic variations during this period.We found that CO was significantly decreased in both groups after the establishment of position following CO2-insufflation.Then CO was further reduced in two groups after the patients were positioned in the 30°head-down tilt.Interestingly,ΔCO reduction was larger in head-down lithotomy than in Trendelenburg group in the first6 min after30°head-down positioning.
It has found a decrease in CO after pneumoperitoneum establishment in many studies[6-7,16].During CO2-insufflation,an acute increase in SVR may induce ventricular dysfunction which is evidenced by transoesophageal echocardiography(TEE)[6].Generally, head-down position raises venous return,while SV reflects the amount of venous return(preload)[17].We also found the ΔSV increases in Trendelenburg position,but we did not find the same phenomenon in head-down lithotomy position.It is probably because venous return had increased when the lithotomy position was placed before CO2-insufflation,and 30°head-down tilt may not further increase venous return.Liu,et al[10]demonstrated that lower extremity venous pressure oflithotomy position wassignificantly increased when compared with the supine position after pneumoperitoneum,which may further decrease the venous return in lithotomy position.In the present study,ventricular dysfunction and reduction of venous return may contribute to the reduction of CO especially in lithotomy position. This finding suggested that there was a significant alteration of cardiac performance that placed the patients at risk,and underthe premise ofmeeting the surgical requirements,surgeons should try to choose the Trendelenburg position for surgery,especially for elderly patients with pre-existing cardiopulmonary disease.Anaesthesiologists and surgeons should pay special attention to the early stage of insufflation and positioning,especially for head-down lithotomy position.
Suh,et al[18]described that MAP was elevated after the creation of pneumoperitoneum and that the position change did not result in any further pressure changes.In ourstudy,differentblood pressure changes were observed between the two groups.MAP in head-down lithotomy group[(97±11)mmHg] was statistically higher than that in Trendelenburg group[(85±6)mmHg](P<0.05)when the patients were placed in the supine position or the lithotomy position before anaesthesia without the 30°head-down tilt.In head-down lithotomy group,MAP significantly decreased at the moment when patients were turned to the 30°head-down tilt position and returned to baseline 5 min later.However,in Trendelenburg group,MAP increased 5 min after the establishment of pneumoperitoneum and positioning(T5:9%±15%;T10:12%±18%);this is similar to what has been found in Harris's research on patients in the Trendelenburg position during laparoscopic colectomy[6].
HR was reduced in both groups compared with baseline values,and there was no significant differences in the range of the decrease between the two groups.The reduction of HR may have resulted from a vasovagal reaction due to the rise in intraabdominal pressure,which has a negative effect on the cardiac conduction system[19].Bradycardia was not observed.Bradycardia during gas insufflation is not necessarily a benign event and appears to be a critical early warning sign for possible impending and unexpected cardiac arrest.Immediate deflation of the pneumoperitoneum and atropine administration are effective measures that may alleviate bradycardia and prevent the progression to cardiac arrest[20].
TPR was significantly elevated in both groups,which was also reported by previous studies[6].Earlier and greater elevation of TPR were observed in head-down lithotomy group(T0:37%±55%vs.5%±28%;T5:52%±49%vs.28%±34%,bothP<0.05).The increase in TPR may have resulted from the augmentation of intra-abdominal pressure.Leg raising after insufflation may have delayed TPR elevation in patients in the Trendelenburg position.
This study had two limitations.Firstly,patients were placed in the position according to the group they were assigned to when they entered the operation room.Therefore,we did not obtain MAP values forpatients in the head-down lithotomy position when they were in the supine position.We chose a noninvasive way to monitor MAP at an interval of 5 min because a shorter interval would lead to subcutaneous haemorrhage in the upper limb.Therefore,we could not continuously monitor MAP.Secondly,we did not set the hemodynamic parameters before positioning as baseline.This is because we aimed to investigate the effect of headdown tilt change after CO2-insufflation on the cardiac hemodynamic.
In conclusion,during the first 10 min after the adjustment of patients' position,CO was significantly decreased in both groups.The mean reduction was larger in patients in the head-down lithotomy position than those in the Trendelenburg position.Therefore,anaesthesiologists and surgeons need to be cautious in the early periods of insufflation and positioning.