Predictive factors for central lymph node metastases in papillary thyroid microcarcinoma
Xin Wu, Bing-Lu Li, Chao-Ji Zheng, Xiao-Dong He, Department of General Surgery, Peking Union Medical College Hospital, Chinese Academy of Medical Sciences and Peking Union Medical College, Beijing 100730, China
Abstract
Papillary thyroid microcarcinoma (PTMC) measures 1 cm or less in its longest dimension. The incidence of PTMC is increasing worldwide. Surgery is the primary treatment; however, prophylactic central lymph node dissection is controversial, and discrepancies between different guidelines have been noted.Routine prophylactic central lymph node dissection may result in hypoparathyroidism and recurrent laryngeal nerve injury in some patients without lymph node metastasis, while simple thyroidectomy may leave metastatic lymph nodes in high-risk patients. To selectively perform prophylactic lymph node dissections in high-risk patients, it is important to identify predictive factors for lymph node metastases in patients with PTMC. Several studies have reported on this, but their conclusions are not entirely consistent. Several clinicopathologic characteristics have been identified as risk factors for central lymph node metastases, and the most commonly reported factors include age,gender, tumor size and location, multifocality, bilaterality, extrathyroidal extension, and abnormal lymph node found using ultrasound. Here, we provide an overview of previous studies along with a favorable opinion on or against these factors, with the aim of increasing the understanding of this topic among the medical community. In addition, current opinions about prophylactic central lymph node dissection are reviewed and discussed.
Key words: Papillary thyroid carcinoma; Papillary thyroid microcarcinoma; Central lymph node dissection; Prophylactic; Risk factor; Prognosis
INTRODUCTION
The incidence of thyroid carcinoma is increasing worldwide. In 2015, over 62000 and 90000 patients were diagnosed with thyroid cancer in the United States and China,respectively[1,2]. However, the mortality from thyroid carcinoma has changed little over the past several decades[1]. Different subtypes of thyroid carcinoma demonstrate completely different clinical behaviors. Indolent tumors and aggressive malignancies should be treated using a different therapeutic approach. Differentiated thyroid carcinoma is the most common type of thyroid carcinoma, and papillary thyroid carcinoma (PTC) is the most common subtype of differentiated thyroid carcinoma.Papillary thyroid microcarcinoma (PTMC) is defined as a PTC measuring 1 cm or less in its longest dimension and has a disease-specific mortality rate, local recurrence rate,and distant metastases rate of < 1%, 2%-6%, and 1%-2%, respectively[3-6]. The excellent prognosis may be related to the indolent nature of PTMC. Some prospective clinical studies reported that only a few PTMC patients showed tumor progression after longterm observation[7,8]. Surgery remains to be the primary treatment method; however,the treatment pattern, especially the extent of surgery, is controversial, and discrepancies between different guidelines have been observed[6,9-11]. An important point of contention is the need for prophylactic central lymph node dissection in PTMC. Routine prophylactic central neck dissection may result in recurrent laryngeal nerve injury and hypoparathyroidism in some patients without lymph node metastasis. Conversely, simple thyroidectomy may leave metastatic lymph nodes in high-risk patients. Therefore, it is necessary to identify predictive factors for lymph node metastases in patients with PTMC and to selectively perform prophylactic lymph node dissections in high-risk patients. In this paper, we review the published literature on possible predictive factors for central lymph node metastases in PTMC patients, with the aim of increasing the understanding of this topic among the medical community.
PREDICTIVE FACTORS
Several different predictive factors for central lymph node metastases in patients with PTMC have been reported. These mainly include three aspects: Demographic characteristics, ultrasonography features, and pathological results. The most commonly reported factors include age, gender, tumor size and location,multifocality, bilaterality, extrathyroidal extension, and abnormal lymph node found using ultrasound. We will review each of these factors below.
Age
Age is a very important factor in the staging system for thyroid carcinoma. The latest American Joint Committee on Cancer (AJCC) TNM staging system utilizes age as an important basis for staging[12]. Moreover, previous studies indicated that age was a risk factor for central lymph node metastases in patients with PTMC[13-17]; however, the age threshold varied between the studies. Luoet al[18]studied 1031 patients with PTMC and reported that people aged ≤ 40 years were prone to central lymph node metastases. Yinet al[19]retrospectively reviewed 1092 PTMC patients and found that the age of < 45 years was an independent predictor of central lymph node metastases.Wanget al[20]conducted a study on 8668 PTMC patients and revealed that the age of <55 years was significantly associated with central lymph node metastases. One of our published reports revealed that age < 45 years was an independent risk factor for central lymph node metastases in patients with PTMC[21]. Despite the variability in the cut-off value for age, the consensus is that young patients have more lymph node metastases than older patients. While focusing on the relationship between age and lymph node metastases, many studies examined the relationship between age and disease prognosis. Some studies reported that a cut-off of 55 years was much more suitable than 45 years as the predictive factor for disease-specific survival of PTC patients[22-29]. Moreover, the AJCC staging system increased the cut-off age at diagnosis from 45 years to 55 years in its eighth edition[12]. Interestingly, most studies indicate that young age is a risk factor for lymph node metastases, while older age is linked to a poor prognosis. A high rate of lymph node metastases is therefore not equal to a poor prognosis. In general, elderly patients tend to have more age-dependent physiological changes, weaker health, and more complications that result in a worse prognosis than younger patients.
Gender
In women, the inc idence of PTMC is much higher but the rate of lymph node metastases is lower than in men[30]. The higher levels of progesterone and estrogen in women than in men can affect the pituitary gonadotropin-releasing hormone levels and result in this phenomenon[31,32]. Concurrently, the higher basal metabolic rate of men may incite an overactive proliferation of tumor cells, which makes men more prone to metastases than women. Zhanget al[33]conducted a retrospective analysis of 1304 cases and reported that being male was an independent predictor of central lymph node metastases in cN0 PTMC patients. In addition, Zhenget al[34]indicated that being male was an independent risk factor for central lymph node metastases in PTMC. Numerous other studies confirmed the association between male gender and lymph node metastases in PTMC[35-37]. Nonetheless, the association between sex and PTMC remains controversial. Jeonet al[38]demonstrated that being male was not an independent risk factor, and Jianget al[39]found no relationship between central lymph node metastases and sex in cN0 PTC patients. In addition to sex and lymph node metastases, researchers studied the relationship between sex and prognosis. Leeet al[40]studied 2930 patients with PTC in a single institution and found that men with PTC had higher rates of recurrence and mortality than women, but there were no differences in disease-free survival rates between the two sexes of patients with PTMC. Thus, in patients with PTMC, sex plays different roles in lymph node metastases and prognosis.
Tumor size
Tumor size is a very important characteristic in most tumor staging systems. For PTC,the definition of T-stage is shown in Table 1. All PTMC patients belong to stage T1a(tumor ≤ 1 cm limited to the thyroid). As early detection of PTMC is the main reason for the rapid increase in the incidence rates of thyroid carcinoma[15,41], researchers hope to stratify the size of PTMC in further detail. When relationships between tumor size and lymph node metastases were studied, several different sizes were quoted. In their study which included 673 patients with PTMC, Jinet al[42]revealed that a tumor size of> 5 mm was an independent predictor of central lymph node metastases. Moreover,Yuet al[43]retrospectively studied 917 patients with PTMC and found that a large tumor size (> 5mm) was an independent factor in the prediction of central lymph node metastases in PTMC patients. A meta-analysis of 19 studies involving 8345 PTMC patients demonstrated that central lymph node metastases were associated with large tumor size (> 5 mm)[44]. A cut-off of 5 mm is accepted and recommended by most published studies[16,18,20,33,35]. In addition, some other sizes have been acknowledged by different studies. Leeet al[45]studied 275 patients with PTMC and found that a tumor size of ≤ 7 mm was less likely to be associated with aggressive features than a tumor size of > 7 mm and recommended a cut-off of 7 mm as the threshold of PTMC tumor size. Zhenget al[34]assessed thresholds greater than 8 mm, 7 mm, 6 mm, 5 mm, and 4 mm and concluded that a tumor size of > 6 mm significantly correlated with central lymph node metastases in PTMC. Guiet al[14]used 5.75 mm as the threshold, while Xuet al[15]deduced the size to be that of 7 mm. Nevertheless, the consensus is that the smaller the tumor, the lower the probability of lymph node metastases. Moreover, tumor size significantly correlates with tumor prognosis. To ensure correct and predictable prognosis of small-sized PTMC, the United Kingdom National Multidisciplinary Guidelines recommended against thyroid stimulating hormone suppression treatment in solitary PTMC with a tumor size of ≤ 5 mm and without the presence of adverse risk factors (being symptomatic, positron emission tomography positivity, extrathyroidal extension, poorly differentiation, desmoplastic fibrosis, and/or infiltrative growth pattern)[10].
Tumor location
The thyroid gland is composed of two lobes and an isthmus, and sometimes, apyramidal lobe is present. For lesions in the right and left lobes, tumor location is described as the upper portion (upper than the high plane of the isthmus), the middle portion (parallel to the isthmus), and the lower portion (lower than the low plane of the isthmus). Alternatively, tumor location is described as upper third, middle third,and lower third. Tumors at different locations have different tendencies of lymphatic metastases. Zhanget al[46]followed 1066 consecutive PTMC patients over a 5 year period and revealed that for PTMC patients with a solitary tumor, the upper portion was associated with a high risk of lateral lymph node metastases but a low risk of central lymph node metastases. Xuet al[47]found that in PTMC patients with a solitary tumor, the lower portion was associated with a high risk of central lymph node metastases. Luoet al[18]found that the lower portion was related to a high risk of central lymph node metastases while the upper portion conferred a high risk of lateral lymph node metastases. In addition, Jinet al[42]reported that the lower portion was an independent risk factor for central lymph node metastases. In a previous study, we found that the tumor location (upper portion) was an independent risk factor for lateral neck lymph node metastases in patients with PTMC[48]. Different rates of lymphatic metastases among different tumor locations may be related to different lymphatic flow pathways. Tumor cells from the lower portion are easily transported to the pretracheal and paratracheal lymph nodesviathe lymphatic flow along the inferior thyroid vein, while lesions of the upper portion are easily transported to the lateral neck lymph nodesvialymphatic flow along the superior thyroid artery[49,50]. A full understanding of the relationship between tumor location and lymphatic metastases is important in determining the extent of lymph node dissection.
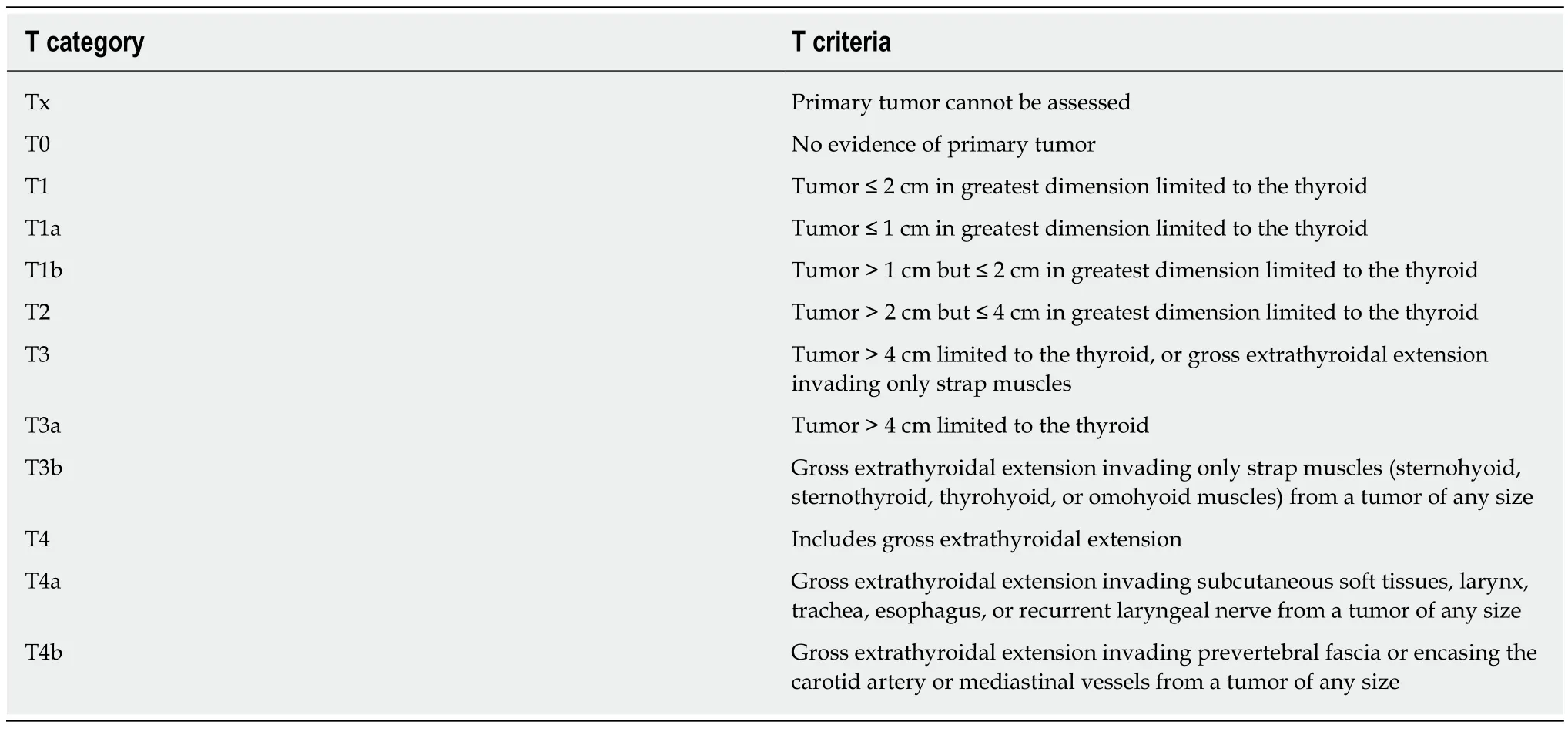
Table 1 The definition of T-stage for papillary thyroid carcinoma
Multifocality
If more than one focus is found in bilateral or unilateral thyroid gland lobes, the tumor is considered to be multifocal. This phenomenon is observed in approximately 20%-40% of patients with PTMC[51-55]. Multifocality is considered as increased development of independent cancers or intraglandular spread of the primary focus[56-59]. Although most tumor staging systems do not include multifocality, it is considered as an independent risk factor for lymph node metastases in patients with PTMC[14,15,17,18,60]. Zhenget al[61]studied 3543 patients with PTMC and found that multifocality with ≥ 3 tumor foci was a risk factor for central lymph node metastases in PTMC. Similarly, Guoet al[62]reported that multifocality was associated with a high risk of central lymph node metastases in PTMC. Additionally, a meta-analysis study revealed the same phenomenon[44]. Conversely, Zhouet al[63]concluded that multifocality was not significantly related to central lymph node metastases in multivariate analysis. Leeet al[64]reported that multifocality was not a risk factor for central lymph node metastases. Thus, there is a lack of consensus on the relationship between multifocality and central lymph node metastases. In addition to lymph node metastases, the association between multifocality and prognosis has been studied.Some previous studies found that multifocality was significantly associated with tumor recurrence[51,53], but other studies showed no direct relationship between multifocality and tumor recurrence in PTMC[54,65]. The prognostic value of multifocality in PTMC needs to be confirmed through further research.
Bilaterality
Bilaterality is a special situation of multifocality, and over 80% of multifocality cases are associated with bilaterality[33,63]. It has been reported that bilaterality could increase the rate of lymph node metastases in PTMC[33-35,66]. Kimet al[67]retrospectively reviewed 5656 patients with PTMC and found that bilaterality was an independent risk factor for a high prevalence of central lymph node metastases. Kimet al[68]studied 483 PTMC patients and found that bilaterality was significantly associated with central lymph node metastases. Conversely, several studies revealed a negative result of the association between bilaterality and lymph node metastases. Yanget al[69]retrospectively studied 291 patients and found no relationship between bilaterality and central lymph node metastases. A meta-analysis that included 14 studies and 4573 patients reported that an elevated risk of central lymph node metastases was associated with multifocality but not with bilaterality[70]. Another meta-analysis of 25 studies involving 7719 patients revealed that bilaterality was not significantly associated with central lymph node metastases[71]. Debates on this topic are ongoing.Different patient selection criteria and statistical methods could result in contradicting conclusions. Moreover, the complex lymphatic flow pathways of the thyroid may play an interfering role.
Extrathyroidal extension
Extrathyroidal extension in PTMC includes various extents of invasion such as the perithyroid tissues, strap muscles, recurrent laryngeal nerves, trachea, esophagus,larynx, prevertebral fascia, and mediastinal vessels. Several studies have reported that extrathyroidal extension was a risk factor for central lymph node metastases in PTMC[46,47,72,73]. Both Gülbenet al[74]and Wanget al[75]reported that thyroid capsular invasion was an independent risk factor for lymph node metastases. Varshneyet al[76]studied 685 consecutive patients and found that there was a significant association between extrathyroidal extension and lymph node metastases. The extrathyroidal extension means that tumor cells have broken through the thyroid gland, which increases the probability of lymph node metastases. However, accurate diagnosis of the extension is challenging since the thyroid gland does not have a well-defined true capsule and the thyroid gland capsule is made up of inconspicuous thin fibrous tissues[34]. Additionally, it is controversial whether minor extension identified only on histological examination has a different effect on metastases and prognosis in PTMC as compared to gross extrathyroidal extension. The latest AJCC TNM staging system highlighted that gross extrathyroidal extension was an unfavorable prognostic factor and downplayed the significance of minor extension[12]. Nonetheless, Guiet al[14]examined 541 PTMC patients and found that the rate of microscopic extrathyroidal extension was significantly different between patients with and without lymph node metastases. Future studies are warranted on the differences in clinical manifestations and molecular mechanisms between minor and gross extensions.
Abnormal lymph node detected by ultrasound
Ultrasonography is the most effective and convenient preoperative thyroid examination. Metastatic lymph nodes are often round in shape, with loss of fatty hilum, calcification in the cortex, cystic changes, hypoechogenicity, and peripheral vascularity[6,77,78]. However, it is very difficult to achieve a satisfactory rate of diagnosis prior to surgery because the exploration of central lymph nodes is significantly affected by glands, bones, and gas[79]. Several studies reported that the sensitivity of ultrasonography in identifying central lymph node metastases was quite low[73,80,81]. Yuet al[43]reported that less than 30% of central lymph node metastases confirmed by frozen section in patients with PTMC could be diagnosed by preoperative ultrasonography. Moreover, our previous study found that only 21% of central lymph node metastases could be correctly diagnosed by preoperative ultrasonography[21].Additionally, Itoet al[30]reported a preoperative ultrasonography sensitivity of just 10.9%. Conversely, the specificity of preoperative ultrasonography is quite high[21,79].Huanget al[82]reported that ultrasonography has sensitivity and specificity rates of 12.5% and 95.2%, respectively, for the evaluation of lymph nodes. Leeet al[83]studied 184 consecutive PTC patients and found that ultrasound had a specificity of 88.4% in assessing central lymph nodes. Therefore, the possibility of metastases is very high if an abnormal lymph node is detected on ultrasound. Nevertheless, ultrasound is an affordable and noninvasive procedure that is easy to perform. Other imaging modalities such as computed tomography, positron emission tomography, and magnetic resonance imaging have all been recommended as an adjunct to ultrasound[6].
Other factors
In addition to the most commonly reported factors discussed above, some other factors have been reported. Luoet al[18]revealed that a sum of the maximum diameter of multifocal lesions of ≥ 8.5 mm in the unilateral lobe was prone to central lymph node metastases in PTMC. In addition, they reported that the probability of lateral lymph node metastases increases with an increase in the sum of the maximum diameter of multifocal lesions in a unilateral lobe. The authors, therefore, stated that attention should be paid to multifocal lesions and the sum of their maximum diameter in PTMC patients. Wanget al[20]reported that lateral lymph node metastases were significantly associated with central lymph node metastases. Jinet al[42]found that BRAF mutation was an independent predictor of central lymph node metastases.These factors have attracted great attention and been studied by several researchers.
PROPHYLACTIC CENTRAL NECK DISSECTION
For PTC, the definition of N-stage is shown in Table 2. The central compartment (level VI) contains pretracheal, paratracheal, and prelaryngeal lymph nodes. Central compartment lymph node dissection should be performed superior to the hyoid bone,inferior to the innominate (brachiocephalic) artery, and lateral to the carotid sheaths.In clinical practice, central neck dissection in thyroid carcinoma can be divided into therapeutic dissection and prophylactic dissection. Therapeutic central compartment lymph node dissection is recommended and routinely performed in PTC patients with clinically positive lymph nodes[6,84,85]. However, the use of prophylactic central compartment lymph node dissection is controversial, especially in PTMC patients with clinically negative lymph nodes[6,10,11,86,87]. Aggressive treatment often increases complications such as hypoparathyroidism and recurrent laryngeal nerve injury,while conservative treatment may result in an increased rate of recurrence.
Many researchers have studied and reported the clinical effects of prophylactic central neck dissection. Kimet al[88]performed a randomized clinical trial and followed 164 PTMC patients for a mean duration of 73.4 mo. They found that prophylactic ipsilateral central neck dissection did not provide any oncological benefit for PTMC patients with clinically negative lymph nodes. Xuet al[89]studied 611 consecutive patients and concluded that routine prophylactic central compartment lymph node dissection was not a protective factor for lateral neck recurrence-free survival in patients with PTMC and clinically negative lymph nodes. Similarly,several meta-analyses[90-92]did not support prophylactic central neck dissection in PTMC patients without clinical lymph node metastases due to a lack of high-level evidence in favor of the procedure. In contrast, some researchers advocated for prophylactic central neck dissection due to the high rates of occult metastatic lymph nodes in clinical negative patients[30,93,94]. Suet al[95]conducted a meta-analysis which highlighted that thyroidectomy plus prophylactic central neck dissection may reduce recurrence rates in patients with PTMC. Another meta-analysis that included five studies with 1132 patients reported that prophylactic central neck dissection does not increase the permanent morbidity rate such as hypocalcemia and vocal cord palsy[96].
The oncologic benefit of routine prophylactic central neck dissection is still controversial. It is essential to identify high-risk patients prior to surgery and to subsequently perform prophylactic central neck dissection in selected patients. The various guidelines currently available provide different treatment options. The American Thyroid Association recommends prophylactic central neck dissection for patients with advanced primary tumors (T3 or T4) or clinical positive lateral lymph nodes metastases (cN1b)[6]. Furthermore, it clarifies that thyroidectomy without prophylactic central neck dissection is an appropriate indication for PTC patients with noninvasive, clinically node-negative, and small primary tumors (T1 or T2)[6]. The European Society of Endocrine Surgeons suggests that prophylactic central neck dissection should be risk-stratified[11]. The potential risk factors include large tumors(T3 or T4), age ≥ 45 years or ≤ 15 years, male sex, bilaterality or multifocality, and involvement of lateral lymph nodes[11]. The United Kingdom National Multidisciplinary Guidelines indicated that prophylactic central neck dissection is associated with a high incidence of long-term permanent hypoparathyroidism and recurrent laryngeal nerve damage and therefore, not recommend prophylactic central neck dissection in low-risk and small papillary carcinomas[10]. Conversely, the Chinese Association of Thyroid Oncology and Chinese Anti-Cancer Association recommends prophylactic central lymph node dissection for cN0 PTMC patients[9]. Nonetheless, it emphasizes the importance of parathyroid gland and recurrent laryngeal nerveprotection[9].
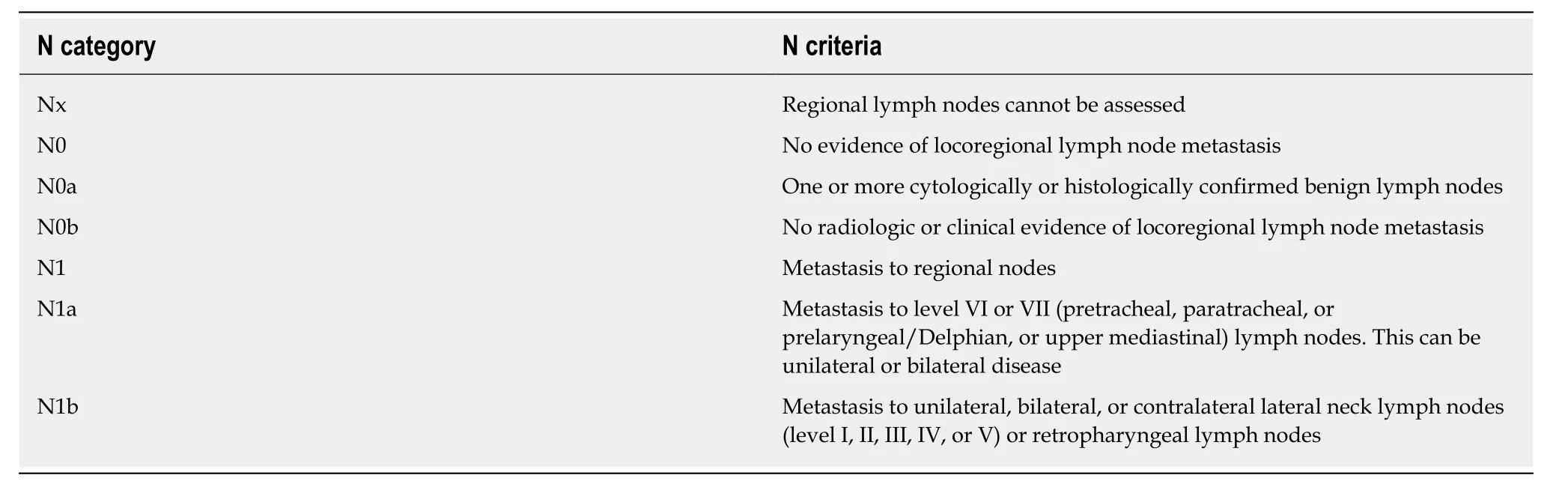
Table 2 The definition of N-stage for papillary thyroid carcinoma
CONCLUSION
Many clinicopathologic factors have been studied as predictors of central lymph node metastases in patients with PTMC. The most interesting and commonly discussed factors include age, gender, tumor size and location, multifocality, bilaterality,extrathyroidal extension, and abnormal lymph node on ultrasound. Studies have been published with a favorable opinion on or against each of these factors. To preoperatively assess whether a PTMC patient is at high risk for lymph node metastases, the presence of a combination of different factors is required. Prophylactic central neck dissection is a controversial procedure and should only be performed selectively in high-risk patients.
 World Journal of Clinical Cases2020年8期
World Journal of Clinical Cases2020年8期
- World Journal of Clinical Cases的其它文章
- Probiotic mixture VSL#3: An overview of basic and clinical studies in chronic diseases
- Mucosa-associated lymphoid tissue lymphoma simulating Crohn’s disease: A case report
- Embolization of pancreatic arteriovenous malformation: A case report
- Novel frameshift mutation in the SACS gene causing spastic ataxia of charlevoix-saguenay in a consanguineous family from the Arabian Peninsula: A case report and review of literature
- Duodenal mature teratoma causing partial intestinal obstruction: A first case report in an adult
- Rare anaplastic sarcoma of the kidney: A case report
