Gastric pyloric gland adenoma resembling a submucosal tumor: A case report
Cong-Cong Min, Jun Wu, Feng Hou, Tao Mao, Xiao-Yu Li, Xue-Li Ding, Hua Liu
Cong-Cong Min, Jun Wu, Tao Mao, Xiao-Yu Li, Xue-Li Ding, Hua Liu, Department of Gastroenterology, The Affiliated Hospital of Qingdao University, Qingdao 266003, Shandong Province, China
Feng Hou, Department of Pathology, The Affiliated Hospital of Qingdao University, Qingdao 266003, Shandong Province, China
Abstract
Key words: Pyloric gland adenoma; Submucosal tumor; Endoscopic submucosal dissection; Case report
INTRODUCTION
Gastric adenomas are benign lesions of the stomach, and comprise less than 10% of all gastric polyps[1]. Gastric adenomas are categorized into gastric and intestinal type according to the 2019 World Health Organization classification[2]. Gastric adenomas comprise pyloric gland adenoma (PGA) and foveolar-type adenoma. PGAs are rare neoplasms with gastric differentiation, first described by Elster[3]in 1976.Subsequently, similar lesions have been gradually recognized in some case reports and small case series. This lesion most frequently occurs in the stomach, but also occurs in the duodenum, esophagus, gallbladder, bile duct, pancreas, and rectum[4-7].In the stomach, PGAs account for 2.7% of all gastric polyps, as observed in the largest study with 90 cases[8]. PGAs endoscopically present as flat, polypoid or mass lesions[9-12]. Moreover, a PGA presenting as a submucosal tumor (SMT) is uncommon.PGAs are considered to be precancerous lesions and have a 12.2%-47% rate of transformation into adenocarcinoma[10,13,14]. However, limited information is available regarding the clinicopathological features, endoscopic performances, and pathogenesis as well as prognoses of PGAs.
Here, we report a case of gastric PGA with an SMT-like appearance that was treated with endoscopic submucosal dissection (ESD) and that could have easily been neglected and have remained under-diagnosed.
CASE PRESENTATION
Chief complaints and history of present illness
A 69-year-old Chinese man presented to our hospital for evaluation and management of an epigastric distention for over a year. He was repeatedly diagnosed with chronic gastritis, and the symptoms were alleviated by administering proton pump inhibitors.Incidentally, an SMT-like lesion with an opening on the upper part of the gastric body was discovered on gastroscopy over 3 mo prior.
History of past illness
He had a history of hypertension for 10 years and was ingesting oral telmisartan 80 mg every day regularly. His blood pressure was controlled and relatively stable. He had no history of surgery and allergic drugs.
Personal and family history
He had an extensive smoking history of 40 years, with an average of 20 cigarettes per day. This patient had no familial history of genetic diseases.
Physical examination upon admission
Physical examination revealed that he was 170 cm in height and 73 kg in weight, with a blood pressure of 127/92 mmHg and pulse rate of 67 beats per minute. There were no other obvious abnormalities during physical examination.
Laboratory examinations
After admission, the patient underwent thorough evaluations including routine investigations of the blood, urine, feces and occult blood, blood biochemistry, and common serum tumor markers such as carcinoembryonic antigen, carbohydrate antigen 19-9, alpha-fetoprotein, and carbohydrate antigen 724. No significant abnormalities were recorded in these investigations.
Imaging examinations
Upper gastrointestinal endoscopy revealed non-atrophic gastritis withoutHelicobacter pylori (H. pylori)infection in the background mucosa. An SMT-like elevated lesion with a diameter of 10 mm was located at the posterior wall of the upper part of the gastric body, with an opening on the surface of the tumor (Figure 1A). Next,magnifying endoscopy with narrow-band imaging (ME-NBI) revealed a regular surface microstructure and microvascular pattern (Figure 1B). Additionally, ME-NBI revealed that the orifice showed dilated glandular duct arising from the deeper mucosa.
Endoscopic ultrasound (EUS, 20 MHz; Olympus, Tokyo, Japan) revealed a 10.6 mm× 5.5 mm equal echoic mass with several cysts located in the submucosal layer with an intact muscularis (Figure 1C). The biopsy results indicated chronic non-atrophic,H.pylori-negative gastritis.
FINAL DIAGNOSIS
According to the endoscopic performance and histopathologic examination, the patient was diagnosed with PGA.
TREATMENT
On the basis of the examination results, the diagnosis of SMT-like tumor in the upper part of the gastric body was uncertain. Diagnostic ESD was performed on the patient to confirm the diagnosis. An elevated tumor measuring 13 mm × 10 mm was identified in the ESD specimen with white mucus oozing out from the opening in the middle when squeezed (Figure 1D). In routine hematoxylin and eosin staining, the low-magnification view revealed that the lesion was located in the submucosal layer,showing a nodular appearance with clear boundaries and increasing number of glands in the lamina propria of the orifice (white arrow) (Figure 2A). The highmagnification view showed that some glandular cavity was irregular, with cystic expansion (orange arrow) and interstitial edema (Figure 2B). The tumor consisted of mucus-rich packed tubular glands lined with cuboidal or low columnar epithelial cells containing an eosinophilic cytoplasm and round nuclei, similar to that in pyloric glands (Figure 2C). There was slight epithelial dysplasia in some areas. Additionally,immunohistochemical staining demonstrated positivity for both mucin 6 (MUC6) and MUC5AC but negativity for MUC4 and p53, and the Ki-67 labeling index was about 2% (Figure 2C-F). According to the above histologic results, we finally made a diagnosis of PGA. Adenocarcinoma components were not identified in the ESD specimen. The horizontal and vertical margin were negative, resulting in complete and curative resection.
OUTCOME AND FOLLOW-UP
The lesion was removed completely by ESD. However, the patient will need to undergo a regular gastroscopy follow-up after surgery.
DISCUSSION
PGA is an uncommon neoplasm that has been gradually recognized in the past few decades. Since Elster[3]first described PGA in a book chapter in 1976, similar lesions were subsequently reported in some cases and small series of clinical studies. The majority of reports on PGA are published by other nations, with a lack of awareness in China.
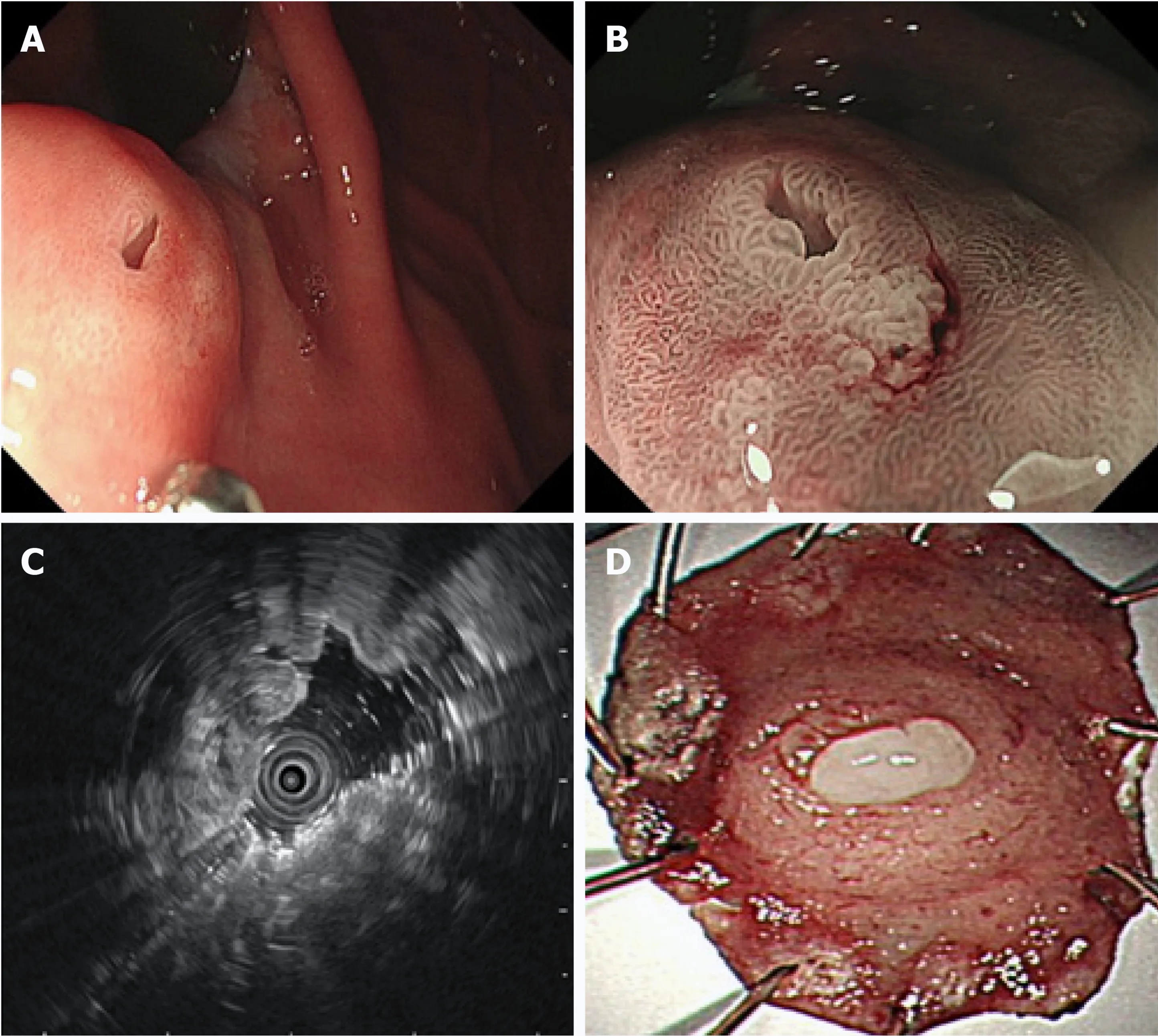
Figure 1 Endoscopic findings. A: A 10 mm submucosal tumor-like elevated lesion with an opening in the posterior wall of the upper part of the gastric body was observed by white light endoscopy; B: A regular microvascular pattern was observed using magnifying endoscopy with narrow-band imaging (magnification: × 40); C: Isoechoic mass (10.6 mm × 5.5 mm) with multiple cysts could be observed in the submucosal layer with intact muscularis using endoscopic ultrasound; D: An elevated tumor measuring 13 mm × 10 mm with oozing white mucus could be observed in the endoscopic submucosal dissection specimen.
Previous studies have shown that PGAs occur more frequently in older women[8,14].Viethet al[8], in one of the largest studies with 90 PGA patients, reported a 2.5:1 ratio for women to men with an average age of 73 years. The predilection site for PGA is the corpus/fundus (64%) of the stomach, followed by cardia (8%), antrum (7%) and intermediate zone (5%), and others occurred in the extra-gastric sites, similar to observations of Choiet al[10]. PGAs present with large lesions at the time of diagnosis,with an average size of 1.6-2.3 cm reported in multiple case reports and clinical studies[8-10,12,15]. In our study, the patient was an elderly man with PGA of 10 mm diameter localized in the upper part of the gastric body near the cardia.Predominantly, PGAs appear as a polypoid lesion or mass[10-12,16], but it may also present as flat lesion[9]or ulcer[10]. We reported an unusual case of PGA mimicking an SMT with an orifice on the surface of the lesion. Similarly, Yamamotoet al[9]reported a flat lesion with two openings at the greater curvature of the upper gastric body.Considering the possible deeper depth of the SMT-like lesion, we did not obtain its biopsy. But biopsy specimen from the orifice of the SMT may contribute to diagnosis.The performance of EUS is important in the diagnosis of an SMT-like lesion. To date,limited information is available on the EUS characteristics of the PGAs. Moreover,PGAs are usually located in the mucosal or submucosal layer in EUS. In the EUS by Yamamotoet al[9], multiple large cysts were found in the second and third layers and the intact fourth layer[9]. Whereas, in our case, EUS for the patient showed an isoechoic nodule with several cysts located in the submucosal layer.
The predisposing factors of PGAs have remained unclear. Eighteen cases (34%) of PGAs presented mainly with atrophic autoimmune gastritis (AIG), and they were also positive forH. pylorigastritis (30%). Moreover, only 3.8% cases have been reported with a normal gastric mucosa[8]. However, a controversy exists with regards to the background mucosa, where 22.4% of the PGAs developed with AIG background,while normal mucosa was seen in 35.8% cases[10]. The predominance of AIG in older women contributes to the frequent occurrence of PGA in these women[8]. In our study,the biopsy from the antrum indicated chronic non-atrophic gastritis without infection ofH. pylori; however, its relationship with the background mucosa and underlying mechanism need to be further explored.
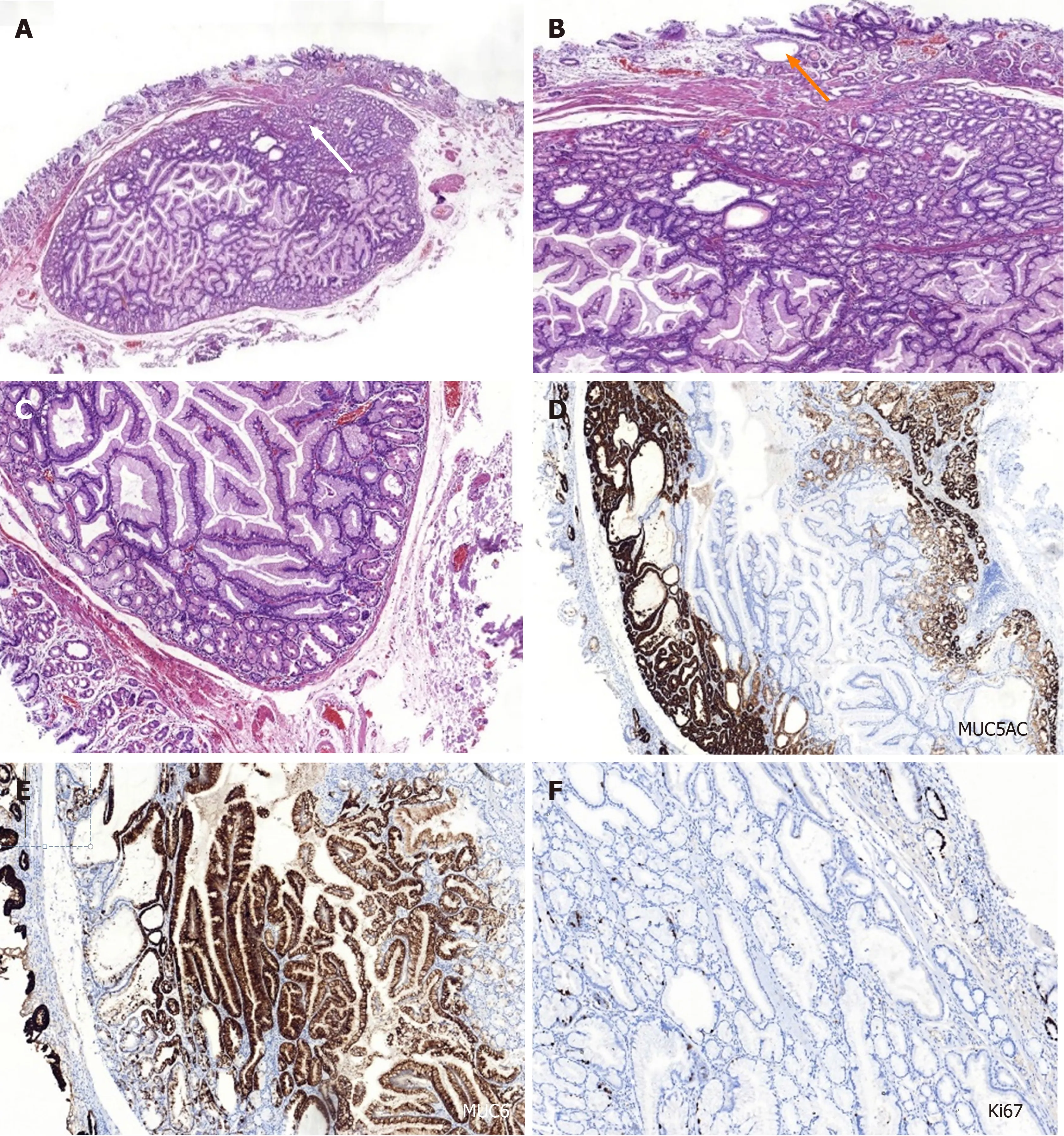
Figure 2 Histopathological and immunohistochemical findings of the pyloric gland adenoma. A-C: Hematoxylin and eosin staining. The submucosal layer shows presence of nodular-like lesions with clear boundaries and increasing number of glands in the lamina propria of the orifice (white arrow) (A; magnification: ×20). Some glandular cavity was irregular, with cystic expansion (orange arrow) and interstitial edema (B; magnification: × 200). The cuboidal or low columnar epithelial cells line the mucus-rich tubular glands in these lesions (C; magnification: × 200); D-F: Immunohistochemical staining. The glandular epithelial cells revealed strongly positive for mucin 5AC (D) and mucin 6 (E) and sparsely positive for Ki67 (F). Magnification: D-F: × 100. MUC5AC: Mucin 5AC; MUC 6: Mucin 6.
Furthermore, EUS revealed a few cysts within the equivalent echogenic mass located in the submucosal layer in our patient. Therefore, PGA should be distinguished from gastritis cystica profundal (GCP), which is a rare lesion of the stomach, characterized by polypoid cystic ectasia of benign gastric glands invading the submucosa. It associates with chronic inflammation and ischemia and is observed primarily in patients who have undergone gastrectomy[17]. The most frequent EUS feature of GCP was multiple anechoic cysts in the submucosal layer, as reported earlier[18,19]. However, we did not find any component of the GCP. There was an opening on the mucosal surface of the PGA that ought to be differentiated from the gastric ectopic pancreas. A dimple or umbilical opening can be observed in some heterotopic pancreases. Anechoic duct-like structure or rare cyst cavity structure can be detected within the hypoechoic mass located in the deep mucosal and submucosal layers by EUS[20]. The majority of heterotopic pancreas cases are located at the gastric antrum. No ectopic pancreatic tissues were identified in the resected specimen by ESD. Additionally, clinicians should differentiate it from other submucosal lesions such as the gastric neuroendocrine tumors[21]and SMT-like gastric adenocarcinoma[22,23].
Next, it was difficult to make an initial diagnosis of PGA due to the SMT-like appearance of the tumor, and an ESD was performed for final confirmation.Histopathological findings revealed mucus-rich pyloric glands lined with cuboidal or low columnar epithelial cells. Additionally, immunohistochemical staining was performed for MUC6 (specific for PGA) and MUC5AC (present in luminal foveolar type epithelium) to confirm the diagnosis of PGA. The gastric type adenoma that needed to be differentiated from PGA is foveolar-type adenoma, which is immunohistochemically positive for MUC5AC but negative for MUC6.
PGAs are considered at a high risk of malignant transformation[10,13], and have been divided into three categories: Viz, without conventional histologic dysplasia; lowgrade dysplasia (LGD); and high-grade dysplasia (HGD)[14]. In a recent multicenter clinicopathologic study with 67 gastric PGA cases, lesions with HGD or adenocarcinoma were found to have larger mean size (3.5 cm) than LGD cases (1.5 cm) (P< 0.001)[10]. They concluded that the risk of developing HGD or adenocarcinoma was directly associated with the size of the lesion, presence of AIG,tubulovillous architecture, and mixed type (co-expression of both MUC6 and MUC5AC in deeper glands with MUC6 expression ranging from 20% to > 90% of the neoplastic glands)[10]. An immunohistochemical analysis of the gastric PGAs indicated higher nuclear expression of p53 in PGAs with adenocarcinoma (82.1%) than those without adenocarcinoma (59.3%)[13], suggesting that nuclear p53 may correlate with high-risk PGAs. In our study, the PGA ought to be classified as mixed type. The relatively small diameter without expression of p53 may be responsible for the lack of conventional hyperplasia histologically. Regardless of the presence of hyperplasia, all PGAs represent at least LGD, even in cases without noticeable conventional histologic dysplasia[10]. Taken together, the patient in our study would need to be followed-up regularly.
Furthermore, in our case, the SMT-like lesion was located in the upper part of the gastric body. We performed ME-NBI and EUS for the patient, but failed to obtain the biopsy of the tumor. Moreover, we could not distinguish it from other SMTs and make an accurate preoperative diagnosis. Therefore, we subsequently performed the diagnostic ESD for this patient, with confirmed diagnosis using histopathological and IHC analysis. Additionally, the resected specimen did not show signs of malignancy.Although the overall recurrence rate of PGAs was very low[10], regular follow-up with periodic gastroscopic surveillance should be suggested.
CONCLUSION
We present a case of PGA with SMT-like appearance, located in the upper part of the gastric body. It poses difficulty in distinguishing from other submucosal lesions.Deeper biopsies using larger forceps or even EUS-guided fine needle aspiration may improve the clinical diagnosis. ESD was subsequently performed to confirm the final diagnosis. It is recommended that all PGAs be completely removed if possible,particularly when they are large or show high-grade features[10]. Clinicians and pathologists should pay close attention to PGAs owing to their potential to transform to adenocarcinoma. The patient needs to be followed up with regular gastroscopy observation.
ACKNOWLEDGEMENTS
We thank all the authors helping the writing and publication of this article.
 World Journal of Clinical Cases2020年11期
World Journal of Clinical Cases2020年11期
- World Journal of Clinical Cases的其它文章
- Tumor circulome in the liquid biopsies for digestive tract cancer diagnosis and prognosis
- Isoflavones and inflammatory bowel disease
- Cytapheresis for pyoderma gangrenosum associated with inflammatory bowel disease: A review of current status
- Altered physiology of mesenchymal stem cells in the pathogenesis of adolescent idiopathic scoliosis
- Association between liver targeted antiviral therapy in colorectal cancer and survival benefits: An appraisal
- Peroral endoscopic myotomy for management of gastrointestinal motility disorder
