Validation of the Arabic version of the Ocular Surface Disease lndex Questionnaire
May M. Bakkar, Ahmad K. El-Sharif , Mohammad Al Qadire
1Department of Allied Medical Sciences, Faculty of Applied Medical Sciences, Jordan University of Science and Technology, Irbid 22110, Jordan
2Department of English Language and Literature, Faculty of Arts and Humanities, Al Al-Bayt University, Mafraq 25113,Jordan
3Department of Adult Health, Faculty of Nursing, Al Al-Bayt University, Mafraq 25113, Jordan
4College of Nursing, Sultan Qaboos University, Muscat 123,Oman
Abstract
● KEYWORDS: OSDI questionnaire; dry eye disease; Arabic;validation; psychometrics analysis; Arabic version of the OSDI
INTRODUCTION
Dry eye disease (DED) is reported to be the most prevalent ocular condition that is encountered in ophthalmic clinics[1]. The Tear Film and Ocular Surface Dry Eye Workshop II (TFOS DEWS II) defines DED as “a multifactorial disease of the ocular surface characterized by a loss of homeostasis of the tear film, and accompanied by ocular symptoms, in which tear film instability and hyperosmolarity,ocular surface inflammation and damage, and neurosensory abnormalities play etiological roles”[2]. The reported global prevalence of DED ranges between 5% and 50%[3]and the disease was reported to affect daily life activities and work productivity in affected patients[4-5].
The risk factors for DED include contact lens wear, using video display unit (VDU), aging, female gender, menopause,some systemic diseases such as diabetes and ocular surface diseases such as keratoconus, meibomian gland dysfunction(MGD) and blepharitis[6-11].
DED can be diagnosed using the diagnostic methodology recommended in TFOS DEWS II[12]. It is based on initial triaging questions of differential diagnosis of DED, ocular history, risk factor assessment and presenting symptoms and signs that are combined with clinical findings[12]. However,clinical signs and symptoms are not linear in DED and vary with individuals with reported symptoms of DED and their impact on patient’s quality of life usually more profound than clinical findings[13-15].
Dry eye symptomology questionnaires are considered the key method to assess symptoms related to DED based on subjective response of the patient. Many questionnaires have been used in this regards such as the McMonnies Questionnaire, the Ocular Surface Disease Index (OSDI)[16], OSDI-6[17], Contact Lens Dry Eye Questionnaire-8 (CLDEQ-8)[18], Standard Patient Evaluation of Eye Dryness (SPEED)[19], the Ocular Comfort Index (OCI)[20], and the Dry Eye Questionnaire-5 (DEQ-5)[21].The OSDI questionnaire is a widely used tool for assessment of DED symptoms, where it has reported simplicity and acceptable test-retest repeatability, with high reliability and validity[16]. The questionnaire has yielded increasing popularity in clinical DED diagnosis, research and clinical trials[22-29]. It has also been translated and culturally adapted for usage in many languages including Chinese[30], Spanish[31], Japanese[32],Farsi[33], Brazilian, and Portuguese[34].
To date, there is no validated Arabic translated questionnaire in Arabic-speaking countries to assess dry eye symptomology.The aim of this study was to evaluate the reliability and validity of the Arabic version of the OSDI questionnaire. Using the validated version, it would be beneficial to use the tool for therapeutic and research purposes in Arabic speaking countries in the Middle East and North Africa (MENA) region.
SUBJECTS AND METHODS
Ethical Apporoval The study was part of a project to study the prevalence of DED symptomology among Jordanian population. Ethical approval to conduct the project was obtained from the Institutional Review Board (IRB) of Jordan University of Science and Technology. All prospective participants were given an information sheet about the study aims and requirements. If they agree, then they are given the questionnaire to complete. Participants were informed that their participation is voluntary. Also, they were informed that returning the completed questionnaire considered as an implicit consent on participation. The study protocol complied with the guidelines of the declaration of Helsinki.
Questionnaire The OSDI questionnaire was originally developed in 1997 by the Outcomes Research Group at Allergan Inc. (Irvin, California, USA). It includes 12-item designed to provide a rapid assessment of symptoms related to ocular irritation and DED for the previous week[16].
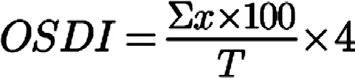
The questionnaire includes three subscales: ocular symptoms(items 1 to 5), vision related function (items 6 to 9) and environmental triggers (items 10 to 12, Table 1). The 12 items of the OSDI questionnaire are graded on a scale of 0 to 4,where 0 indicates none of the time; 1, some of the time; 2,half of the time; 3, most of the time; and 4, all of the time. For the items 6 to 12 the option “N/A” is also available. The total OSDI score is then calculated as recommended by Schiffmanet al[16]based on the following formula, OSDI={[sum of the scores for all questions answered (x)×100]/total number of questions answered (T)}×4.In this study, the validation process of the Arabic version of the OSDI questionnaire was accomplished over two phases as follows:Phase 1: Translation: Establishment of the Arabic version of the OSDI questionnaire.

Table 1 Questions in OSDI questionnaire used to screen dry eye symptoms in the study population
Edited by: http://atomurl.net/
The English version of the OSDI questionnaire was translated into Arabic in accordance and permission of its original publisher Allergan Inc. (Irvine, CA, USA). The translation process involved the following steps that is based on previous literature[32-37]:
1) Forward translation: the Arabic translation of the original English version of the OSDI questionnaire was obtained by an accredited translator in accordance, and with permission, of Allergan, Inc., Irvin, CA, USA. The identity of the accredited translator was anonymous to the researchers.
2) Cultural adaptation of the Arabic translation was conducted by a group of bi-lingual eye care professionals including three optometrists and two ophthalmologists. This step was performed to ensure scientific and cultural appropriateness of the Arabic translation, and to reveal if the questionnaire items are understandable to Arabic speaking patients.
3) Backward translation: the Arabic version of the questionnaire was then back-translated into English by a group of four English language (bilingual) linguists without medical background and without their mutual consultation. The linguists were blinded to the original English version of the questionnaire. The researchers collected the four backward translations, and they analysed the questionnaire by categorizing its content into translation units according to the original version of the questionnaire. These units represent a one coherent unit of meaning which can stand alone either as lexemes (words with form and meaning definable in the dictionary) such as index, eye, lens, dry; phrases such as experienced practitioner, limited responsibility, windy conditions, driving at night; clauses and sentences such as areas that are air conditioned; idiomatic expressions such as turn a blind eye to someone or something; or proverbs such as all’s well that ends well.
Then, each linguist qualitatively analysed and validated the other three translations done by the other three linguists through blind peer-reviewing process. Final, the researchers compared the four translations with the original English version of the questionnaire in order to identify the level of discrepancy in translation between the four translations on the one hand and the original one on the other hand. All instances of discrepancies were identified and examined meticulously as it is highlighted below.
4) Cognitive debriefing: after considering discrepancies,the pre-final Arabic version was forwarded to 30 Arabicspeaking participants to test their ability to understand and comprehend the questionnaire. Then, the pre-final version of the questionnaire underwent a second review by a focus group of 3 optometrists, and the final translation was used to test psychometric properties of the Arabic version of the questionnaire.
The level of discrepancy between the backward translations of the four linguists and the original English questionnaire was not significant in general. Almost all the four translators have managed to convey the intended equivalent translation of all items in the questionnaire. The discrepancy in these translations is found to affect both the grammar (syntactic component) and meaning (the semantic component).
All the participants enrolled in the cognitive debriefing step reported that they have not encountered any difficulty related to reading and responding to the questions in the Arabic translation of the questionnaire. After confirming that all questionnaire items are clear and easy to understand (as indicated through the results of forward-backward translation and cognitive debriefing), the final questionnaire was accredited without amendments; it is then named as ARB-OSDI.
Phase 2: Assessing the psychometric properties of the ARB-OSDI.Psychometric properties evaluation included internal consistency, scale homogeneity and test-retest reliability which were carried out to test the validity and reliability of the ARBOSDI questionnaire.
Study Design A cross-sectional survey design was used to test the reliability of the Arabic version of the OSDI questionnaire.
Sample and Settings Participants were recruited from the general non-clinical population. The participants were invited to participate in the study during community medical days in Jordan. Only native Arabic-speaking subjects who are above 18-year-old with normal cognitive ability were recruited in this prospective study. Participants with active ocular disease and recent ocular surgeries were excluded from the study.
Participants were invited to complete the ARB-OSDI questionnaire. If they agreed, then, they were given a print-out copy of an informed consent and the ARB-OSDI questionnaire to complete. Further demographic data were also collected from participants. These included: age, gender, education level and area of residence. The ARB-OSDI questionnaire was administered by trained Arabic-speaking interviewers who explained to the participants its purpose, method, and significance. Then, 30 participants were asked to re-fill the questionnaire for the second time within a period of 72h after the first completion. This time point was set to avoid changes in reported dry eye symptoms and to avert patients from recalling their first reported answers. Interviewer kept the first copy of the questionnaire and participant were asked to send the second completed copy as an email attachment or as a WhatsApp message according to their convenience.
Data Analysis Data were analysed using the statistical Package for Social Sciences (SPSS) software version 21 (SPSS,International Business Machine Corp. IBM, Chicago, IL, USA).Descriptive statistics were used to summarize sociodemographic characteristics of participants. Cronbach’s-α coefficient was used for reliability analysis of the scale. For the test and retest analysis, Intraclass correlation coefficient was used.
Construct validity of the scale was investigated by exploratory factor analysis and varimax rotation. The Kaiser-Meyer-Olkin(KMO) test was used to evaluate the relevance of the sample size. The value ofP<0.05 was accepted as an indication of being statistically significant.
RESULTS
A total of 200 participants completed the ARB-OSDI questionnaire. Among them, 114 (57%) were male. The average age of the study group was 31.21y (SD=13.2), range(18-75y). Demographic characteristics for all participants are presented in Table 2.
The mean OSDI score of the study population was 32(SD=21.56) with a range of 0 to 100. The mean scores in each sub-scale of ARB-OSDI are shown in Table 3.
Internal Consistency Items analysis of the ARB-OSDI subscales revealed an acceptable internal consistency as measured by Cronbach’s-α and item-to-scale correlation. For most items in the different subscales of the ARB-OSDI, the corrected item to scale (item to total) correlation coefficients ranged from 0.50-0.77, except for item 2 (eyes that feels gritty) (Table 4).This correction suggests that each item has a good correlation with the scale.For total scale, Cronbach’s-α was generally high for each scale (Table 5). Cronbach’s-α was also high for all items in each three subscales of the ARB-OSDI with a measured Chronbach-α ranged between 0.881 and 0.891 for the subscales about ocular symptoms (items 1 to 5), ranged between 0.887 and 0.890 for the subscales of the vision related functions(items 6 to 9), and for the subscales of environmental triggers to DED symptoms (items 10 to 12) ranged between 0.887 and 0.891.
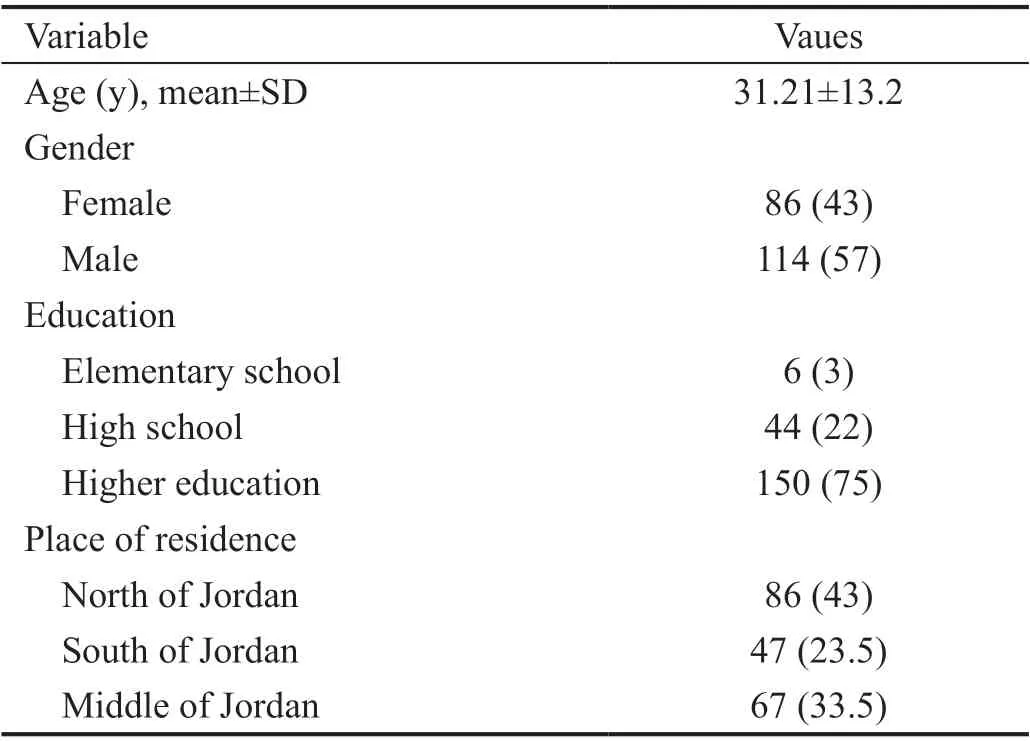
Table 2 Demographic characteristics of participants (n=200) n (%)

Table 3 Number of items in each scale and mean scores in each scale of ARB-OSDI
Test-retest Reliability To examine test-retest reliability of the questionnaire, Pearson correlation coefficient was calculated.The results show that the questionnaire has very good reliability withr=0.832,P<0.001.
Construct Validity An exploratory factorial analysis(Table 6) for the 12 items in the OSDI Arabic Scale was conducted. The Kaiser-Meyer-Olkin Measure confirmed the sample adequacy (KMO=0.85). Bartlett’s Test of Sphericity indicated that correlation between items were sufficiently large [χ2(66)=817.52,P<0.001]. Three factors (subscales) had eigenvalues over Kaiser’s criterion of 1 and they explain 68%of the variance.
DISCUSSION
The OSDI questionnaire is a valid and reliable instrument in quantifying subjective symptoms related to DED and the impact of the disease on visual functions[38]. The questionnaire is found to effectively discriminate between normal, mild, moderate and severe DED based on a composite disease severity score[16].In addition, the questionnaire has extensively been used in many populations-based studies to assess ocular symptoms associated with DED and other ocular surface conditions such as blepharitis, allergy and contact lens wear[30,39-40]. According to the TFOS DEWS II workshop, the OSDI questionnaire or in alternative the DEQ-5 were suggested as a part of the diagnostic criteria of DED to assess presence of dryness related symptoms[12].
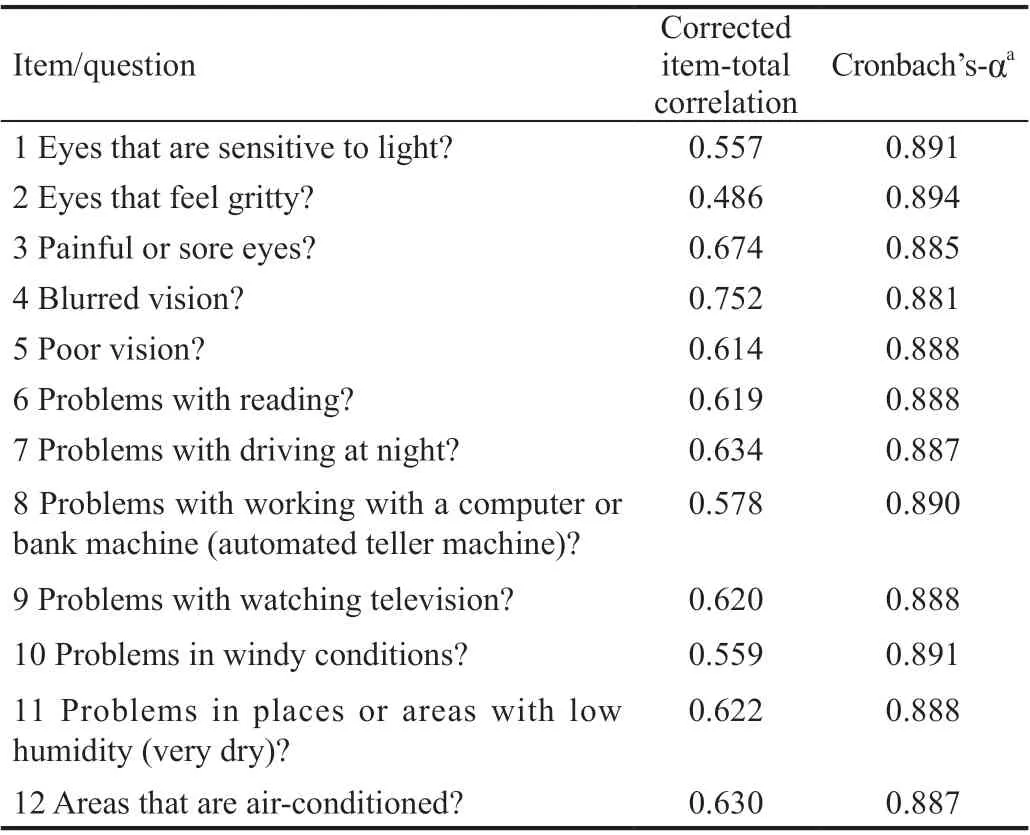
Table 4 Item analysis and internal consistency of the ARB-OSDI
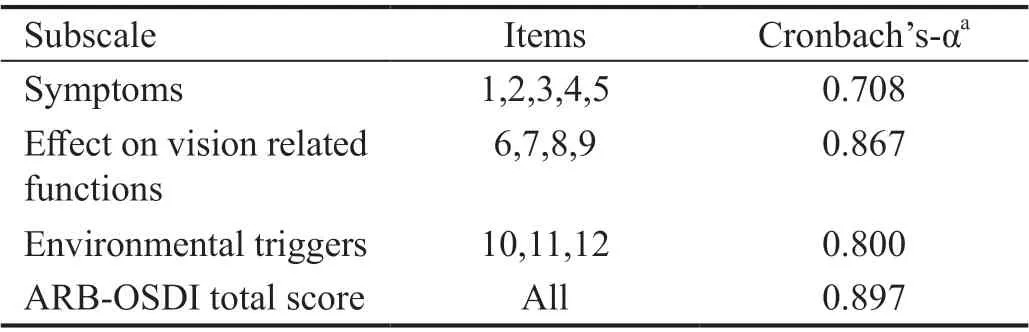
Table 5 Internal reliability of ARB-OSDI
Despite the expected high incidence of DED in Arabicspeaking countries, the prevalence of DED is not frequently studied in Arab communities in the MENA region. However,few reports have reported variable and noticeably high prevalence of DED in the region including Kingdom of Saudi Arabia (32.1%-93.2%)[41-43], Jordan (59%)[44], Palestine (69%)[45],and Lebanon (36.4%)[46]. In these reports, prevalence of DED was either studied based on severity of dryness symptoms using questionnaires[41,44,46]or a combination of symptoms and clinical assessment[42-43,45]. Nevertheless, it is found that all dryness symptoms questionnaires used in Arabic language have not been linguistically validated, or culturally adapted,prior to use in the studies.
The current study is the first endeavour to translate and validate the Arabic version of the OSDI questionnaire. The results demonstrate that the ARB-OSDI is of adequate reliability andvalidity to be used for the assessment of DED symptoms. The process of validation went through two main steps: a backforward translation into Arabic, and a validation that aimed to ensure that the questionnaire retains psychometric properties of the original OSDI among Arabic speaking population in Jordan.

Table 6 Rotated factor loadings for OSDI scale
The researchers found that the grammar (the syntactic component) of the original English text does not impose significant challenges to the translator. Thus, the accredited Arabic translation was straightforward and unproblematic.This allowed the translators to come up with an equivalent translation that is both grammatical and idiomatic. Hence, no significant difficulty or miscomprehension in this regard have been observed by the researchers. In few cases, the discrepancy between the four translators’ back translation was due to polysemy (the capacity for a word or phrase to have multiple meanings). For example, there is the case of the attributive adjective ‘poor’ (da3if) in ‘poor vision’ which is translated in the accredited translation as (da3if) and the noun phrase is(da3f fel naZar). When back-translated from Arabic to English,two of the translations involved the word ‘weakness’ instead of ‘poor’ (and the phrase was ‘weakness in vision’). A similar case was reported when the technical (highly-specialized) term‘sensitive’ in ‘sensitive to light’ (Hasasah lelDuu’) which was back-translated as ‘allergic’ by two translators.
In few cases, the relative discrepancy between the four translations and the original one is attributed to some required modifications in the syntactic structure of the phrase, or word class, because there is no one-to-one correspondence between some of the English and Arabic phrases or words in the accredited Arabic translation of the questionnaire. This was the case of the translation of the units ‘feel gritty’, ‘problems with your eyes’, ‘windy conditions’. The accredited translation has opted to modify the internal structure of the original English text. For example, the phrase ‘gritty eyes’ has been translated into Arabic as a larger phrase that involves a noun phrase ‘sand’and a prepositional phrase complement ‘in the eyes’ to make the phrase ‘sand in the eyes’ (ramlun fel 3ayn).
In all, such insignificant discrepancies were accounted for,and they were treated by the researchers while conducting the experiments by explaining to the respondents their meanings.The questionnaire distributors and data gatherers were notified and made aware of such discrepancies. They were told to clarify to the respondents the intentions of their questions and the sort of data they are expected to receive.
In this regard, the validated ARB-OSDI questionnaire demonstrated good psychometric properties including both high internal consistency and test-retest reliability. Internal consistency measures whether all items of the questionnaire measure the same characteristics[30]. The results showed that all the three subscales in the questionnaire; ocular symptoms,environmental triggers vision related functions had good internal consistency of the answers obtained and high correlation coefficient.
The corrected item to scale (item to total) correlation coefficients for most items in the different subscales of the ARB-OSDI showed acceptable level, except for item 2; eyes that feels gritty. This may indicate that this question item may require further clarification to respondents by interviewers or by adding clarifying sentence if self-completed by subjects.In conclusion, the ARB-OSDI shows consistent psychometric properties that makes it applicable to use in the assessment of DED in Arabic-speaking communities. Using the ARB-OSDI questionnaire could also be a rapid and instrumental tool in assessing and monitoring of subjective symptoms of DED in routine clinical practice and in future population-based studies in Arabic-speaking countries. Furthermore, the questionnaire is presented in Standard Arabic (AL-Fosha), a variety of Arabic that is highly esteemed by Arabs as it is the variety used in the Holy Qur’an, literature, and media. In addition, this variety is mutually understandable by the different speakers of regional Arabic dialects regardless of their social backgrounds.
On the other hand, this study has several limitations. First,discriminant validity of the ARB-OSDI was not tested. In future work, this could be possible by using the ARB-OSDI in two groups of subjects; a group with clinical diagnosis of DED and a group with no DED to test if the ARB-OSDI can discriminate between the two groups. Second, the study did not recognize what would be the cut-off value for suspecting DED. This would be possible if the ARB-OSDI applied in DED patients’ group beside other clinical tests such as TFBUT, osmolarity and corneal staining. Finally, the 72h for testing test-retest reliability might be short interval. However,this interval was considered short enough to avoid changes in ocular symptoms as the DED status of patients can change within days and long enough for patients not to remember the answers[47], relying on the fact that the OSDI was designed to provide assessment of dryness symptoms for the previous week[16].
ACKNOWLEDGEMENTS
We would like to thank all participants who agreed to participate in this study. The researcher would like to thank the anonymous translators at the translation company who were in charge of translating the English version of the OSDI to Arabic. In addition, the researchers are grateful to the four linguists from Al-AlBayt University who preferred to remain anonymous, for their time and effort in doing the backtranslation of the accredited translation to English.
Foundation:Supported by the Deanship of Research at Jordan University of Science and Technology.
Conflicts of Interest:Bakkar MM, None; El-Sharif AK,None; Al Qadire M, None.
 International Journal of Ophthalmology2021年10期
International Journal of Ophthalmology2021年10期
- International Journal of Ophthalmology的其它文章
- Exosomal miR-29b found in aqueous humour mediates calcium signaling in diabetic patients with cataract
- Intraluminal stenting versus external ligation of Ahmed glaucoma valve in prevention of postoperative hypotony
- Visual acuity after intravitreal ranibizumab with and without laser therapy in the treatment of macular edema due to branch retinal vein occlusion: a 12-month retrospective analysis
- Dexamethasone intravitreal implant (Ozurdex) in diabetic macular edema: real-world data versus clinical trials outcomes
- Comparative analysis of the clinical outcomes between wavefront-guided and conventional femtosecond LASlK in myopia and myopia astigmatism
- Reliability of the ocular trauma score for the predictability of traumatic and post-traumatic retinal detachment after open globe injury
