Unilateral orbital cellulitis after bilateral strabismus correction: a rare complication after strabismus surgery
Gui-Ou Zhang, Na-Min Li, Jian Zhou, Dan Hu, Yu-Sheng Wang, Chang-Mei Guo
Dear Editor,
I am Dr. Chang-Mei Guo, from the Department of Ophthalmology, Xijing Hospital, Fourth Military Medical University, Xi’an, Shaanxi Province, China. We write to present a case of unilateral orbital cellulitis after bilateral strabismus surgery. This study has been performed in accordance with the Declaration of Helsinki and written informed consent for publication of photographs was obtained from the patient.
The risk of postoperative infection after strabismus surgery is relatively low. The incidence of infections following strabismus surgery is estimated to be between 1/1100 to 1/1900 surgeries[1-2]. Orbital cellulitis is an extremely rare complication after strabismus surgery. It was reported that 12 cellulitis cases in a large series of 12 263 patients or approximately 1 per 1000 cases treated at the Columbia Presbyterian Hospital in New York[2]. We describe a case of a healthy male presented with orbital cellulitis after strabismus surgery, and cultures indicated methicillin-resistant staphylococcus aureus. Sensitive antibiotics was then switched according to results of drug sensitivity test. The patient showed improvement in visual acuity, pain, and extraocular motility. This is the first case of orbital cellulitis after strabismus surgery that we have encountered in the past 30y.

Figure 1 External photograph demonstrated the marked right eyelid swelling, the limited extraocular motility of the right eye on 6d after strabismus surgery.
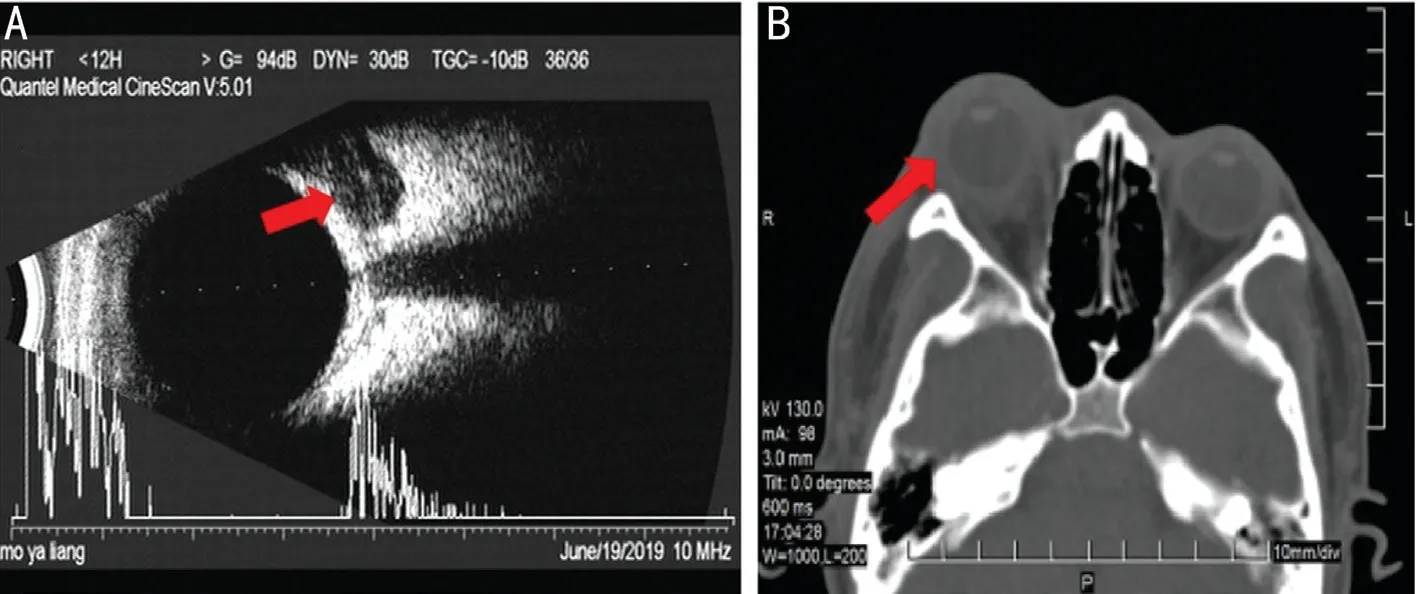
Figure 2 Orbital cellulitis was confirmed by imaging examination on 6d after strabismus surgery A: B-ultrasound indicated hypoechoic area in upper orbit of right eye, and periocular hypoechoic band is observed, indicating inflammation; B: Orbital axial computed tomography revealed right exophthalmos, and thickening of surrounding soft tissues.
A 17-year-old male presented to our hospital with a 10-year history of deviation of eye position and was diagnosed with concomitant exotropia and ametropia. The patient underwent bilateral lateral rectus recession and right medial rectus resection under local anesthesia. Two days before operation,the patients were treated with levofloxacin ophthalmic solution 4 times a day, and preoperatively the patient’s face was prepped with 0.45%-0.55% iodophor solution, and 5% povidone drops were instilled in both eyes for 90s. Parks conjunctival incisions were performed for binocular rectus operation, which were closed postoperatively with 3 stitches using 8-0 PGLA absorbable suture (HOLYCON, Nantong, China). Gatifloxacin eye gel was instilled in both eyes at the conclusion of surgery.The patient was using levofloxacin (q.i.d) and fluorometholone(t.i.d) eye drops in both eyes postoperatively. Then the patient was discharged upon normal results of eye examination 20h after the surgery. At 48h after the surgery, the patient presented with unexpected redness, swollen, pain, tearing, and increased secretion of right eye, accompanied with right-sided headache.At 72h, the patient developed hyperthermia (maximum body temperature 37.9℃) and deterioration of eye symptoms.Systemic cephalosporin treatment was administered at local clinic, and levofloxacin eye drop was increased to six times a day. After treatment, the body temperature was normalized yet eye symptoms were not alleviated. At the return visit on day 6 after the surgery, the corrected visual acuity was 20/40 in the right eye and 20/20 in the left eye. Intraocular pressure was 22 mm Hg in the right eye and 17 mm Hg in the left eye. External examination revealed severe erythema of right eyelid with skin hyperthermia, orbital hypertension, difficulty in lifting upper eyelid, and different degrees limitation of eye movement in all directions (Figure 1). Outward deviation of right eye was 10° at left eye fixation, and 30° outward of left eye at right eye fixation. Right conjunctiva presented with severe congestion and edema protruding from palpebral fissure, with large number of yellow secretions particularly on temporal side. The incision was closed, and 3 sutures were all in place. Other anterior segments and posterior segments were all normal. The patient was diagnosed as right orbital cellulitis after strabismus surgery and was admitted immediately.Routine blood test showed the leukocyte count was 9.87×109/L.B-scan ultrasound indicated hypoechoic area in upper orbit of right eye, and periocular hypoechoic band is observed,indicating inflammation (Figure 2A). Orbital computed tomography (CT) revealed right exophthalmos and thickening of surrounding soft tissues (Figure 2B). Conjunctival secretion culture and blood culture was performed. The patient was given levofloxacin eye drop per 1h, tobramycin dexamethasone eye dropsq.i.d, ceftriaxone sodiumi.v.(0.5 g,b.i.d), dexamethasonei.v.(5 mg,q.d), and compound mannitol.At the third day of admission, conjunctival secretion culture came back positive for methicillin-resistantStaphylococcus aureus(MRSA) while blood culture negative. The drug was intravenous then switched to moxifloxacin (0.4 g,q.d)according to result of drug sensitivity test. At the sixth day of admission, the symptoms were alleviated. The corrected visual acuity was 20/20 in both eyes, and the redness of right eyelid disappeared. Outward movement of right eye was 2 mm less than normal, while movement in other directions were normal.Outward deviation of right eye was 0° at left eye fixation, and 5° outward of left eye at right eye fixation. Right conjunctiva was slightly congested, and the cornea was transparent. The remaining anterior segments and posterior segments were normal. After discharge, the antibiotic therapy was switched to moxifloxacin oral administration 400 mg/d for 14d. The return visit at 3mo after surgery revealed inflammation absorption,both eyes were in normal position and normal ocular movement.Kivlin and Wilson[1]surveyed members of the American Association for Pediatric Ophthalmology and Strabismus(AAPOS) and reported the details of 25 cases of cellulitis in 1995. The infection usually appears within 5d after surgery[1,3],and the earliest time reported was one day after operation[4].There was a predominance of young children especially preschool age patients[1,4]. While Kimet al[3]reported a 76-yearold patient presented with orbital cellulitis after strabismus surgery, even developed choroidal detachment on postoperative day 9.Staphylococcus aureusis the most common pathogenic bacteria in conjunctival cultures[1,5]. The survey conducted by AAPOS in 1995 stated that 25 cases orbital cellulitis were all unilateral despite most of surgeries were bilateral, and excessive eye rubbing, unsuspected sinusitis, and poor hygiene were the possible predisposing factors for infection[1]. In this case, the patient was young and healthy without conjunctivitis,nasosinusitis, furuncle, or systemic infection, which excluded the pre-operative factors of infection. Since the surgery of this patient was appointed as the second one among all operations performed in that room on that day, and patients receiving operation before and after this patient had no signs of infection,which helps to exclude factors related to the environment of operation room. The vomica was located near the lateral rectus of the second eye without infection of the first eye, thus factors in relation to operation equipment can be excluded. During the operation, three extraocular muscles were involved, each seamed with an independent suture, and when we learned that the patient had orbital cellulitis after he returned for subsequent visit on the sixth day after the surgery, it was no longer possible to check the surgical suture at that time to confirm whether it was contaminated. A randomized controlled trial by Eustis and Rhodes[6]reported that the rate of bacterial contamination was 28% after strabismus surgery using sterile suture. This is probably due to the contact between suture and eyelash or skin during the surgery. The patient took a more than 9-hour bus’s trip to a hotel on the first day after operation, and he was unable to take medicine on time as directed. In addition,the patient did not perform basic hand hygiene during drug administration and repeatedly rubbed the operated eyes. At 48h after the surgery, the patient showed the clinical symptoms of cellulitis. So, we speculated that the cellulitis may be related to contaminated suture, the post-operative environment and poor compliance in taking medicine. However, it should be noted that MRSA was detected in conjunctival culture, which has strong toxicity and is commonly seen in hospital-acquired infection and community-acquired infection, so which suggesting exogenous sources as a potential etiologic contributor.
Dhrami-Gavaziet al[7]reported a healthy 3-year-old boy presented with bilateral orbital abscesses after strabismus surgery whose CT imaging stated that he had pansinusitis.Therefore, pre-operative evaluation is of great significance.It may be recommended to treat significant sinus disease with oral antibiotics prior to strabismus surgery or even postponement of surgery[7]. Moreover, enough attention should be paid to aseptic techniques during the procedure, with sufficient sterilization area around the eyes, and some authors have advocated routine administration of povidone-iodine in the fornix[8]. After the surgery, local anti-inflammation treatment should be administered, and patients with obvious orbital symptoms should be admitted to hospital for systemic antibiotic therapy until the condition becomes stable. If medical treatment turned out ineffective, along with development of vision loss, progressive exophthalmos or orbital apex syndrome, surgical interventions such as orbital decompression should be performed. Early diagnosis and active management are the key to preventing deterioration.
In conclusion, orbital cellulitis is an extremely rare and potentially vision- and life-threatening complication after strabismus surgery. Several techniques may be prudent for the strabismus surgeon to adopt to decrease the bacterial load and minimize the risk of infection. For patients with poor compliance or may be long exposure to environment with high risk of infection in the early postoperative period, days of hospitalization should be prolonged to guarantee postoperative drug administration and post-operative education should be strengthened. The surgeon should be encouraged to consider preoperative use of povidone-iodine on the operative field. Early diagnosis and active management are the key to preventing deterioration.
ACKNOWLEDGEMENTS
Foundations:Supported by the National Natural Science Foundation of China (No.81470655); Multidisciplinary Projects of the Subject Boosting Program of Xijing Hospital(No.XJZT19MDT12).
Conflicts of Interest:Zhang GO, None; Li NM, None; Zhou J, None; Hu D, None; Wang YS, None; Guo CM, None.
 International Journal of Ophthalmology2021年10期
International Journal of Ophthalmology2021年10期
- International Journal of Ophthalmology的其它文章
- Exosomal miR-29b found in aqueous humour mediates calcium signaling in diabetic patients with cataract
- Intraluminal stenting versus external ligation of Ahmed glaucoma valve in prevention of postoperative hypotony
- Visual acuity after intravitreal ranibizumab with and without laser therapy in the treatment of macular edema due to branch retinal vein occlusion: a 12-month retrospective analysis
- Dexamethasone intravitreal implant (Ozurdex) in diabetic macular edema: real-world data versus clinical trials outcomes
- Comparative analysis of the clinical outcomes between wavefront-guided and conventional femtosecond LASlK in myopia and myopia astigmatism
- Reliability of the ocular trauma score for the predictability of traumatic and post-traumatic retinal detachment after open globe injury
