Effects of scalp acupuncture plus acupuncture exercise therapy on walking ability in children with spastic cerebral palsy
ZHAO Yong (赵勇), JIN Bingxu (金炳旭), ZHAO Wenjian (招文健), CHENG Jixiang (程吉祥), HUANG Yinying (黄银英),GUO Jiankun (郭建坤), HAN Yu (韩玉), ZHANG Chuntao (张春涛), FU Jianmei (付建梅)
1 Nanhai Maternity and Child Hospital Affiliated to Guangzhou University of Chinese Medicine, Foshan 528200, China
2 Panyu Hospital of Chinese Medicine, Guangzhou, Guangdong Province, Guangzhou 511400, China
Abstract
Keywords: Acupuncture Therapy; Scalp Acupuncture; Scalp Stimulation Areas; Acupuncture Exercise Therapy; Cerebral Palsy;Myospasm; Movement Disorders; Child, Preschool
Cerebral palsy (CP) is a syndrome characterized by movement disorders caused by non-progressive brain injury in infants, of which spastic type accounts for about 60%[1]. The acquisition of walking ability,walking efficiency, and posture are the most concerning issues for the parents of children with CP,and it is also one of the main functions of self-care and social adaptation for CP children’s future life. The disease is difficult to treat and has a long recovery period, which brings on a heavy burden to society and family. In recent years, acupuncture therapy has been widely used in the clinical treatment of CP with satisfactory clinical effects[2-4]. In the 1970s,researchers put forward the concept of acupuncture exercise therapy (AET). It refers to performing acupuncture simultaneously with exercises to enhance the therapeutic effect. It has been widely used in the clinical treatment of pain and neurological diseases. Its efficacy in the rehabilitation of adults with stroke and spinal cord injury has already been confirmed[5].
At present, the treatment for children with CP is mainly based on acupuncture plus physical therapy[6].How to further improve the quality of life of CP children, decrease the family and social burden has always been the focus of the medical staff. In this study, AET was applied to the children with spastic CP,and the difference in efficacy between AET and conventional acupuncture was observed.
1 Clinical Materials
1.1 Diagnostic criteria
This study referred to the diagnostic criteria for spastic CP in theGuidelines for Rehabilitation of Cerebral Palsy in China(2015):Part One[1]. Central dyskinesia; abnormal motion posture and pattern such as tip foot and scissors gait; stretch hyperreflexia;increased muscle tone; with etiological evidence for CP, and/or cranial imaging evidence.
1.2 Inclusion criteria
Those who met the above diagnostic criteria; male or female; aged 3-6 years old; had no orthopedic surgery or injection of botulinum toxin type A treatment in the past 6 months; children and their guardians agreed to participate in this trial and signed informed consent.
1.3 Exclusion criteria
Those who had primary diseases involving cardiovascular system, liver, kidney, or hematopoietic system; those who were allergic constitution or allergic to multiple drugs; patients with epilepsy;those with coagulation disorders.
1.4 Elimination and dropout criteria
Those with poor compliance or presenting with new conditions and were unable to continue the treatment; dropped out due to the children’s or their parents’ reasons; had severe adverse reactions.
1.5 Statistical methods
All data were statistically analyzed by the SPSS version 21.0 statistical software. Age, the modified Ashworth scale (MAS) score, scores of dimensions D and E of the gross motor function measure (GMFM)scale, walking speed, and walking distance were quantitative data with normal distribution, thus expressed as mean ± standard deviation (±s). The pairedt-test was used for intra-group comparisons.The independent samplest-test was applied to the comparisons between the groups. Gender, spastic CP type, and gross motor function classification system(GMFCS) were qualitative data and described by frequency. The comparisons between the groups were analyzed by Chi-square test.P<0.05 was considered to indicate a statistical difference.
1.6 General data
A total of 60 CP children were enrolled in the Rehabilitation Department of Nanhai Maternity and Child Hospital Affiliated to Guangzhou University of Chinese Medicine. All the children were divided into a control group and an observation group by the random number table method, with 30 cases in each group. This study was reviewed and approved by the Ethics Committee of the Nanhai Maternity and Child Hospital Affiliated to Guangzhou University of Chinese Medicine (Approval No. 2019-01).
During the treatment, two cases in the observation group dropped out due to poor compliance during needle retention and unable to cooperate with the completion of the treadmill ambulation training.There were no adverse reactions presented during the treatment. There were no statistical differences in the general data between the two groups (P>0.05),indicating that the two groups were comparable(Table 1).

Group n Gender (case) Average age(Cerebral palsy type (case) GMFCS grade (case)images/BZ_7_1311_2835_1350_2881.png±s, year)Male Female Quadriplegia Diplegia Hemiplegia Ⅰ Ⅱ ⅢObservation 28 17 11 4.4±0.8 8 15 5 6 9 13 Control 30 19 11 4.2±0.9 9 15 6 7 9 14
2 Treatment Methods
2.1 Conventional rehabilitation treatment
The conventional rehabilitation treatment for CP here included conventional sports therapy[7]and treadmill ambulation training.
Treadmill ambulation training method (with or without body weight support): The training equipment was the HY-JZB-A1 electric weightsupported gait training system (Nanchang Tongjin Trade Co., Ltd., China). Children could watch walking animations during training. Pre-tests were taken before training. If the child could successfully do walking training for more than 10 min, and there was no serious abnormal posture during the training process, then weight support would not be necessary.A suspension device for weight support would be provided If the child could not tolerate or presented with severe abnormal postures during walking. In the beginning, the maximum weight support should be determined as that the child’s hip joints can extend and both lower limbs can support and then gradually decrease till no longer needed. The speed of the treadmill plate started from what the child could bear and gradually increased. The individualized training program was formulated according to the situation of the children. The training time started from 10 min and gradually increased to 20 min also according to the individual situation of the children. The training was performed once a day, 5 times a week, with 10 times as a treatment course and a 2-week interval between two courses, and 3 courses were given in total.
2.2 Scalp acupuncture therapy
Scalp acupuncture stimulation area (JIAO’s scalp acupuncture): Motor Area (bilateral lower limbs),Foot Motor Sensory Area, and Balance Area.
Methods:The child took a sitting position. The physician stood behind the child. After routine disinfection, spiral-handle needles of 0.30 mm in diameter and 40 mm in length were obliquely punctured at an angle of 30° between the needle tip and scalp. After insertion, as the needle tip reached the underlying galea aponeurotica, the needle body was flattened and inserted by 1.0-1.3 Cun in depth along the stimulation area. The needles were retained for 2 h. The treatment was performed once a day, 5 times a week, with 10 times as a treatment course and a 2-week interval between two courses,and 3 courses were given in total.
2.3 Grouping and intervention
Both groups were treated with the conventional rehabilitation treatment and scalp acupuncture mentioned above.
Children in the control group received the conventional rehabilitation treatment first, then the treadmill ambulation training, and finally the scalp acupuncture therapy. Children took a 30-minute rest after each treatment and then continued the next.
Children in the observation group received AET,which was, they were treated with the scalp acupuncture therapy first, and after 20 min of needle retention the conventional rehabilitation treatment,and then the treadmill ambulation training. All interventions were completed within 2 h of the scalp needle retention.
3 Observation of Results
3.1 Observation items
3.1.1 MAS score
The MAS score was used to evaluate the muscle tone of lower limbs. Grade 0 (0 point): no increase in the lower-limb muscle tone, and no resistance; grade 1 (1 point): slight increase in the lower-limb muscle tone, with a little resistance at the terminal end;grade 1+(2 points): slight increase in the lower-limb muscle tone, and stuck with slight resistance at the terminal end; grade 2 (3 points): mild increase in the lower-limb muscle tone, with resistance in most parts;grade 3 (4 points): moderate increase in the lowerlimb muscle tone, with resistance throughout the whole range; grade 4 (5 points): severe increase in the lower-limb muscle tone, with great resistance.
3.1.2 GMFM score
The GMFM scale was used to evaluate the standing ability of the children. The scale includes 88 items divided into 5 dimensions: A (recumbent position and turning over), B (sitting position), C (crawling and kneeling), D (standing position), and E (walking,running, and jumping). Dimension A scores 51 points,dimension B scores 60 points, dimension C scores 42 points, dimension D scores 39 points, and dimension E scores 72 points. In this study, only dimensions D and E were scored and converted according to the full score of 100. The higher the score of GMFM, the better the standing ability.
3.1.3 Walking speed measurement
The distance of children walking at their own preferred speed or as fast as possible within 1 min was measured, and the average value of 3 measurements for each time was taken. Walking speed = Walking distance ÷ 60.
3.1.4 Walking distance measurement
Six-minute walking distance measurement is the most common method for testing walking distance and walking endurance in children. During the measurement, a preset time of 6 min was set on the treadmill to measure the walking distance of children within 6 min. The above observation items were measured once before and after the treatment. The surveyors were senior rehabilitation therapists and were not aware of the treatment grouping.
3.2 Results
3.2.1 Comparison of the MAS score
Before treatment, there was no statistical difference in the MAS score between the two groups(P>0.05). After treatment, the MAS scores in both groups decreased (P<0.05), and the MAS score in the observation group was lower than that in the control group (P<0.05), (Table 2).
3.2.2 Comparison of the GMFM scores of dimensions D and E
Before treatment, there were no statistical differences in the scores of dimension D or dimension E in the GMFM scale between the two groups(P>0.05). After treatment, the scores of dimensions D and E in both groups increased (P<0.05) and were higher in the observation group than in the control group (P<0.05), (Table 3).
3.2.3 Comparison of the walking speed between the two groups
Before treatment, there was no statistical difference in the walking speed between the two groups (P>0.05). After treatment, the walking speed in both groups increased (P<0.05), and the walking speed in the observation group was higher than that in the control group (P<0.05), (Table 4).
3.2.4 Comparison of the 6 min walking distance
Before treatment, there was no statistical difference in the 6 min walking distance between the two groups (P>0.05). After treatment, the 6 min walking distance in both groups increased (P<0.05),and the 6 min walking distance in the observation group was longer than that in the control group(P<0.05), (Table 5).

Group n Before treatment After treatment t-value P-value Observation 28 2.29±0.60 1.57±0.57 8.216 0.000 Control 30 2.37±0.61 1.90±0.48 5.037 0.000 t-value 0.507 2.372 P-value 0.614 0.021

Group n Dimension D t-value P-value Dimension E t-value P-value Before treatment After treatment Before treatment After treatment Observation 28 60.77±19.54 75.38±16.42 9.453 0.000 41.82±17.22 53.89±15.07 7.841 0.000 Control 30 59.35±20.13 65.62±17.53 7.332 0.000 40.45±18.76 44.89±16.48 5.912 0.000 t-value 0.272 2.184 0.289 2.165 P-value 0.786 0.033 0.773 0.034

Group n Before treatment After treatment t-value P-value Observation 28 0.51±0.19 0.61±0.15 10.140 0.000 Control 30 0.50±0.21 0.52±0.18 9.826 0.000 t-value 0.189 2.060 P-value 0.850 0.044
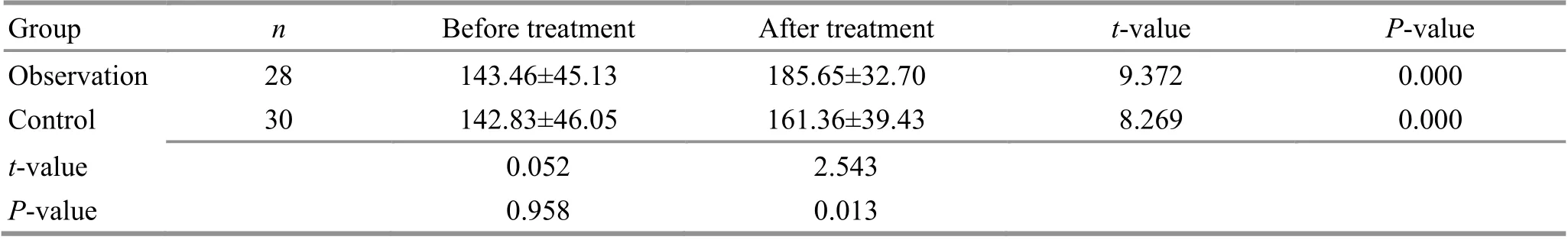
Group n Before treatment After treatment t-value P-value Observation 28 143.46±45.13 185.65±32.70 9.372 0.000 Control 30 142.83±46.05 161.36±39.43 8.269 0.000 t-value 0.052 2.543 P-value 0.958 0.013
4 Discussion
The typical clinical feature of spastic CP is increased muscle tone. The increased muscle tone reduces normal muscle strength and at the same time restricts the free movement of joints, thus affecting normal motor function[8]. Increased muscle tone will simultaneously inhibit the coordination of synergistic and antagonistic muscles during exercise, reduce the ability to maintain and control the body posture during exercise, thus affecting balance control and causing movement disorders[9-10]. Therefore, reducing the muscle tone of spastic muscle groups, improving the muscle strength of related muscle groups, and improving the movement range of restricted joints are the basis for improving the walking ability of children with CP. Previous studies have shown that acupuncture can effectively reduce the muscle tone of the spastic muscle group in children with CP and improve the movement range of the joints[11-13], thus improving the walking ability of children.
Treadmill ambulation training, also known as active treadmill walking training, can carry out in a weight-support or non-weight-support manner according to the condition of children. This training method is commonly used in walking training for CP children. With the exercise plate rotation, the child steps subconsciously, which is a compulsive active movement, making the hip joints passively overstretched. And this traction will increase the contraction of the hip flexors, making the limbs swing forward. The conveyor belt continuously moves backward, forcing the child to step forward,completing the contraction of the anti-gravity muscles, and flexing the hips, knees, and ankles. For children with poor balance ability, a suspension holding device can be used to take part of the child’s body weight, so as to assist the child in an upright standing state and avoid falling, thereby enhancing the sense of security and self-confidence of the child during walking. A domestic study showed that treadmill training (with or without weight support)could improve the walking speed of children with spastic diplegia[14]. Foreign studies have shown that weight loss treadmill walking training can effectively reduce neuromuscular abnormalities in children with CP, control spasms, and continuously improve posture stability[15-16]. This study also confirmed to a certain extent that treadmill walking training can improve the walking ability of children with CP.
The core concept of AET is to conduct active or passive movements of the patient’s limbs simultaneously with acupuncture (or during needle manipulation after insertion of needles), in order to enhance the curative effect. This therapy integrates traditional acupuncture, Tuina (Chinese therapeutic massage), and psychology, and combines with modern sports rehabilitation and anatomy, boasting the characteristics of integrated traditional Chinese and Western medicines, and its clinical efficacy is often better than that of acupuncture or exercise therapy alone[17]. Since acupuncture at the relevant points (areas) of the head does not affect the movement of the limbs, the AET formed by scalp acupuncture combined with the movement of the affected limb is most widely used in the rehabilitation of limb movement disorders caused by pain,neurological and orthopedic diseases in adults[18], and is also suitable for the rehabilitation of motor disorders in children. Scalp acupuncture combined with treadmill ambulation training is one kind of AET and is suitable for the rehabilitation of children with poor compliance during walking training.
The results of this study showed that after 3 courses of treatment, the MAS score of the spastic CP children in both groups was decreased, and the GMFM score, walking speed, and walking distance were increased, indicating that dysmyotonia, walking ability, and balance ability of the children in both groups were improved. It is suggested that conventional rehabilitation training combined with scalp acupuncture and partial weight-support gait training can effectively improve the gross motor function of children with CP, which is consistent with previous studies[10,19-20]. In this study, the improvements of each item in the observation group treated with AET were more significant than those in the control group treated with non-simultaneous scalp acupuncture and treadmill ambulation training,which confirms that AET has a specific curative effect.We believe that the mechanism of this specific curative effect may be related to the following four factors. First, as the meridian Qi provoked by scalp acupuncture circulates along the course of meridians and reaches the disease location, it combines with the meridian Qi provoked by topical exercises,synergistically playing a therapeutic role and achieving the purpose of treatment. Second, in the process of scalp acupuncture treatment, the lower limbs perform active movements, which can easily promote the meridian Qi provoked by scalp acupuncture to reach the disease location, so as to achieve the purpose of “the arrival of Qi (Deqi)breeding effectiveness”. Third, the scalp acupuncture areas are located in the projection sites of the cerebral motor cortex on the body surface.Acupuncture and walking training performed simultaneously are more conducive to the activation of motor cortex function and the repair of injury.Fourth, during the walking training process on the activity platform, the children can watch the build-in animation of children’s walking movements on the training equipment, which may synchronously let the children develop motion imagination, activating mirror neurons and strengthening the efficacy of AET.
In summary, compared with non-simultaneous scalp acupuncture and treadmill ambulation training,AET, the simultaneous combination of scalp
acupuncture and treadmill ambulation training, can better improve the walking ability of children with spastic CP and improve muscle tone. Meanwhile, this therapy is easy to operate, without expensive rehabilitation equipment, and the simultaneous operation of these two therapies can shorten the treatment time, which is worth further studies and promotion. Furthermore, animal experimental studies can help explore the possible mechanism.
Conflict of Interest
The authors declare that there is no potential conflict of interest in this article.
Acknowledgments
This work was supported by the Special Fund Project of Guangdong Provincial Inheritance and Development of Traditional Chinese Medicine (广东省传承发展中医药事业专项资金项目, No. 20201339).
Statement of Informed Consent
Informed consent was obtained from the guardians of the recruited children in this study.
Received: 31 August 2021/Accepted: 18 October 2021
 Journal of Acupuncture and Tuina Science2022年3期
Journal of Acupuncture and Tuina Science2022年3期
- Journal of Acupuncture and Tuina Science的其它文章
- Effects of electroacupuncture pretreatment on motor function and cerebral blood flow in MCAO model rats
- Effect of moxibustion on N-methyl-D-aspartate receptor subtype 2B expression in hippocampus of rheumatoid arthritis model rats
- Therapeutic efficacy and safety rating of Tui-Pushing chest-back manipulation for children with cough variant asthma
- Clinical observation on moxibustion at Baihui (GV20)plus Tuina for children with postnasal drip syndrome
- Clinical study of warm needling moxibustion combined with entecavir in the treatment of compensated cirrhosis due to chronic hepatitis B
- Clinical study of warm needling moxibustion plus intra-articular injection of sodium hyaluronate for hip involvement in ankylosing spondylitis
