1例中毒性表皮坏死松解症继发脓毒血症的药物治疗及监护
陈昆 陈虹 方洁
摘 要 目的:探讨临床藥师在中毒性表皮坏死松解症继发脓毒血症患者的治疗方案制定、治疗药物监测、皮肤护理、不良反应防治中的作用和价值。方法:临床药师通过ALEND评分识别可疑致敏药物为布洛芬,根据患者病原学检查结果,运用治疗药物监测协助临床医师优化抗感染治疗方案,同时对患者皮肤护理、药物不良反应等进行药学监护。结果:治疗后患者感染得到有效控制,临床症状好转,且未发生药物不良反应。结论:临床药师对患者实施全程药学监护,可优化治疗方案,及时发现和评估可能出现的严重药品不良反应,提高了药物治疗的安全性和有效性。
关键词 中毒性表皮坏死松解症 脓毒血症 临床药师 药学监护
中图分类号:R758.25 文献标志码:B 文章编号:1006-1533(2022)09-0058-05
引用本文 陈昆, 陈虹, 方洁. 1例中毒性表皮坏死松解症继发脓毒血症的药物治疗及监护[J]. 上海医药, 2022, 43(9): 58-62.
Pharmaceutical care of a case of toxic epidermal necrolysis secondary to sepsis
CHEN Kun1,2, CHEN Hong3, FANG Jie2
(1. Department of Pharmacy, the Hospital affiliated to Southwest Medical University, Luzhou 646000, China; 2. Department of Pharmacy, Ruijin Hospital affiliated to School of Medicine, Shanghai Jiao Tong University, Shanghai 200025, China; 3. Department of Pulmonary and Critical Care Medicine, Ruijin Hospital, School of Medicine, Shanghai Jiao Tong University, Shanghai 200025, China)
ABSTRACT Objective: To explore the role and value of clinical pharmacists in the formulation and adjustment of treatment plans, drug monitoring, skin care and prevention of adverse reactions for toxic epidermal necrolysis secondary to sepsis. Methods: Clinical pharmacists identified ibuprofen as the suspected sensitizer by ALEND score, used therapeutic drug monitoring to assist clinicians to optimize the anti-infective treatment plan based on the results of etiological examination and the characteristics of PK/PD of antibiotics in burn patients and also conducted pharmaceutical care for patients’ skin care, adverse drug reactions and so on. Results: Her infection was effectively controlled, clinical symptoms were improved, and no adverse drug reactions occurred after treatment. Conclusion: The whole-course pharmaceutical care provided by clinical pharmacists for patients with toxic epidermal necrolysis can optimize the treatment plan, timely detect and evaluate possible serious adverse drug reactions, and improve the safety and effectiveness of drug treatment.
KEY WORDS toxic epidermal necrolysis; sepsis; clinical pharmacist; pharmaceutical care
中毒性表皮坏死松解症(toxic epidermal necrolysis,TEN)和史提芬-强生症候群(Stevens-Johnson syndrome,SJS)是一种严重皮肤不良反应,以表皮剥脱和黏膜损害为特征,表皮剥脱面积≥30%时被诊断为TEN[1]。70%~90%的SJS/TEN由药物导致,最常见的致敏药物包括抗生素、别嘌醇、非甾体类抗炎药和抗癫痫药[2]。SJS/TEN急性期可累及多个脏器,出现肾衰竭、肠道病变、肺部病变和脓毒血症等一系并发症,如不及时救治可能危及患者生命[1]。本研究记录临床药师对1例TEN继发脓毒血症患者治疗全程的药学监护,探讨临床药师在TEN治疗中的作用与价值。
1 病例资料
患者,女性,25岁,体重50 kg。因“确诊亚急性皮肤红斑狼疮17年,发热皮疹3月余,加重5 d”入院。患者院外长期口服醋酸泼尼松片10 mg qd、沙利度胺50 mg qn,期间病情稳定。2020年5月5日,患者受凉后发热,伴寒战,Tmax 39.3 ℃,自行服用布洛芬后体温可降至正常,但随后再次发热。2020年5月8日自行加用奥司他韦、阿莫西林后,晚上出现躯干处红斑、瘙痒,次日加重蔓延至面部、颈部、四肢,伴颜面部浮肿,至当地医院住院治疗后皮疹好转。但2020年7月23日患者出现全身多发水疱,疱液澄清,予以甲泼尼龙60 mg qd ivgtt、丙种球蛋白20 g治疗后,水疱逐渐结痂干涸,但反复出现新发水疱。2020年8月14日起水疱明显增多,融合,表皮剥脱。2020年8月18日患者再次发热,Tmax 38.6 ℃,病情危重,于8月19日转入我院皮肤科。
查体:颜面、躯干、四肢广泛皮肤剥脱,尼氏征阳性,剥脱面积>80%,其上有大面积糜烂面,糜烂面大量渗出,部分为脓性分泌物。生殖器及口腔黏膜可见糜烂。
辅助检查:白细胞计数(white blood cell count,WBC)3.95×109/L,中性粒细胞(neutrophil,NEUT)% 71.7%;C-反应蛋白(CRP)35 mg/L;降钙素原(PCT)0.31 ng/mL;自身免疫抗体检测示:ANA颗粒型1∶2 560,抗Chrom抗体(+),抗SSA抗体(+),抗SSB抗体(+),抗SmRNP抗体(+),抗RNP抗体(±),抗RNP A抗体(±);肝功能、肾功能未见异常。
诊断:中毒性表皮坏死松解症;亚急性皮肤红斑狼疮。
2 治疗经过
3 讨论
3.1 可疑致敏药物的识别
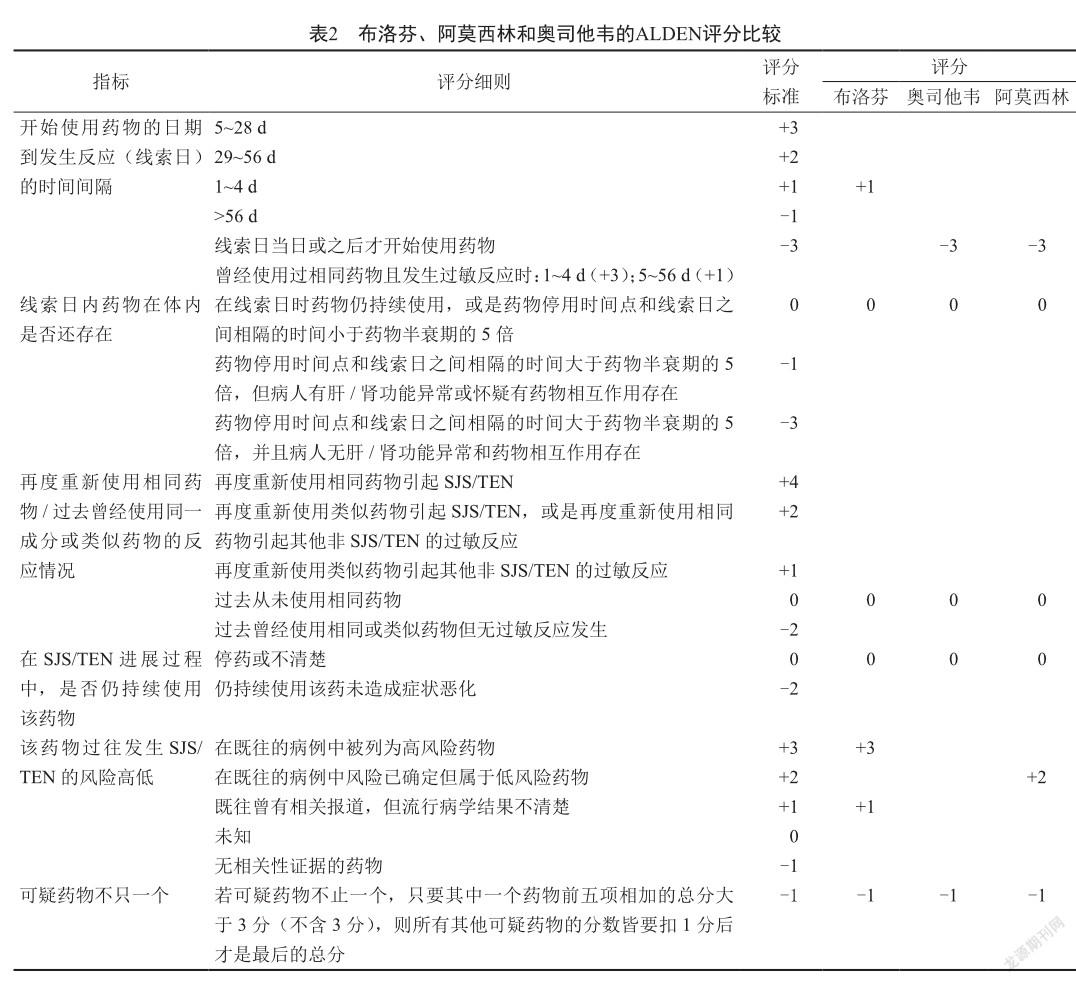
目前,TEN的治疗还没有标准化的诊疗指南,早期对可疑致敏药物的识别和及时停药是治疗的首要步骤和关键点,临床主要使用因果关系评估工具(causality assessment tools,CAT)来评估药物与严重皮肤不良反应的关联性,例如ALDEN评分[3]、Liverpool评分[4]和 Naranjo评分[5]。其中ALDEN评分是完全针对SJS或TEN所设计,是目前识别TEN致敏药物的最佳评估工具。临床药师详细询问患者过敏史用药史后,初步推断出可能导致该患者发生TEN的藥物为布洛芬、阿莫西林、奥司他韦,分别对上述3种药物进行ALDEN评分:布洛芬4分(可能)、阿莫西林-2分(极不可能)、奥司他韦-4分(极不可能)(表2)。
3.2 抗感染治疗方案的制定与调整
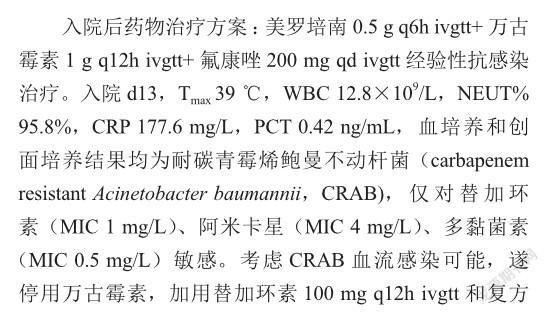
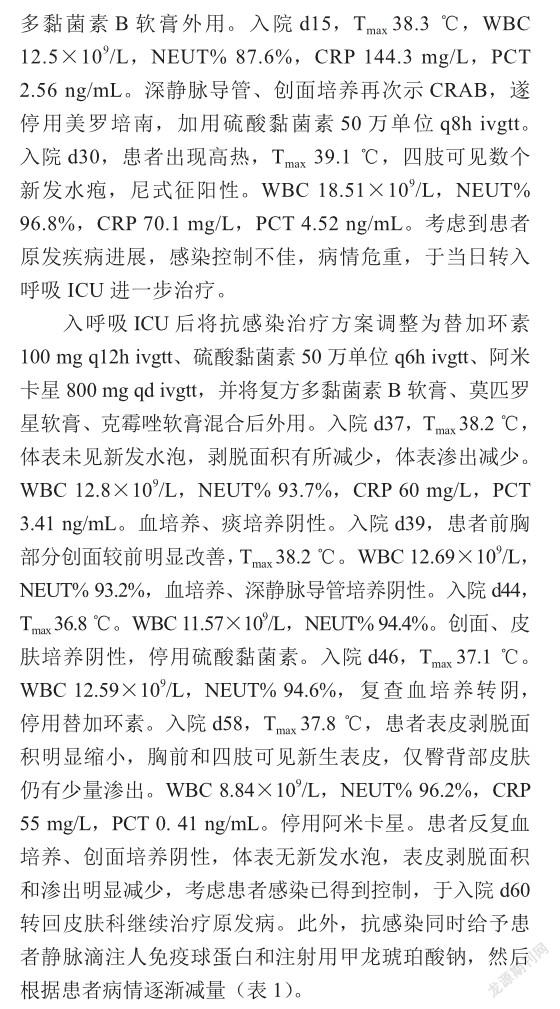
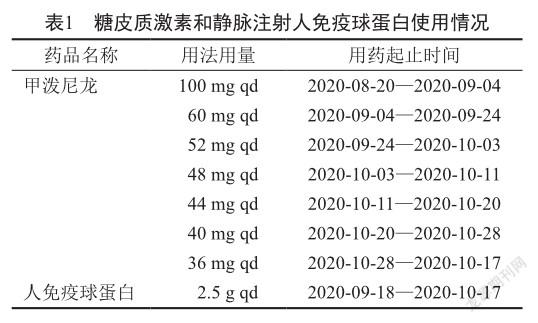
脓毒血症是导致TEN患者死亡的主要原因,最常见的病原体为金黄色葡萄球菌、铜绿假单胞菌,其次是鲍曼不动杆菌以及肠杆菌科细菌,当怀疑发生脓毒血症时,应尽早地给予对肠杆菌科细菌以及皮肤培养的病原菌有活性的抗菌药物治疗[6-7]。由于TEN疾病本身可能引起肝肾功能不全,而且TEN患者大面积表皮剥脱后大量体液和蛋白的流失造成血流动力学不稳定,都会对抗菌药物的PK/PD产生较大影响,增加了抗感染治疗的难度。
目前对CRAB的治疗通常以多黏菌素或者替加环素为基础的联合方案。替加环素在皮肤和软组织中浓度和渗透性高,且替加环素可以调节基质金属蛋白酶-9(matrix metalloproteinase-9,MMP-9)促进烧伤患者伤口愈合,对于多药耐药(multidrug resistant,MDR)或广泛耐药(extensively drug resistant,XDR)革兰阴性菌引起的严重感染患者,建议替加环素的给药方案为200 mg负荷剂量,100 mg q12h维持治疗[8-9]。Chung等[10]发现多黏菌素E联合阿米卡星能有效清除幸存的鲍曼不动杆菌,有助于其所致严重感染的治疗。因此予以硫酸黏菌素50万单位q8h ivgtt+替加环素100 mg q12h ivgtt+阿米卡星600 mg qd ivgtt抗感染。但硫酸黏菌素联合阿米卡星可能会增加肾毒性,因此对于硫酸黏菌素剂量的选择和治疗药物监测就显得极为重要。硫酸黏菌素仅在我国批准上市,说明书推荐首剂100万单位,之后50万单位,q8~12h维持,目前缺乏重症感染或严重烧伤患者的用药经验。Bode-B?ger等[11]报道了1例严重烧伤继发脓毒血症的患者,给予多黏菌素E甲磺酸钠(colistimethate sodium,CMS)负荷剂量9百万单位,维持剂量3百万单位(≈90 mg CBA)q8h,两天后测得多黏菌素E峰谷浓度分别为0.91 mg/L和0.48 mg/L,未能达到有效的血药浓度。Lee等[12]关于烧伤患者的群体药动学研究表明,烧伤患者多黏菌素E的半衰期(6.6 h)明显短于其他重症患者。此外,该患者入院后始终处于肾功能亢进状态,肌酐清除率基本维持在150 mL/min以上,因此临床药师建议增加硫酸黏菌素给药频次为50万单位q6h ivgtt。同时对硫酸黏菌素进行治疗药物监测,在给药后第4天测得硫酸黏菌素谷、峰浓度分别为1.20 mg/L和3.70 mg/L,估算平均稳态血浆浓度(average steady-state concentration,ACSS)为2.45 mg/L,达到《多黏菌素优化使用国际共识指南》推荐的2 mg/L的PK/PD靶值[13]。经过上述抗感染治疗后,患者于1周后血培养转阴,2周后创面培养转阴,体温也较前降低,各项感染指标正常,前胸和四肢新生表皮达90%,背部、臀部由于长期受压,新生表皮较少,但渗出明显减少,说明患者的感染得到了有效控制。
3.3 皮肤的管理
TEN患者存在广泛的表皮剥脱和黏膜损伤,导致皮肤黏膜屏障功能受损,因此皮肤的消毒和促进创面修复也是治疗的关键。因此,前期给予患者盐酸利多卡因0.6 g+硫酸庆大霉素48万U+地塞米松磷酸钠注射液50 mg+0.9%氯化钠注射液500 mL bid湿敷创面,可以起到消毒、抗炎、止痛的作用。后期由于创面多次培养出CRAB和真菌,于是先使用洗必泰对创面、外阴、腋窝等部位消毒,然后将复方多黏菌素B软膏、莫匹罗星软膏、克霉唑软膏混合后均匀涂抹于油纱上,再将凡士林纱布敷于创面或者使用银离子敷料外敷。凡士林纱布可以增强屏障功能,减少水分流失并促进皮肤再生[14]。而多项研究[15-16]表明银离子敷料具有很强的抗菌活性,能够促进表皮再生,而且使用方便安全,每2~3 d更换1次即可,与凡士林纱布交替使用效果佳。
參考文献
[1] Duong TA, Valeyrie-Allanore L, Wolkenstein PP, et al. Severe cutaneous adverse reactions to drugs[J]. Lancet, 2017, 390(10106): 1996-2011.
[2] Bettuzzi T, Ingen-Housz-Oro S, Purtillo CC, et al. Changing spectrum of suspected drugs of epidermal necrolysis: a World Health Organization pharmacovigilance database analysis from 1997-2020[J]. J Am Acad Dermatol, 2021, 85(6): 1581-1584.
[3] Sassolas B, Haddad C, Mockenhaupt M, et al. ALDEN, an algorithm for assessment of drug causality in Stevens-Johnson syndrome and toxic epidermal necrolysis: comparison with case-control analysis[J]. Clin Pharmacol Ther, 2010, 88(1): 60-68.
[4] Gallagher RM, Kirkham JJ, Mason JR, et al. Development and inter-rater reliability of the Liverpool adverse drug reaction causality assessment tool[J]. PLoS One, 2011, 6(12): e28096.
[5] Naranjo CA, Busto U, Sellers EM, et al. A method for estimating the probability of adverse drug reactions[J]. Clin Pharmacol Ther, 1981, 30(2): 239-245.
[6] Creamer D, Walsh SA, Dziewulski P, et al. UK guidelines for the management of Stevens-Johnson syndrome/toxic epidermal necrolysis in adults 2016[J]. J Plast Reconstr Aesthet Surg, 2016, 69(6): e119-e153.
[7] Koh HK, Chai ZT, Tay HW, et al. Risk factors and diagnostic markers of bacteraemia in Stevens-Johnson syndrome and toxic epidermal necrolysis: a cohort study of 176 patients[J]. J Am Acad Dermatol, 2019, 81(3): 686-693.
[8] Simonetti O, Cirioni O, Lucarini G, et al. Tigecycline accelerates staphylococcal-infected burn wound healing through matrix metalloproteinase-9 modulation[J]. J Antimicrob Chemother, 2012, 67(1): 191-201.
[9] De Pascale G, Montini L, Pennisi M, et al. High dose tigecycline in critically ill patients with severe infections due to multidrug-resistant bacteria[J]. Crit Care, 2014, 18(3): R90.
[10] Chung ES, Ko KS. Eradication of persister cells of Acinetobacter baumannii through combination of colistin and amikacin antibiotics[J]. J Antimicrob Chemother, 2019, 74(5): 1277-1283.
[11] Bode-B?ger SM, Schopp B, Tr?ger U, et al. Intravenous colistin in a patient with serious burns and borderline syndrome: the benefits of therapeutic drug monitoring[J]. Int J Antimicrob Agents, 2013, 42(4): 357-360.
[12] Lee J, Han S, Jeon S, et al. Population pharmacokinetic analysis of colistin in burn patients[J]. Antimicrob Agents Chemother, 2013, 57(5): 2141-2146.
[13] Tsuji BT, Pogue JM, Zavascki AP, et al. International Consensus Guidelines for the Optimal Use of the Polymyxins: endorsed by the American College of Clinical Pharmacy(ACCP), European Society of Clinical Microbiology and Infectious Diseases (ESCMID), Infectious Diseases Society of America (IDSA), International Society for Anti-infective Pharmacology (ISAP), Society of Critical Care Medicine(SCCM), and Society of Infectious Diseases Pharmacists(SIDP)[J]. Pharmacotherapy, 2019, 39(1): 10-39.
[14] Seminario-Vidal L, Kroshinsky D, Malachowski SJ, et al. Society of Dermatology Hospitalists supportive care guidelines for the management of Stevens-Johnson syndrome/ toxic epidermal necrolysis in adults[J]. J Am Acad Dermatol, 2020, 82(6): 1553-1567.
[15] Haung SH, Wu SH, Sun IF, et al. AQUACEL Ag in the treatment of toxic epidermal necrolysis (TEN)[J]. Burns, 2008, 34(1): 63-66.
[16] Smith SD, Dodds A, Dixit S, et al. Role of nanocrystalline silver dressings in the management of toxic epidermal necrolysis (TEN) and TEN/Stevens-Johnson syndrome overlap[J]. Australas J Dermatol, 2015, 56(4): 298-302.