Efficacy of mild moxibustion combined with surgery for meniscal injury and its effect on TGF-β1 and PDGF levels in the fluid of knee joint
LU Fangqin (陆芳芹), MAO Zhijuan (茅志娟), CHEN Lijuan (陈丽娟), CHEN Xuexian (陈学先)
Nantong Hospital of Traditional Chinese Medicine, Jiangsu Province, Nantong 226001, China
Abstract
Keywords: Moxibustion Therapy; Moxa Stick Moxibustion; Arthroscopic Surgery; Meniscus Injuries; Pain Measurement;Visual Analog Scale; Transforming Growth Factor Beta1; Platelet-derived Growth Factor
Meniscal injury is a common type of knee sports injury that occurs mostly in physically active people,such as young adults and athletes. It is characterized by knee pain, swelling, popping, interlocking, and limited motion[1]. The blood supply to the meniscus is poor,most injuries heal poorly, and conservative treatment is not very effective, so early surgical treatment is often recommended[2]. With the development of arthroscopic technology and the improvement of biomaterials,arthroscopic meniscal repair has gradually become the mainstream procedure for treating meniscal injuries. It can achieve the purpose of repairing the injury while preserving the integrity of the meniscus as much as possible, with the advantages of less trauma, shorter operation time, and faster postoperative recovery[3-4].However, postoperative complications such as intra-articular blood accumulation, swelling, and joint pain are still inevitable and can lead to muscle wasting atrophy, which affects functional recovery and surgical outcomes[5]. In this study, we used mild moxibustion combined with arthroscopic meniscal repair to treat meniscal injury and observed its efficacy and effects on transforming growth factor (TGF)-β1 and plateletderived growth factor (PDGF) in the fluid of knee joint.
1 Clinical Materials
1.1 Diagnostic criteria
Referred to the diagnostic criteria for meniscal injury inFractures and Joint Injuries[6]. In an acute injury, there is a history of trauma, and in chronic injury, there is less trauma; the joint is swollen and painful when moving,with popping and interlocking of the knee; grinding and compression test (+), McMurray’s test (+); magnetic resonance imaging (MRI) examination suggests meniscal injury.
Meniscal injury can be graded according to MRI findings[6]. Grade Ⅰ: MRI suggests spot or high nodular signal in the meniscus; Grade Ⅱ: MRI suggests high linear signal; Grade Ⅲ: MRI examination suggests rupture of the fibrocartilaginous plate in the meniscus.
1.2 Inclusion criteria
Met the above diagnostic criteria, and the meniscus injury was a grade Ⅲ injury; aged 20-60 years;proposed to be hospitalized for arthroscopic meniscal repair, and the site of meniscal injury was in the red zone or red-white junction zone; unilateral injury;provided informed consent.
1.3 Exclusion criteria
Those with a previous history of knee surgery or significant knee osteoarthritis; women during pregnancy or lactation; those with severe cardiovascular diseases.
1.4 Criteria for elimination and dropout
Those who developed postoperative infections; those who used other treatments without authorization;those who voluntarily withdrew from the trial; those who had serious adverse events; and those with incomplete information.
1.5 Statistical analysis
Data analysis was performed using the SPSS version 18.0 software. Counting data were expressed as the number of cases or percentages, and the Chi-square test was used. Categorial data were tested by rank-sum test. Measurement data conforming to normality and homogentity of variance were expressed as mean ±standard deviation (±s), and pairedt-test was used for intra-group comparisons and unpairedt-test for inter-group comparisons. Non-parametric test was used for measurement data not conforming to normality or homogeneity of variance.P<0.05 was considered a statistically significant difference.
1.6 General data
Ninety-eight patients with a meniscal injury admitted to the hospital between June 2017 and June 2019 were selected. The SPSS version 18.0 software was used to generate a random number table, and sealed envelopes were used to divide the patients into the surgery group or the moxibustion plus surgery group, with 49 cases in each group. There was no statistically significant difference between the two groups in gender, age, or site of disease (P>0.05). See Table 1.
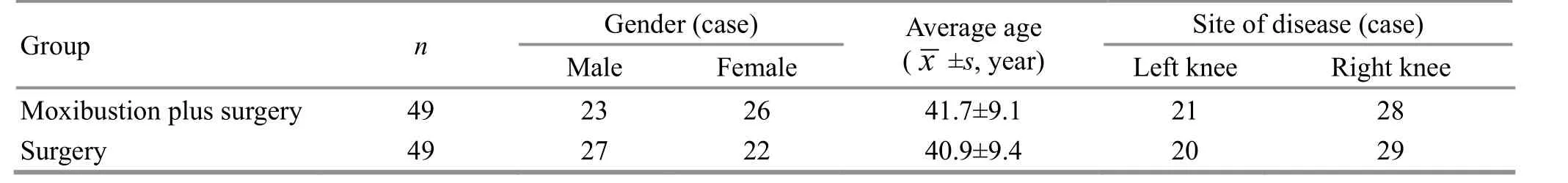
Table 1. Baseline characteristics of the two groups
2 Treatment Methods
2.1 Surgery group
The meniscal repair was performed using the arthroscopy technique. After admission,electrocardiogram, blood routine, biochemical, and coagulation tests were given to exclude contraindications to surgery. After spinal and epidural analgesia, the patient was placed in the horizontal position, and a pneumatic tourniquet was tied to the upper mid-thigh of the affected limb. The standard anterolateral and anteromedial approaches to the knee were taken, with the articular lens placed on one side of the approach and the probe hook and other instruments used on the other side. The intra-articular free body was removed, the hyperplastic synovial tissue was cleared, the site and type of meniscal injury were carefully explored and clarified, the torn edge of the meniscus was trimmed, and the best approach was selected for suturing. The joint cavity was irrigated to avoid residual debris and free bodies in the joint cavity,and the incision was sutured and wrapped with an elastic bandage with pressure for 24 h. Intermittent cold compresses were applied for 30 min/time twice a day for one week after the surgery, and functional exercises were taken.
2.2 Moxibustion plus surgery group
Patients in this group received mild moxibustion in addition to the same surgery used in the surgery group.Mild moxibustion was taken 48 h after the surgery.
Points: Bilateral Xuehai (SP10), Yanglingquan (GB34),and Taichong (LR3).
Method: Moxibustion was performed with pure moxa sticks of 1.8 cm in diameter and 20 cm in length(Nanyang Wolong Han Medical Moxa Factory, China).The patient was in a supine position with the skin below the mid-thigh exposed. After lighting the moxa sticks,the physician aligned the moxa sticks to the selected points and applied mild moxibustion 2-3 cm away from the skin, taking care to avoid surgical incisions and dressings. Moxibustion was performed until the skin flushed with local warmth and no burning pain. Each selected point was treated in sequence for about 10 min. Moxibustion was taken 3 times a week (once every other day or 3 d) for a total of 4 weeks.
3 Observation of Therapeutic Efficacy
3.1 Observation items
3.1.1 Lysholm score
In both groups, the Lysholm score, including limp,need for support, interlocking, pain, swelling, difficulty going up and down stairs, and difficulty squatting, was evaluated before and after treatment. The score ranges from 0 to 100 points, with higher score indicating better knee function[7].
3.1.2 Visual analog scale (VAS) score
The VAS was used to evaluate the pain level before and after treatment in both groups. The score ranges from 0 to 10 points, with 0 indicating no pain and 10 indicating the most severe pain[8].
3.1.3 Mobility of the affected knee
Before and after treatment, the maximum angle of active flexion and extension of the affected knee was measured using a joint goniometer in both groups.
3.1.4 Healing of meniscus
Three months after the surgery, MRI was performed on the affected knee in both groups. The contrast agent was injected into the joint cavity, and the patient was asked to perform several active knee flexion and extension movements, followed by oblique sagittal and oblique coronal scans of the meniscus. The meniscus was considered to be fully healed if no high signal of contrast agent entry was seen in the whole meniscus on the image; partially healed if only a high signal of contrast agent was visible inside the meniscus but did not penetrate the whole meniscus; not healed if a high signal of contrast agent was seen inside the meniscus and penetrated the whole meniscus[9].
3.1.5 TGF-β1 and PDGF levels in the fluid of the affected knee joint
Before and after treatment, 3 mL of knee joint fluid was extracted, and the levels of TGF-β1 and PDGF were measured by enzyme-linked immuno- sorbent assay.
3.2 Results
3.2.1 Comparison of the Lysholm and VAS scores
Before treatment, there was no statistically significant difference in the Lysholm or VAS scores between the two groups (P>0.05). After treatment, the Lysholm scores increased in both groups (P<0.05), and the VAS scores decreased in both groups (P<0.05). The Lysholm score was higher in the moxibustion plus surgery group than in the surgery group, and the VAS score was lower in the moxibustion plus surgery group than in the surgery group. The differences between groups in both scores were statistically significant(P<0.05). See Table 2.
Table 2. Comparison of the Lysholm and VAS scores between the two groups ( ±s, point)

Table 2. Comparison of the Lysholm and VAS scores between the two groups ( ±s, point)
Note: VAS=Visual analog scale; compared with the same group before treatment, 1) P<0.05; compared with the surgery group after treatment, 2) P<0.05
Group n Lysholm score VAS score Before treatment After treatment Before treatment After treatment Moxibustion plus surgery 49 54.57±8.74 90.65±3.731)2) 6.07±1.47 1.05±0.581)2)Surgery 49 55.14±8.80 85.86±4.011) 6.34±1.36 1.86±0.741)
3.2.2 Comparison of the mobility of the affected knee
Before treatment, there was no statistically significant difference in the mobility of the affected knee between the two groups (P>0.05). After treatment,the mobility of the affected knee increased in both groups (P<0.05), and it was greater in the moxibustion plus surgery group than in the surgery group (P<0.05).See Table 3.
3.2.3 Comparisons of the TGF-β1 and PDGF levels in the fluid of the affected knee joint
Before treatment, there were no statistically significant differences in the TGF-β1 or PDGF levels in the fluid of the affected knee joint between the two groups (P>0.05). After treatment, the TGF-β1 and PDGF levels in the fluid of the affected knee joint increased in both groups (P<0.05), and they were higher in the moxibustion plus surgery group than in the surgery group (P<0.05). See Table 4.
3.2.4 Comparison of the healing of meniscus
The healing of the meniscus in the moxibustion plus surgery group was significantly better than that in the surgery group at the follow-up visit 3 months after surgery (P<0.05). See Table 5.
Table 3. Comparison of the mobility of the affected knee between the two groups ( ±s, °)
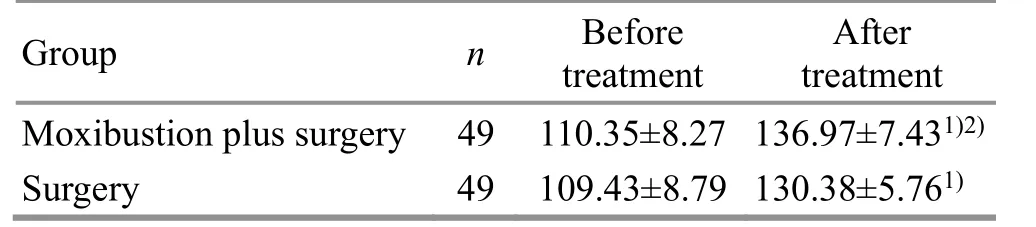
Table 3. Comparison of the mobility of the affected knee between the two groups ( ±s, °)
Note: Compared with the same group before treatment,1) P<0.05; compared with the surgery group after treatment,2) P<0.05
Group n Before treatment After treatment Moxibustion plus surgery 49 110.35±8.27 136.97±7.431)2)Surgery 49 109.43±8.79 130.38±5.761)
Table 4. Comparison of the TGF-β1 and PDGF levels in the fluid of the affected knee joint between the two groups ( ±s, pg/mL)

Table 4. Comparison of the TGF-β1 and PDGF levels in the fluid of the affected knee joint between the two groups ( ±s, pg/mL)
Note: TGF-β1=Transforming growth factor β1; PDGF=Platelet-derived growth factor; compared with the same group before treatment, 1) P<0.05; compared with the surgery group after treatment, 2) P<0.05
Group n TGF-β1 PDGF Before treatment After treatment Before treatment After treatment Moxibustion plus surgery 49 14.39±2.62 25.56±5.731)2) 201.16±29.96 326.33±54.801)2)Surgery 49 14.77±3.14 18.45±4.711) 199.25±32.05 245.29±34.811)
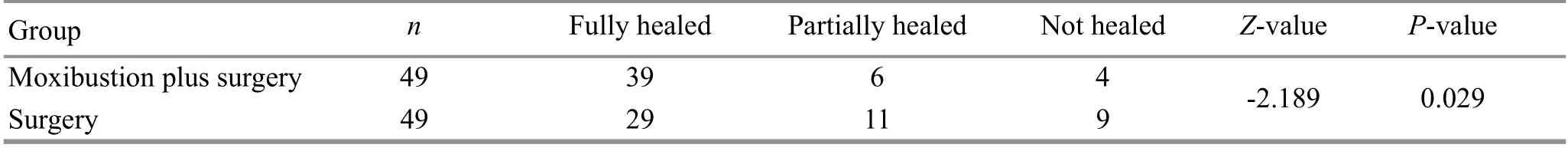
Table 5. Comparison of the healing of meniscus between the two groups (case)
4 Discussion
Arthroscopic knee surgery can suture and repair the injured meniscus, largely avoiding the adverse consequences of meniscectomy, and has a more prominent efficacy for meniscal blood flow zone (red zone and red-white zone) injury[10-11]; while the bloodless meniscus zone (white zone) has almost no blood supply, the poor healing ability after an injury,and no value of suture and repair treatment[12], so this study only included patients with red zone or red-white zone injury of the meniscus.
Meniscal injury belongs to the category of “tendon injury” and “knee paralysis” in traditional Chinese medicine. External violence and chronic strain damage the knee meridians and veins, and blood vessels are paralyzed, causing pain when they do not pass; in addition, surgery can directly damage blood vessels and veins, resulting in blood stasis outside the veins and causing local swelling and pain. Therefore, after arthroscopic knee surgery for the meniscus injury, local symptoms of Qi stagnation and blood stasis are often seen[13], and treatment should be based on the principle of moving Qi and blood and reducing swelling and pain.
Mild moxibustion is a type of suspended moxibustion,suitable for the treatment of tendon injury and knee paralysis due to Qi stagnation and blood stasis. Xuehai(SP10), Yanglingquan (GB34), and Taichong (LR3) were selected for this study. Xuehai (SP10) can invigorate and nourish blood, and is good at treating all blood disorders, and it is close to the knee joint, so it can unblock the Qi and blood circulation in the knee and play a proximal treatment role[14]. Yanglingquan (GB34)is the He-Sea Point of the Gallbladder Meridian and the Lower He-Sea Point of the gallbladder, able to soothe the liver and regulate Qi, and unblock meridians. This point is also the Confluence of Tendons of the Eight Confluent Points, which can strengthen tendons and bones, unblock meridians, and relieve acute pain.Taichong (LR3) is the Shu-Stream Point and Yuan-Primary Point of the Liver Meridian. It can circulate Qi, clear the liver, harmonize blood, resolve blood stasis, and relieve pain. Together, these points work to relax tendons and unblock meridians, circulate Qi, resolve blood stasis, and relieve swelling and pain[15-16].
TGF-β1 and PDGF play an important role in meniscal healing. TGF-β1 is a pleiotropic proteoglycan that has the ability to promote angiogenesis, chemotaxis of fibroblasts and macrophages, and stimulate collagen deposition. It promotes extracellular matrix synthesis and further protects the extracellular matrix by downregulating matrix metalloproteinase 2, matrix metalloproteinase 1, and other extracellular matrix degrading enzymes[17]. Studies have shown that TGF-β1 promotes the proliferation of meniscal cells,chemotactic migration of various neoplastic cells to the area of injury, and stimulates the production of type Ⅰcollagen and aminoglycan by meniscal cells to promote chondrogenesis and healing of meniscal injury[18-19]. In a sheep meniscal injury model, TGF-β1 was found to be elevated early in the injury and peaked at 2 weeks, and then gradually decreased over time, suggesting that TGF-β1 may be involved in the repair of meniscal tissue early in the injury and may be associated with a higher healing rate in the acute phase of meniscal injury than in the chronic phase[20]. PDGF is a chemokine that promotes mitosis, cell proliferation, and angiogenesis.In meniscal injury, PDGF increases infiltration of traumatic fibroblasts and inflammatory cells, has chemotactic effects on chondrocytes and mesenchymal stem cells, promotes the proliferation of meniscal chondrocytes, and enhances their ability to synthesize extracellular matrix, prompting rapid granulation tissue formation to accelerate injury healing[21]. It also stimulates endothelial cell growth and promotes capillary angiogenesis in the damaged area[22].Platelet-rich plasma contains high concentrations of TGF-β1 and PDGF, which have the functions of promoting osteogenesis, accelerating bone healing and soft tissue repair, significantly shortening the healing time of meniscal injury, and improving healing quality.Thus, they have become a hot spot for trauma healing research at home and abroad[23].
The results of this study showed that after treatment,the Lysholm score increased and the VAS score decreased in both groups, and the Lysholm score in the moxibustion plus surgery group was higher than that in the surgery group, and the VAS score in the moxibustion plus surgery group was lower than that in the surgery group; after treatment, the mobility of the affected knee increased in both groups, and the mobility of the affected knee in the moxibustion plus surgery group was greater than that in the surgery group; 3 months after the surgery, the healing of the meniscus in the moxibustion plus surgery group was significantly better than that in the surgery group. Compared with the pre-treatment period, the levels of TGF-β1 and PDGF in the fluid of the affected knee joint increased in both groups after treatment, and the levels of both indexes were higher in the moxibustion plus surgery group than in the surgery group. These results suggest that the addition of mild moxibustion to surgical treatment can further improve the function and mobility of the knee joint, relieve pain, and promote meniscal healing in patients with meniscal injury, which may be related to the up-regulation of TGF-β1 and PDGF levels in the fluid of the affected knee joint.
Conflict of Interest
The authors declare that there is no potential conflict of interest in this article.
Acknowledgments
There was no project fund support for this study.
Statement of Informed Consent
Informed consent was obtained from all individual participants.
Received: 11 January 2021/Accepted: 11 March 2021
 Journal of Acupuncture and Tuina Science2022年5期
Journal of Acupuncture and Tuina Science2022年5期
- Journal of Acupuncture and Tuina Science的其它文章
- Clinical study on tube moxibustion plus point-toward-point needling method in treating refractory facial paralysis
- Effects of acupuncture plus medication on hippocampus SIRT1 and FOXO3a expression, MDA content, and SOD activity of rats with Alzheimer disease
- Improvement effect of acupuncture on locomotor function in Parkinson disease via regulating gut microbiota and inhibiting inflammatory factor release
- Effects of Mo-Rubbing abdomen manipulation on glucose metabolism and inflammatory factors in rats with type 2 diabetes mellitus
- Observation on the therapeutic efficacy of Tuina plus “three-bridge” exercise for non-specific low back pain
- Influence of herbal cake-partitioned moxibustion on lumbar functions and inflammatory factors in patients with lumbar disc herniation due to kidney deficiency and blood stasis
