Clinical profile of febrile encephalopathy patients at a tertiary care hospital in India: A retrospective study
Sanjeev Sengupta ,Ashish Kumar Shukla ,Kunal Kishore ,Jitesh Goel ,Amlan Ghosh
Department of Cardiology1,Department of Medicine2,Department of Neurology3,Command Hospital,Eastern Command,Kolkata-700064,West Bengal,India
ABSTRACT Objective:To investigate demography,etiology,and clinical profile and to analyze the outcomes of patients presenting with febrile encephalopathy at a tertiary care center in Eastern India.Methods:This retrospective,observational study included a total of 50 patients (>18 years) who presented with fever and encephalopathy.All patients underwent blood analysis;culture test for blood,urine,sputum,cerebrospinal fluid,and other body fluids;chest and abdominal ultrasonography;neuroimaging;polymerase chain reaction test,and other relevant tests as and when applicable.Results:The mean age of all enrolled patients was (58.0±16.0) years with male to female ratio of 1.27∶1.Viral encephalitis was diagnosed in 16 (32%) patients,sepsis-associated encephalitis in 14 (28%),bacterial meningoencephalitis in 8 (16%) and tuberculosis meningoencephalitis in 5 (10%).The mean hospital stay was 10 (4,17) days.At 6-month follow-up,10 (20%) patients died,10 (20%) patients recovered with sequelae (cognitive impairment,critical care neuropathy,etc.),and 30 (60%) patients recovered without sequelae.A statistically significant association was noted between Glasgow Coma Scale (<8) and mortality rate (P=0.02).Conclusions: Primary central nervous system infection is the most frequent etiology of febrile encephalopathy and viral encephalitis is the most common etiological cause.Accurate,systematic,timely diagnosis and management are prime factors to reduce mortality and morbidity.
KEYWORDS: Encephalopathy;Fever;Acute syndrome;Etiology;Infection
1.Introduction
Febrile encephalopathy is a clinical condition characterized by short febrile illnesses and is accompanied or followed by an altered mental state and impaired cognition,attention,and orientation.It is a frequently encountered condition in emergency and outpatient departments and should be treated as a medical emergency[1].Febrile encephalopathy has a wide range of clinical presentations and requires careful consideration of differential diagnoses.It is crucial to promptly distinguish these disorders as accurate diagnosis and treatment greatly affect morbidity and mortality rates[2-4].
Febrile encephalopathy could be a result of pathogenic factors that directly affect the central nervous system (infective or noninfective causes),or various systemic complications (hypoglycemia,hyperpyrexia,hypotension,hypoxia,or electrolyte imbalance).Globally,infection of the central nervous system is the primary cause of febrile encephalopathy which can be caused either by viruses,bacteria,or parasites[1].The etiological and clinical characteristics of febrile encephalopathy significantly differ depending on the geographic location and season[3].In a study involving Indian pediatric patients (age <18 years),viral encephalitis (~40%) was the most common cause of acute febrile encephalopathy followed by bacterial meningitis (33.8%),tubercular meningitis (7.9%),and cerebral malaria (5.2%)[5].Emergency healthcare providers must make precise diagnoses and promptly administer appropriate antimicrobials and supplementary medications to patients in need.At the same time,they must strive to avoid subjecting patients who do not have these conditions to unnecessary,invasive,and timeconsuming testing and treatment.Therefore,the present study was designed to examine demography,etiology,and clinical profile and to analyze the outcomes of febrile encephalopathy in Eastern Indian patients.
2.Patients and methods
2.1.Study design and population
This was a retrospective,observational study conducted at a tertiary care center in India from February 2021 to July 2022.
2.2.Inclusion and exclusion criteria
Patients (>18 years) who presented with fever and encephalopathy were enrolled in the study.The patients with known brain spaceoccupying lesions,meningitis post-head injuries,post-neurosurgery encephalitis,post-surgical sepsis,postpartum sepsis,and hypoxicischemic encephalopathy were excluded.
2.3.Clinical investigation
All patients underwent following examinations: i) complete blood count,serum electrolytes,liver function test,renal function test,and blood culture test;ii) urine analysis -routine urine examination and urine culture sensitivity,and urine metanephrines test;iii) serological tests -malarial parasites immunochromatographic,Widal,dengue serology,leptospira,and scrub typhus tests;iv) sputum examination -for acid-fast bacillus stain,ZN stain,fungal stain,and Mycobacterium tuberculosis GeneXpert;v) cerebrospinal fluid (CSF) examination -for cytology,biochemistry,malignant cells,staining for acid-fast bacillus,ZN,KOH mount,acanthamoeba;vi) neuroimaging -magnetic resonance imaging,and non-contrast computed tomography of the head;vii) electroencephalogram;and viii) PCR panel for meningitis,viral encephalitis,and autoimmune encephalitis.
2.4.Statistical analysis
The sample size was calculated using the following formula:
whereN=sample size;Zα=Zvalue or standard score (At α [error]=5% and 95% confidence intervalZvalue becomes 1.96);p=incidence rate of disease in the subject population (from available data,the incidence of febrile encephalopathy ranges from 1.4%-5.4 % among ICU admissions) and in this study,we consideredpto be 3.4% (mean of 1.4 and 5.4);and e=precision rate as 5.
Data were analyzed using SPSS (version 27.0;SPSS Inc.,Chicago,IL,USA) and Graph Pad Prism version 5.Data were expressed as mean and standard deviation for numerical variables and count/percentages for categorical variables.Chi-square test was used.P-value <0.05 was considered statistically significant.
3.Results
A total of 50 patients were included (Figure 1).
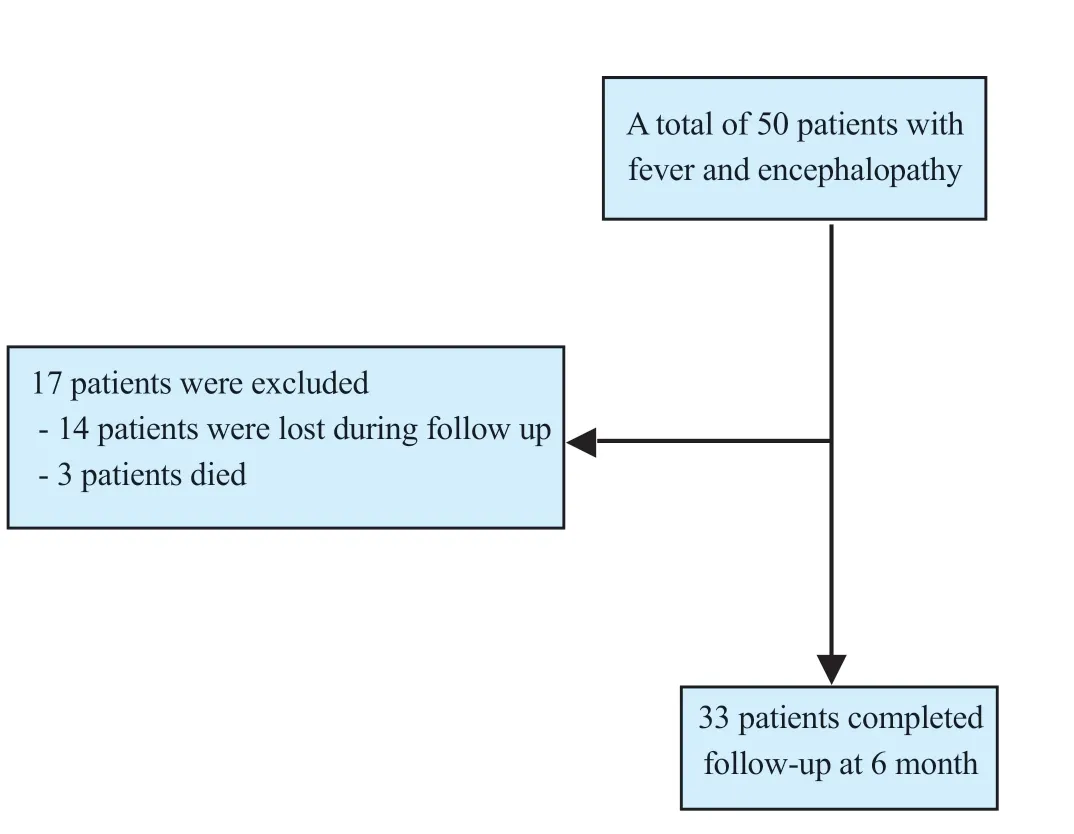
Figure 1.The study flowchart.
3.1.Demographic and clinical characteristics
The mean age of all the enrolled patients with febrile encephalopathy was (58.0±16.0) years with male to female ratio of 1.27∶1.Among all,21 (42%) patients had hypertension,and 15 (30%) patients had diabetes mellitus.At presentation,9 (18.0%) patients had tachycardia,3 (6.0%) had bradycardia,10 (20.0%) had high and 7 (14.0%) had low systolic blood pressure,6 (12.0%) had low and 8 (16.0%) had high diastolic blood pressure,and 6 (12%) patients had low SpO2(<94%).Of 50 patients,6 (12.0%) presented with shock in the emergency department.Baseline demography and clinical findings of all the enrolled patients are outlined in Tables 1 and 2.
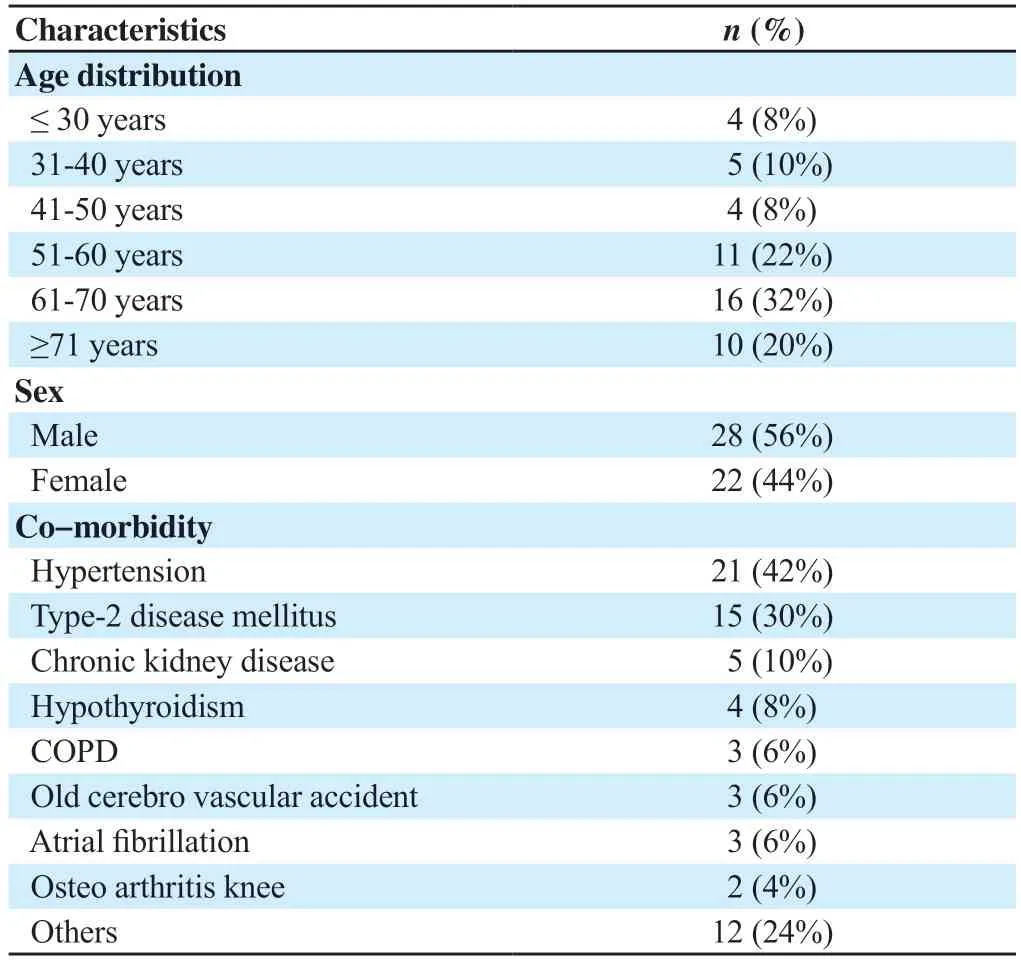
Table 1.Baseline data of patients (n=50).
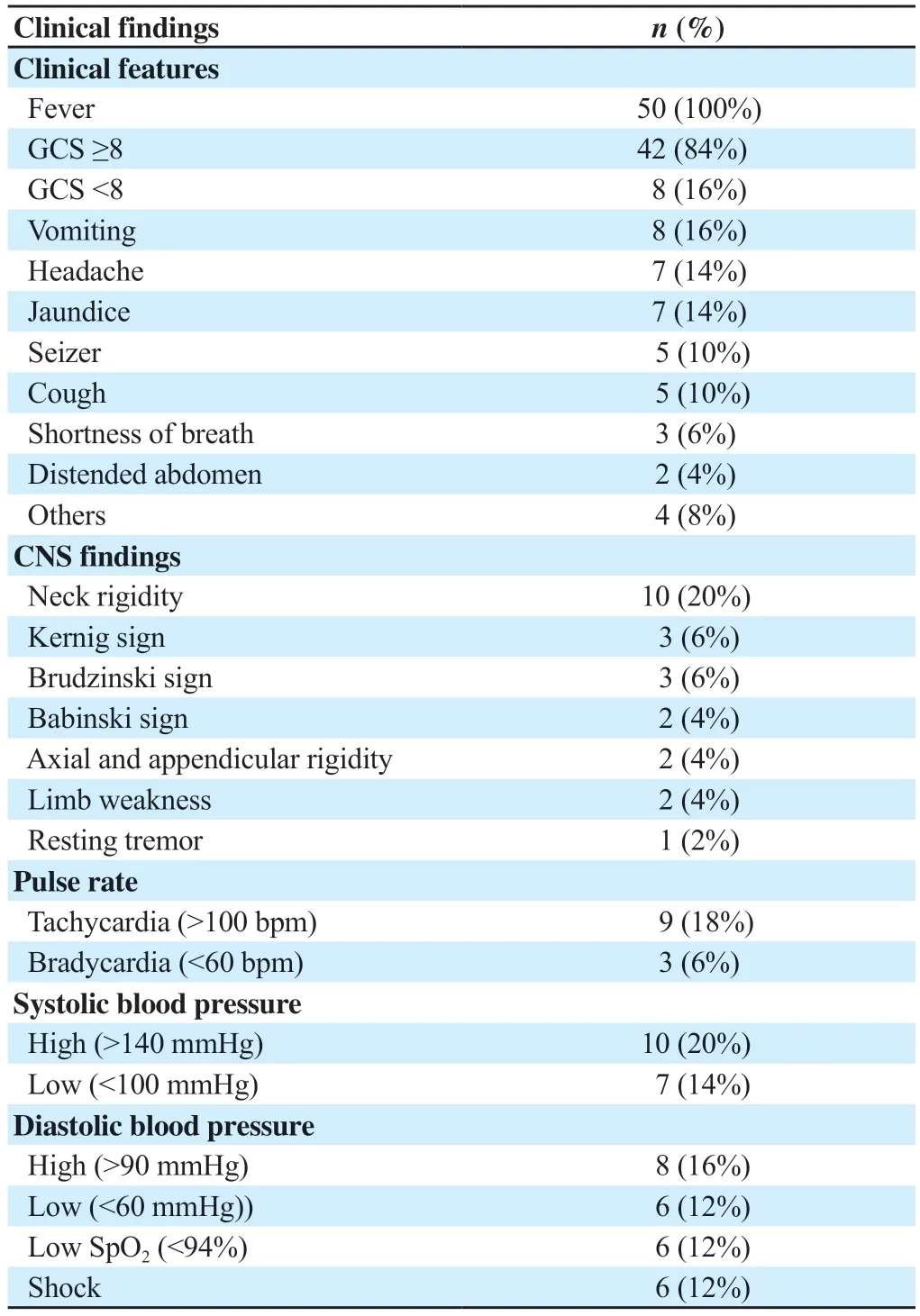
Table 2.Clinical findings (n=50).
3.2.Laboratory finding
Complete blood count of all the enrolled patients revealed anemia (male: <13.5 mg/dL and female: <12.5 mg/dL) in 29 patients,leucocytosis (>11 000 cells/mm3) in 20 patients,leucopenia (<4 000 cells/mm3) in 5 patients,thrombocytosis (>4 lakh cells/mm3) in 6 patients and thrombocytopenia (<1.5 lakh cells/mm3) in 20 patients.C-reactive protein level was high in 29 (58%) patients.The investigation of electrolyte levels revealed hyponatremia in 19 (38%) patients,hypernatremia in 3 (6%),hypokalemia in 17 (34%),and hyperkalemia in 1 (2%) patient.In addition,26 (52%) patients had high blood urea levels and 21 (42%) had high serum creatinine levels.Furthermore,total bilirubin level was 1.5 (0.2,23.7) mg/dL,aspartate transaminase was 138.1 (15.9-1 842.3) IU/dL,alanine transaminase 126.7 (10.6,1 966.1) IU/dL and normal alkaline phosphatase 107.9 (50.5,345.2) IU/dL.The random blood glucose level was (127.96±39.02) mg/dL which showed higher levels (>200 mg/dL) in two (4%) patients.The detailed laboratory findings are depicted in Table 3.

Table 3.Laboratory findings (n=50).
3.3.Imaging results
Chest X-ray revealed pleural effusion either unilateral or bilateral in 7 (14%) patients,non-homogenous opacity in 10 (20%) patients,and cardiomegaly in 4 (8%) patients.Abdominal ultrasound revealed hepatomegaly in 6 (8%) patients and splenomegaly in 4 (8%),whereas 3 (6%) patients had intraabdominal collections.Contrastenhanced CT of the chest and abdomen revealed consolidations in different lung fields in 6 (12%) patients of which 5 (10%) each had pleural effusion and ground-glass opacity,whereas 3 (6%) patients had a tree-in-bud appearance.Non-contrast CT scans showed old infarct in the brain in 4 (8%) patients,fresh infarct in the brain in 2 (4%),whereas 3 (6%) patients showed small vessel ischemic changes.Brain magnetic resonance imaging showed diffuse cerebral atrophy in 5 (10%) patients and ventriculomegaly in 3 (6%) patients.Hyperintensity was noted in T2WI/FLAIR in the temporal lobe of 3 (6%) patients,which suggested herpes encephalitis.
3.4.Diagnosis result
Based on all the examinations,viral encephalitis was diagnosed in 16 (32%) patients,sepsis-associated encephalitis in 14 (28%) patients,bacterial meningoencephalitis in 8 (16%) patients,and tuberculosis meningoencephalitis in 5 (10%) patients.In addition,3 patients were diagnosed with pneumonia,including 2 patients with lobar pneumonia and 1 with atypical pneumonia.Central nervous system infection (~52%) was the most frequent etiology of febrile encephalopathy followed by sepsis-associated encephalopathy (24%).Other causes of febrile encephalopathy found in our study were autoimmune encephalitis (n=1),cerebral malaria (n=1),paraneoplastic syndrome (n=1),scrub typhus (n=1),uremic encephalopathy (n=1) and viral hepatitis (n=1) (Table 4).
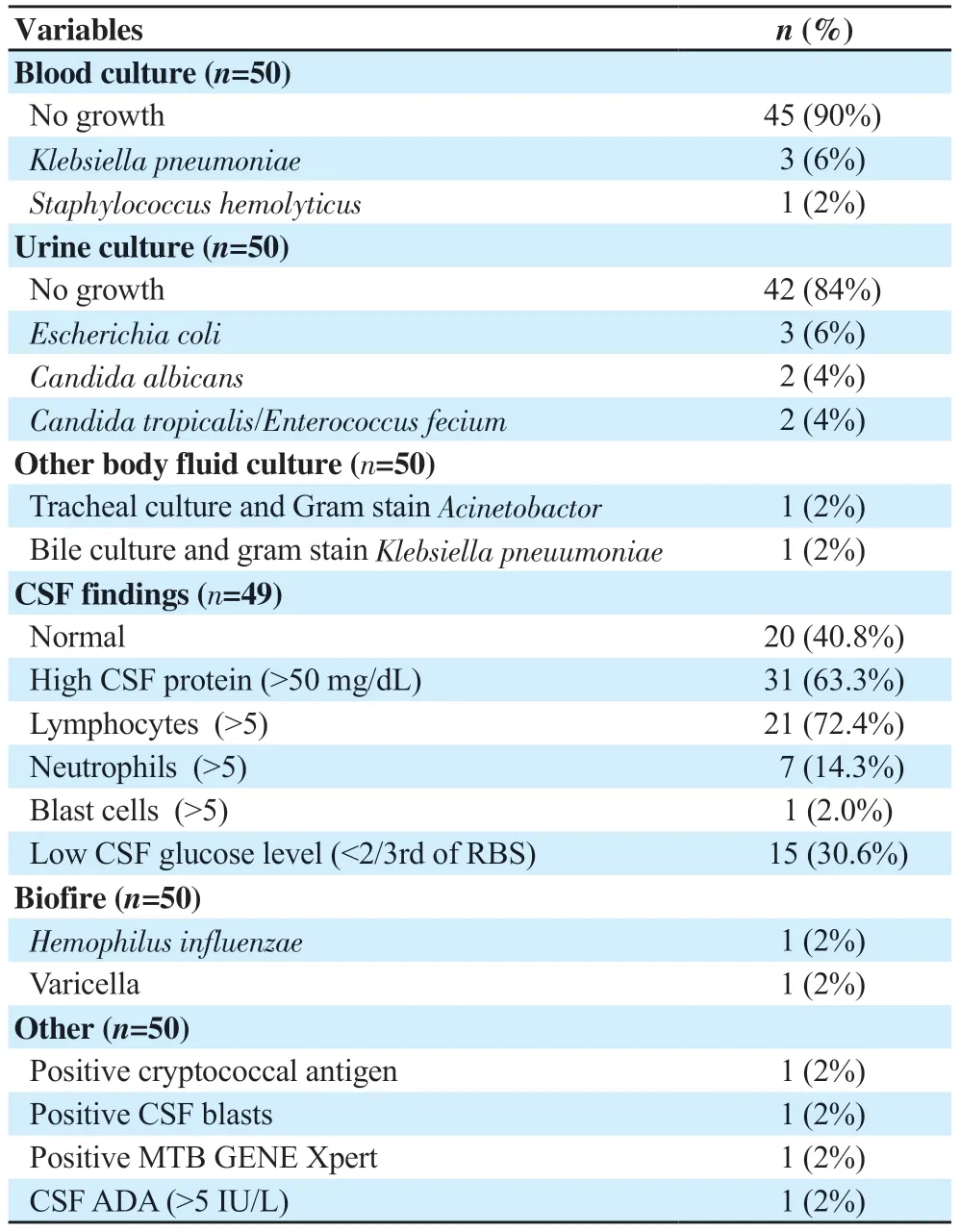
Table 4.Culture findings of different body fluids (n=50).
3.5.Outcome of patients
The mean hospital stay was 10 (4,17) days.At 6-month followup,10 (20%) patients died,10 patients recovered with sequelae (cognitive impairment,critical care neuropathy,etc.),and 30 patients recovered without sequelae.
Patients with bacterial meningitis had the highest fatality rate (50%);however,patients with tuberculosis-associated encephalitis had a higher rate of sequelae (60%).The association of mortality and different etiological variables in patients with febrile encephalopathy is outlined in Table 5.Patients with Glasgow Coma Scale (GCS) <8 had lower mortality.
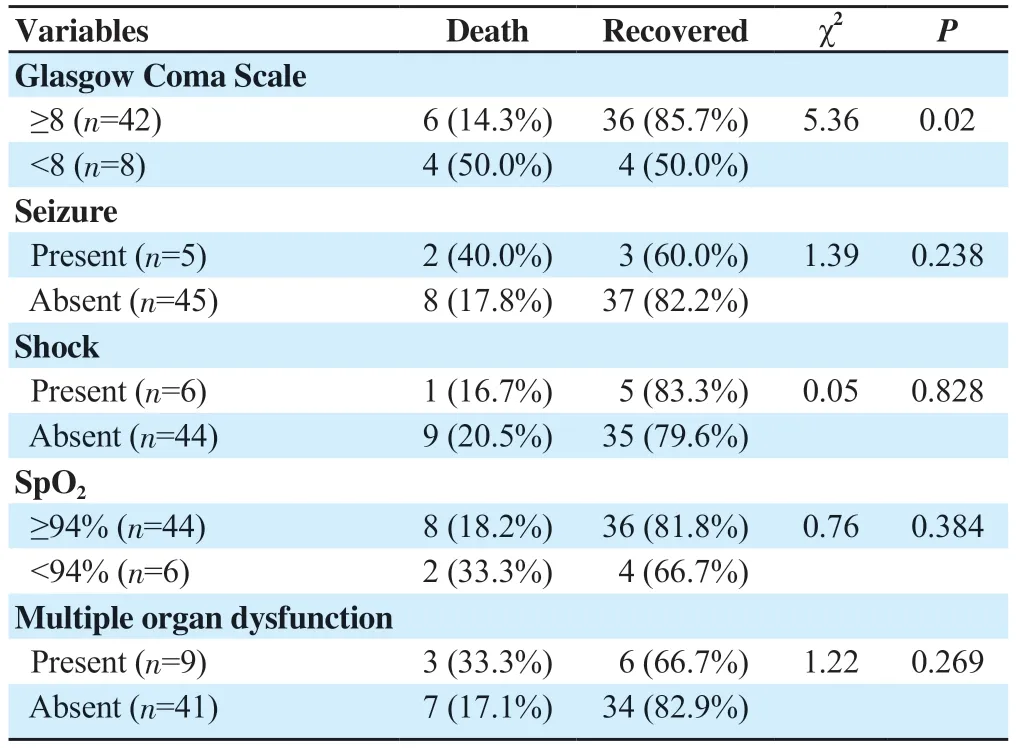
Table 5.Association of etiological variable and mortality in patients with febrile encephalopathy (n=50).
4.Discussion
Encephalopathy refers to a syndrome that is not specific to a particular cause but indicates diseases or etiologies that affect the brain,leading to structural and functional changes in the central nervous system.Encephalopathy accompanying fever is one of the most common encounters in the emergency department and its wide range of potential causes makes it challenging for physicians to make an accurate and timely diagnosis.This study evaluated the demographic parameters,clinical profile,etiology,and outcomes of febrile encephalopathy in patients in Eastern India.
Contrary to the previous findings,the mean age of patients with afebrile encephalopathy in the present study was older (58.0±16.0) years (ranging from 19 years to 86 years) and the majority of patients (52%) were of >60 years of age.In most of the previous studies conducted on Indian adults presenting with acute afebrile encephalopathy,the mean age was <50 years,and even in Iranian patients the mean age was <50 years[6-10].In our study,no male preponderance was noted (male/female ratio=1.27∶1),which was contradictory to the previous studies[4,6-8].Hypertension (42%) and type-2 diabetes mellitus (30%) were the two most common comorbidities found in our patients,which was similar to the previous findings[7,8].In the present study,40% of patients had normal CSF analysis.The most common CSF abnormalities included high CSF protein (63.3%),lymphocytic pleocytosis (42.9%),and neutrophilic pleocytosis (14.3%).One patient showed the presence of lymphoblasts in CSF and subsequent etiological evaluation revealed acute lymphoblastic leukemia.Specific etiological diagnosis with positive CSF PCR was noted in one case each for varicella zoster,Mycobacterium tuberculosis,cryptococcal antigen,andHemophilus influenzae.
The present study reported viral encephalitis (32%) as the most common etiological diagnosis among patients with febrile encephalopathy.Among this group of patients,two COVID-19 patients developed encephalopathy.However,these patients responded well to treatment with intravenous immunoglobulins and rituximab.In line with the present findings,a study by Jobet al.[8]on south Indian patients reported viral encephalitis in 28.9% of cases and a study by Senet al.[6]on East Indian patients reported viral encephalitis in 30% of cases.Contrary to the findings of the previous studies[4,6,8],a higher number of cases of sepsisassociated encephalopathy (28%) were reported in the present study.Pneumonia was found as the most common cause of sepsisassociated encephalopathy in the present study as well as in the previous study by Anguset al.[11].Moreover,tuberculosis-associated febrile encephalopathy was reported in 10% of cases in the present study which was comparable to the findings of previous studies on patients of different geographies in India[4,6-8].In the present study,bacterial meningoencephalitis was diagnosed in 8 patients with culture-confirmed infective etiologies includingKlebsiella pneumoniae(n=3),Staphylococcus hemolyticus(n=2),and others (n=4) Therefore,in accordance with previously published data[4-6],central nervous system infection (~52%) was the most frequent etiology of febrile encephalopathy followed by sepsis-associated encephalopathy (24%).Other causes of febrile encephalopathy found in our study were autoimmune encephalitis (n=1),cerebral malaria (n=1),paraneoplastic syndrome (n=1),scrub typhus (n=1),uremic encephalopathy (n=1) and viral hepatitis (n=1).
The present study showed an overall mortality rate of 20% which was comparable with the mortality rates reported by Bhallaet al.[7](16.5%),Modiet al.[4](13.4%) and Senet al.[6](24%).Among survival patients,most recovered without any sequelae,and 20% of patients developed sequelae such as cognitive impairment,critical care neuropathy,or other.On further analysis,the present study noted the highest fatality rate among patients with acute bacterial meningoencephalitis (50%) followed by sepsis-associated encephalopathy (38%).A nationwide multi-centered study in Korea by Moonet al.[12]demonstrated 20.5% mortality in patients with bacterial meningitis.
A total of 14.3% of patients having ≥8 GCS and 50.0% of patients having <8 GCS at initial presentation had died and the association of GCS with mortality rate was statistically significant (P=0.02).However,no statistically significant association of presence shock at presentation,seizure at presentation,SpO2<94% at presentation,and multiple organ dysfunction with mortality rate was found in patients with febrile encephalopathy.In a study by Biswaset al.[13],it was seen that low GCS,refractory seizures,multiple organ dysfunction,and respiratory failure were significantly associated with mortality (P<0.05) in patients with febrile encephalopathy.
However,this study still has some limitations.Small sample sizes and single-center experience make it very difficult to generalize current findings and extrapolate data to the general population.Therefore,further larger studies covering different geometries are required to generalize etiological findings and outcomes in patients with febrile encephalopathy.
Conflict of interest statement
The authors report no conflict of interest.
Funding
This study received no extramural funding.
Authors'contributions
All authors have equally contributed to the concept and design of study,acquisition of data,analysis and interpretation of data,drafting the article or revising it critically for important intellectual content,and final approval of the version to be published.
 Journal of Acute Disease2023年4期
Journal of Acute Disease2023年4期
- Journal of Acute Disease的其它文章
- Biochemical indicators and the Peradeniya Organophosphate Poisoning scale in prediction and prognosis of organophosphorus poisoning: An observational prospective study
- Heparin-binding protein combined with human serum albumin in early assessment of community-acquired pneumonia: A retrospective study
- Effects of long COVID-19 among young adults in Turkey: A crosssectional study
- Epidemiology of animal bite injuries in North of Fars province in Iran
- Clinical and epidemiological features of pelvic fractures presenting to the emergency department in a tertiary health care hospital in south India: A retrospective study
- Central venous catheterization-related complications in a cohort of 100 hospitalized patients: An observational study
