Prevalence and risk factors for acquired long QT syndrome in the emergency department: a retrospective observational study
Diogo de Almeida Fernandes , Guilherme de Freitas Camões, Diana Ferreira, Carolina Queijo, Carlos Fontes-Ribeiro,4, Lino Gonçalves,4, Rui Pina, Natália António,4
1Department of Cardiology, Coimbra Hospital and University Centre (CHUC), Coimbra 3000-075, Portugal
2Department of Internal Medicine, Coimbra Hospital and University Centre (CHUC), Coimbra 3000-075, Portugal
3Faculty of Medicine, University of Coimbra, Coimbra 3000-370, Portugal
4Institute for Clinical and Biomedical Research, Faculty of Medicine, University of Coimbra, Coimbra 3000-548, Portugal
KEYWORDS: Long QT syndrome; Epidemiology; Drug interactions; Emergency department
INTRODUCTION
Long QT syndrome (LQTS) is a heterogeneous syndrome that may be congenital or acquired,[1]the latter being more common.[2]It is defined as a prolonged corrected QT (QTc) interval in the electrocardiogram(ECG) with values greater than 470 ms in men and 480 ms in women.[3]Values higher than 500 ms are considered severe for both sexes and indicate a particularly high risk for torsades de pointes (TdP)or polymorphic ventricular tachycardia (pVT).[3,4]An increase >60 ms from the QTc baseline is also considered an alarming sign.[5]pVT and TdP may present with syncope, cardiac arrest or sudden cardiac death (SCD).Timely diagnosis and treatment are crucial to prevent them.[4,6]
Risk factors for acquired LQTS (aLQTS) include female sex, advanced age, metabolic disorders,electrolyte imbalances and cardiac diseases (acute coronary syndromes and myocarditis).[7–9]The most common cause of prolongation of the QT interval is drugrelated.A wide range of different drug classes influence repolarization, including class IA antiarrhythmics,[8]class III antiarrhythmics,[7]fluoroquinolones, macrolides,antifungals, antipsychotics, antidepressants, H1 antihistamine and anticholinergics.[8,10–16]
The real-world prevalence of aLQTS remains to be determined, and specific data regarding its prevalence in the emergency department (ED) is largely unknown.Additionally, this syndrome includes a heterogeneous group of patients who lacks better analysis.
Previous studies reported a prevalence between 28.5%–35% in the ED for QT prolongation, both acquired and hereditary.[17–20]Also, approximately 25%of the patients admitted to cardiac intensive care units(ICUs) had prolonged QTc intervals at admission[3]and 20%–24% had severely prolonged QTc intervals when admitted to any ICU.[21,22]The prevalence of QTc interval greater than 500 ms in other hospital wards was 0.7%–0.9%.[23,24]
Our aim was to determine the prevalence of aLQTS in patients admitted to the ED and to characterize the subset of patients at particularly high risk of TdP (patients with QTc>500 ms).
METHODS
Study design and patient selection
We performed a retrospective study of consecutive patients admitted to the ED of a tertiary hospital between the 28thof January and 17thof March 2020 (prepandemic period in Portugal).
This study was performed in line with the principles of theDeclaration of Helsinki.Approval was granted by the Local Ethics Committee (OBS.SF.23/2021).Due to the observational aspect of this study, informed consent was waived.
Patient eligibility criteria
Patients were eligible for inclusion if they had an ECG with a prolonged QTc interval using Bazett’s formula (greater than 470 ms in men and 480 ms in women as defined by the American Heart Association and American College of Cardiology Foundation).[3]
Exclusion criteria were the following: 1) congenital LQTS or known relative with LQTS; 2) repeated ED admissions; 3) bad ECG quality; 4) atrial fibrillation (AF)/atrial flutter; and 5) pacemaker rhythm.
Data collection
Variables retrieved were age, sex, clinical presentation (palpitations, presyncope, syncope, seizure or cardiac arrest) and QT prolonging drugs or with known risk of TdP and risk factors contributing to prolonged QT interval as determined by CredibleMeds®(an online resource that promotes the safe use of medicines).[8]QTc was determined using the Bazett’s formula and uncorrected QT interval as measured manually by the main researchers using the average of three measurements.
Drugs were grouped according to drug class:antiarrhythmics, antibiotics, antihistamines, antiemetics,antifungal, immunomodulators, opioids, antipsychotics,antidepressants, diuretics, anti-migraine, bronchodilators,hormones, proton-pump inhibitors (PPIs) and others.
Study endpoints
The primary endpoint was to determine the prevalence of aLQTS and its impact on symptoms at admission to the ED.
The secondary endpoints focused on determining risk factors for a severely prolonged QT interval defined as values greater than 500 ms.[3]
Data analysis
Statistical analysis was performed using IBM SPSS Statistics version 26.Categorical variables are presented as frequencies and percentages, and continuous variables as means and standard deviations if normally distributed, or as medians and interquartile ranges for variables with skewed distributions.Normal distribution was verified through the Kolmogorov-Smirnov test or skewness and kurtosis (maximum tolerated interval of -1 to 1).
Bivariate analysis was performed by using Chisquare test (or Fisher exact test as appropriate) for categorical variables with a Bonferroni correction for multiple analyses and independentt-test for continuous variables.Using logistic regression, odds ratio (OR) were determined for the variables withP<0.100.All reportedPvalues are two-tailed with values less than 0.05 indicating statistical significance.The authors had full access to data and take full responsibility for its integrity.
RESULTS
A total of 6,280 ECGs were identified.These ECGs belonged to 5,056 patients.A total of 1,380 ECGs were subsequently excluded.No patients with a prior diagnosis of LQTS were identified.The final sample comprised 2,573 women and 2,327 men.A total of 383 ECGs with prolonged QTc were recognized (Figure 1).The total prevalence of aLQTS was 7.82%.
Patients with aLQTS were more commonly men(n=204; 53.3%) with an average age of 73.49 ± 14.79 years old (range 19–95 years) and average QTc interval of 505.3 ± 32.4 ms (range 470–680 ms).The majority of patients were asymptomatic (79.6%) and the most common symptom was syncope (39/78) followed by presyncope (22/78).No TdP or pVT were documented.Baseline characteristics and risk factors are shown in Table 1.Diuretics, PPIs, antidepressants, and antipsychotics were among the classes most frequently present in patients with prolonged QT (Table 2).
Subgroup analysis of patients with severely prolonged QTc interval (>500 ms)
There were 163 patients with severely prolonged QTc intervals (> 500 ms), corresponding to a prevalence of 3.3% (and 42.6% of the overall aLQTS group).
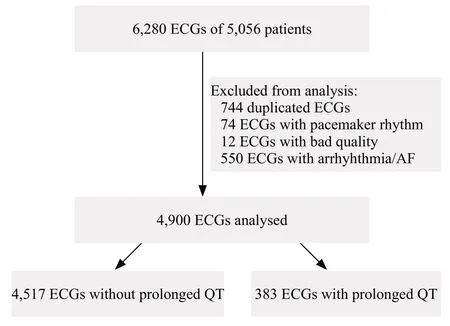
Figure 1.Flowchart of ECG selection.ECG: electrocardiogram; AF:atrial fibrillation.
Female patients (59.5%;P<0.001) and patients on QT prolonging drugs (77.3%;P=0.025) were more likely to have a severely prolonged QTc interval (Table 3).Additionally, the use of a greater number of drugs and particularly, intake of antibiotics (P=0.004), antipsychotics (P=0.014)or antidepressants (P=0.028) were associated with severely prolonged QTc interval (Table 3).There was also a trend for prolonged QTc intervals in patients on diuretics (P=0.051) (Table 3).Of note,although the mean number of risk factors was greater in the population with severely prolonged QTc intervals, the difference was not statistically significant (P=0.055) (Table 3).No statistically significant differences were found regarding age,clinical presentation or type of risk factors present.
Using logistic regression, patients on antibiotics had the greatest odds of severely prolonged QTc interval (OR4.860; 95% confidence interval (95%CI) 1.497–14.631;P=0.008).Female patients had almost 2.5 times greater odds of severely prolonged QTc (OR2.473; 95%CI1.663–3.747;P< 0.001).The remainingORs are shown on Table 4.
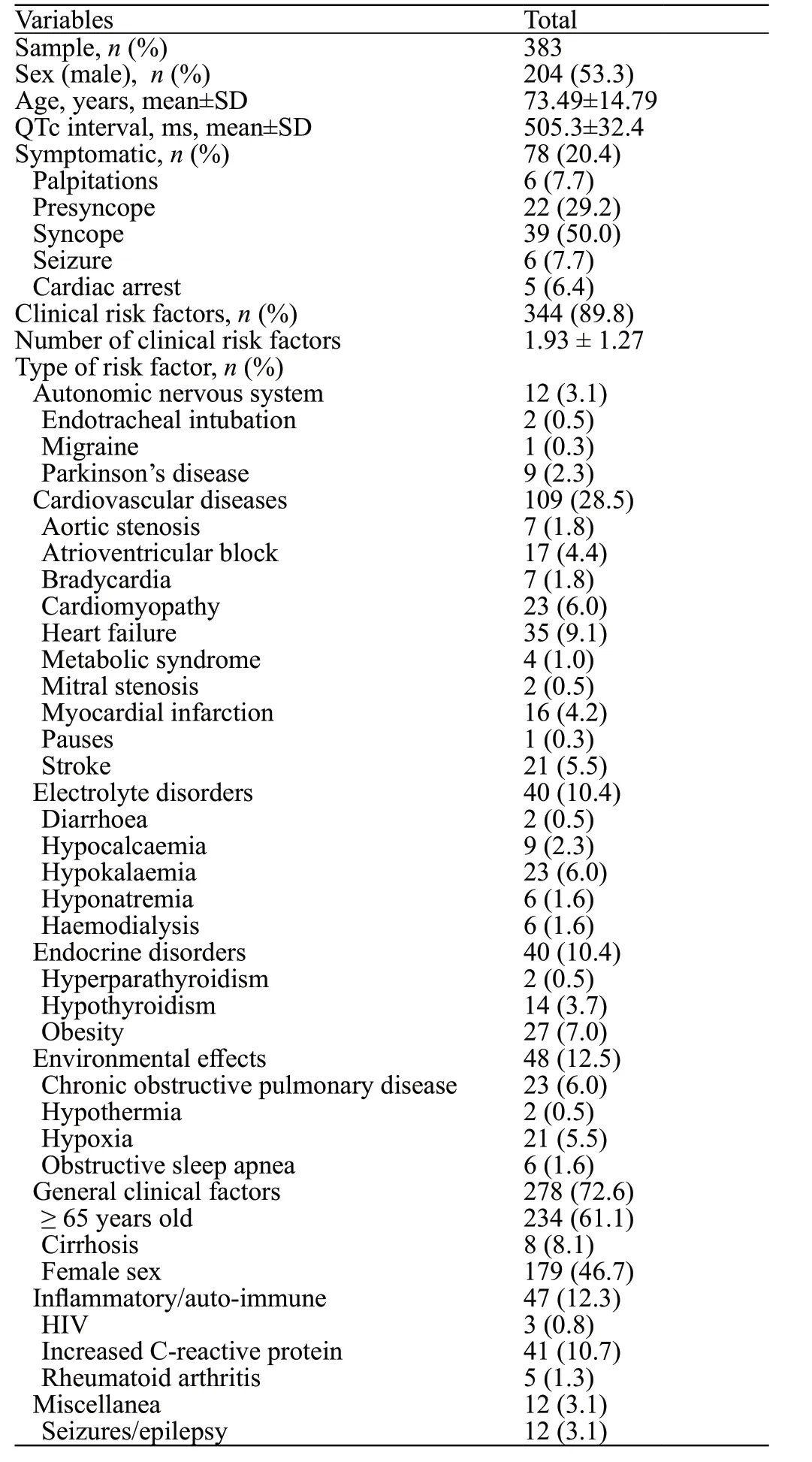
Table 1.Baseline characteristics and risk factors of the studied population
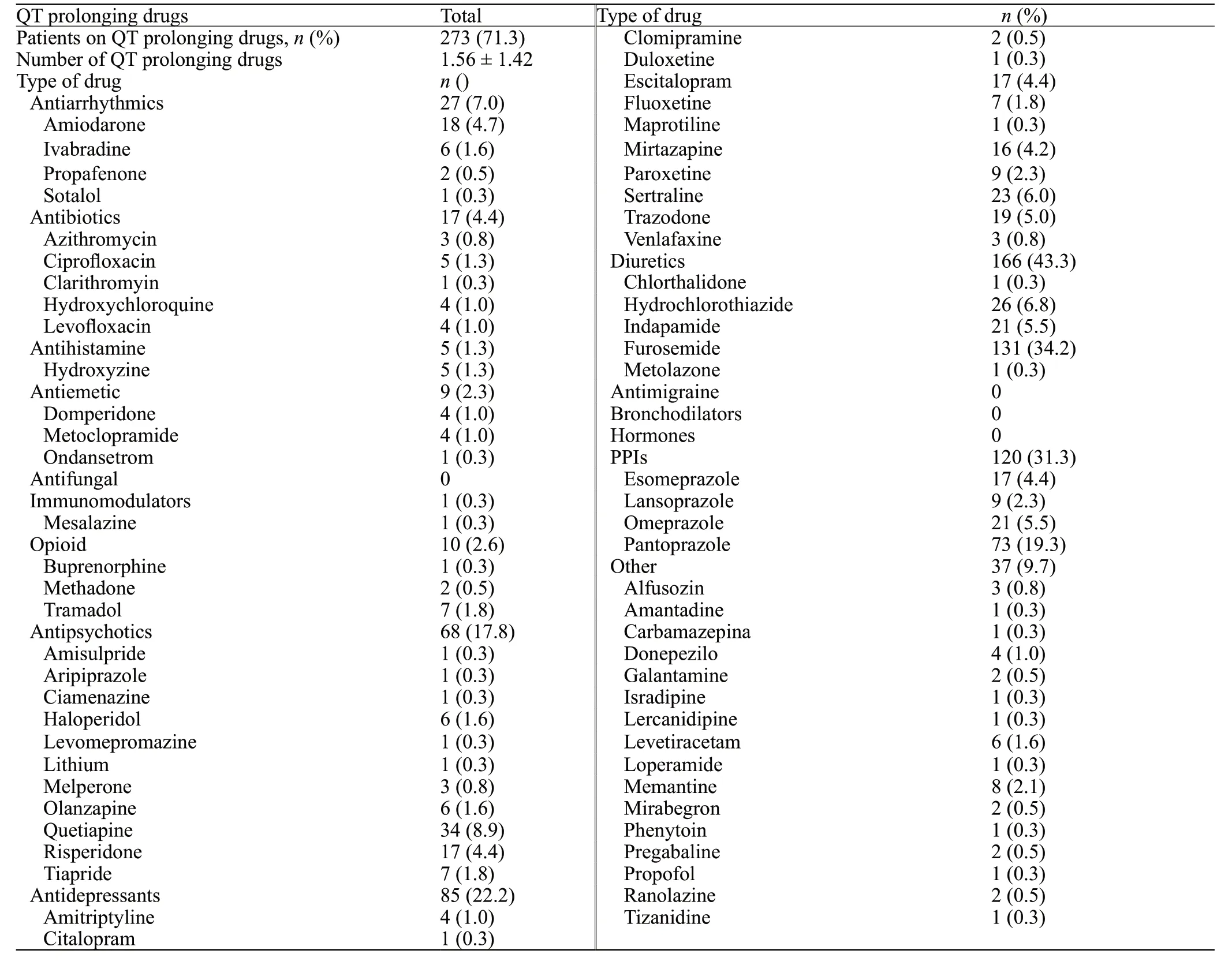
Table 2.Patients on QT prolonging drugs
DISCUSSION
Acquired LQTS is an often-overlooked entity that lacks better understanding and study.Previous studies estimate that the prevalence of LQTS in the ED is 30%–40%.[17–20]Our results show that this syndrome is particularly common in this setting, even when accounting only for patients with a severely prolonged QTc.Similar to other studies, we detected that these were mainly older patients (73.49±14.79 years).[2,25]Of note, the great majority of patients in this study had no symptoms that could draw attention to LQTS.As such, careful evaluation of the QT interval is key, even in asymptomatic patients, as it may be the only sign detected before a dysrhythmic event and death.
Regarding drugs contributing to this syndrome,most interact with thehERGgene and the IKrchannel.[26]In this study, and in contrast to previous studies where antiarrhythmics had the spotlight,[2,25]diuretics (and in particular, furosemide) were the drugs most commonly associated with LQTS in our emergency population.In addition to contributing to ionic imbalance, furosemide may lead to QT prolongation even when corrected for low serum levels of calcium and potassium.[27]We hypothesize that the high prevalence of these drugs in our population reflects advanced age and the fact that heart failure and hypertension are particularly frequent in the ED setting.
The second most prescribed drug class in this population was PPIs, mainly pantoprazole.Its impact is mainly due to decreased absorption of magnesium and consequent hypomagnesaemia and not by directly prolonging QT.[28,29]This effect is particularly magnified in the presence of diuretics.[28]
Antipsychotropic medication also plays a crucial role in a large subset of patients.[30]Antidepressants (selective serotonin reuptake inhibitor [SSRI] but also tricyclic drugs) are increasingly prescribed and used chronically.[31]The main mechanism for QT prolongation appears to be Na+channel blockage in tricyclic agents and inhibition of the IKrchannel in SSRIs.[14]Their impact on the QT interval demands a careful risk-benefit analysis prior to their initiation and in every hospital appointment,[32,33]as excessive dosage or co-administration with other drugs such as K+channel blockers may lead to a devastating effect.[14,34]Regarding antipsychotics, their impact has long been studied and is mainly mediated by hERG channel blockade.[35]Nearly all antipsychotics cause QT prolongation[32]but particular attention needs to be given to patients on haloperidol, thioridazine, pimozide,ziprasidone, risperidone, melperone, and quetiapine, as they are known to prolong QT the most.[34]
Also of note are antibiotics.Macrolides and fluoroquinolones are increasingly utilized in clinical practice as beta-lactam resistance surges.Similar to SSRIs, blockade of the IKrchannel is the main contributor to QT prolongation.[14,30,36]In addition, CYP3A4 inhibition by macrolides can also increase the half-life and concentration of other QT prolonging drugs and dramatically increase QTc.[14]
Classically regarded as the main culprits of prolonged QT, antiarrhythmics were found in only a small proportion of our sample.Nonetheless, the same channel blocking capabilities responsible for their antiarrhythmic effectcontribute to QT prolongation and TdP.[14,30,37]As such,careful ECG monitoring, especially in class IA (quinidine,procainamide and disopyramide) and class III agents (such as amiodarone and sotalol), is needed to maintain a tight control of the clinical status.[14]

Table 3.Comparison between patients with and without severely prolonged QTc interval
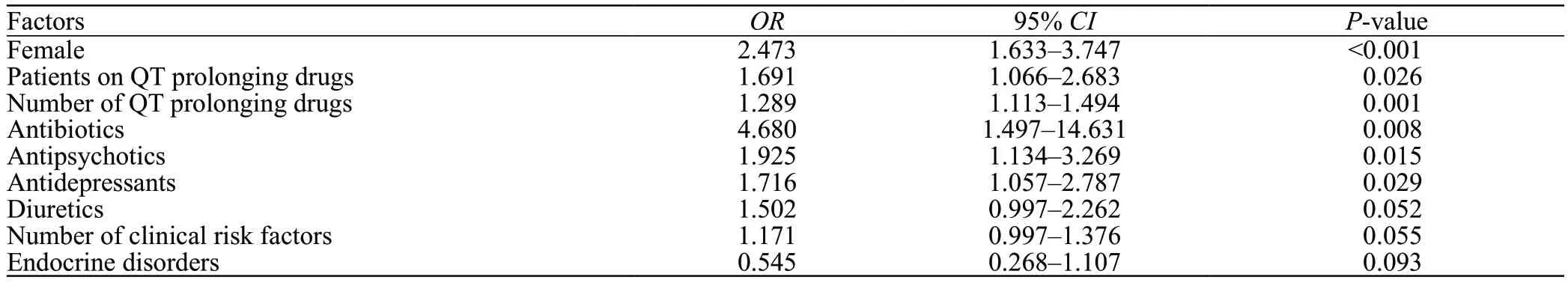
Table 4.Logistic analysis of the risk factors of severely prolonged QTc interval
Regarding clinical risk factors, our study showed that patients with elevated C-reactive protein more frequently had LQTS in the ED.Recent studies have shown that the inflammatory pathway affects the electrophysiological properties of cardiomyocytes, contributing to changes in repolarization and consequent QT prolongation.[38]Heart failure was also particularly prevalent in our study population.Multiple mechanisms have also been hypothesized to contribute to QT prolongation in heart failure, including structural changes and heterogeneous depolarization, in addition to the effect of drug iatrogenesis.[39,40]Hypokalemia is also a determinant factor in prolonging QT.Its impact on the functioning of potassium channels leads to synergy with the inhibiting properties of QT prolonging drugs and a marked increase in the risk of ventricular fibrillation (VF) and TdP.[41]
A QT interval greater than 500 ms has been linked to an increased risk of ventricular arrhythmias and complications.[3,24]Our study demonstrated that female patients on antibiotics were at an increased risk of severely prolonged QT interval.Other particularly relevant contributors to this severely prolonged QTc were the number of QT prolonging drugs, clinical risk factors,and the use of antipsychotics and antidepressants.Studies have shown that antipsychotics and antidepressants are being prescribed at a particularly high and increasing rate in recent years, particularly in elderly patients.[42–44]In fact, most recent national studies found an increasing trend for overall polypharmacy in the elderly, reaching in some cases a general prevalence of 8%–29%.[45–48]This fact leads not only to increased direct costs in healthcare systems, but also to a greater risk of drug and clinical factor interactions.Accordingly, careful monitoring of baseline and follow-up ECG in this therapeutic setting is crucial to avoid severe QT prolongation.
Despite the increased risk of TdP, the direct correlation between QT prolongation and clinical presentation remains to be fully determined.[7,24]Our study showed no link between a severely prolonged QT interval and symptoms.
Limitations
Our study was retrospective and unicentric which may have led to bias in the sample selection and increased the probability of the presence of confounders.Other factors contributing to QT prolongation such as race and socioeconomic status were not evaluated due to the lack of reporting on the clinical data used.Additionally, it was impossible to ascertain the prognostic influence of aLQTS during follow-up and correction using Bazett’s formula may overcorrect the QT interval at higher heart rates.
CONCLUSION
In conclusion, aLQTS is particularly prevalent in the ED setting.The complex interaction of clinical factors and drug iatrogenesis and the unpredictability of its manifestations render its management and recognition difficult but essential.Efforts must be made to raise clinicians’ awareness to avoid, detect and treat aLQTS as early as possible.
Funding:The authors did not receive support from any organization for the submitted work.
Ethical approval:All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964Helsinki Declarationand its later amendments or comparable ethical standards.The study was approved by the Ethics Committee of Centro Hospitalar e Universitário de Coimbra(OBS.SF.23/2021).
Conflicts of interest:The authors have no relevant financial or non-financial interests to disclose.
Author contribution:DAF and GC contributed equally to the work and are co-first authors.Conception and design of study:DAF, GC, DMF, CQ; Acquisition of data: DAF, GC, DMF, CQ;Analysis and/or interpretation of data: DAF, GC, DMF, CQ;Drafting the manuscript: DAF, GC, DMF, CQ; Revising the manuscript critically for important intellectual content: CFR,LG, RP, NA; Approval of the version of the manuscript to be published: DAF, GC, DMF, CQ, CFR, LG, RP, NA.
 World journal of emergency medicine2023年6期
World journal of emergency medicine2023年6期
- World journal of emergency medicine的其它文章
- Tension urinothorax as a reversible cause of cardiac arrest: a case report
- A case of pulmonary mucormycosis presented with cardiac arrest
- Pyopneumothorax caused by Parvimonas micra and Prevotella oralis: a case report
- Hemorrhagic pancreatitis from fenofibrate and metformin toxicity: a case report
- The effect of prophylactic antibiotics in acute upper gastrointestinal bleeding patients in the emergency department
- The effects of hyperbaric oxygen therapy on paroxysmal sympathetic hyperactivity after cardiopulmonary resuscitation: a case series
