Value and prognostic factors of repeat hepatectomy for recurrent colorectal liver metastasis
Jia-Min Zhou ,Lu Wang ,An-Rong Mao
a Department of Hepatic Surgery,Shanghai Cancer Center,Fudan University,Shanghai 20 0 032,China
b Department of Oncology,Shanghai Medical College,Fudan University,Shanghai 20 0 032,China
Keywords: Hepatectomy Colorectal neoplasms Liver neoplasms Neoplasm recurrence Prognosis
ABSTRACT Background: More than 50% of patients with colorectal cancer develop liver metastases.Hepatectomy is the preferred treatment for resectable liver metastases.This review provides a perspective on the utility and relevant prognostic factors of repeat hepatectomy in recurrent colorectal liver metastasis (CRLM).Data sources: The keywords “recurrent colorectal liver metastases”,“recurrent hepatic metastases from colorectal cancer”,“liver metastases of colorectal cancer”,“repeat hepatectomy”,“repeat hepatic resection”,“second hepatic resection”,and “prognostic factors” were used to retrieve articles published in the PubMed database up to August 2020.Additional articles were identified by a manual search of references from key articles.Results: Despite improvements in surgical methods and perioperative chemotherapy,recurrence remains common in 37%–68% of patients.Standards or guidelines for the treatment of recurrent liver metastases are lacking.Repeat hepatectomy appears to be the best option for patients with resectable metastases.The commonly reported prognostic factors after repeat hepatectomy were R0 resection,carcinoembryonic antigen level,the presence of extrahepatic disease,a short disease-free interval between initial and repeat hepatectomy,the number (>1) and size (≥5 cm) of hepatic lesions,requiring blood transfusion,and no adjuvant chemotherapy after initial hepatectomy.The median overall survival after repeat hepatectomy ranged from 19.3 to 62 months,and the 5-year overall survival ranged from 21% to 73%.Chemotherapy can act as a test for the biological behavior of tumors with the goal of avoiding unnecessary surgery,and a multimodal approach involving aggressive chemotherapy and repeat hepatectomy might be the treatment of choice for patients with early recurrent CRLM.Conclusions: Repeat hepatectomy is a relatively safe and effective treatment for resectable recurrent CRLM.The presence or absence of prognostic factors might facilitate patient selection to improve shortand long-term outcomes.
Introduction
Colorectal cancer is the third most diagnosed cancer,with 1.8 million new cases,and has the second highest mortality rate,with almost 881 0 0 0 deaths in 2018 worldwide [1].The main cause of mortality in most patients with colorectal cancer is metastasis,and the liver is the predominant metastatic site due to hematogenous dissemination.Curative-intent surgery for colorectal liver metastasis (CRLM) has been demonstrated to be beneficial,with a 5-year survival rate of 30%–58% [2,3].Despite improvements in surgical methods and perioperative chemotherapy,37%–68% of patients with CRLM present with recurrent lesions after initial resection [4–7].Different studies have reported a median time to recurrence of up to 2 years,with intrahepatic lesions being the most predominantly observed evidence of recurrence [4,8,9].An international multi-institutional analysis reported that 947 (56.7%)of 1669 patients developed recurrence,43.2%,21.0%,and 35.8%of whom experienced intrahepatic only,intra-and extrahepatic,and extrahepatic only recurrence,respectively [4].Inadequate resection margins,missed occult lesions from the first operation,and natural progression of micrometastatic disease may explain recurrence [10–13].
The high rate of hepatic recurrence after initial hepatectomy underscores the importance of repeat hepatectomy in these patients.Among CRLM patients experiencing recurrence after initial resection,25%–38% of patients might be eligible for repeat hepatectomy as salvage therapy [5,14].A subset of patients has also been reported to have undergone subsequent third and fourth curative hepatectomies [5].The survival outcome of repeat hepatectomy is comparable to that of the first hepatectomy in a subset of patients with favorable prognostic factors,whereas it may be compromised in patients with unfavorable prognostic factors [5,14].
Despite the availability of studies,the utility of repeat hepatectomy in patients with intrahepatic recurrence of CRLM remains controversial owing to the overlooked selection bias of the available studies and a lack of prospective studies.In this review,we provide a perspective based on available evidence on the challenges and value of repeat hepatectomy in patients with recurrent CRLM.
Search strategies
A literature search was performed in PubMed for articles published in English from inception until August 2020,with a focus on articles related to prognostic factors of repeat hepatectomy for recurrent CRLM.We included the keywords “recurrent colorectal liver metastases”,“recurrent hepatic metastases from colorectal cancer”,“liver metastases of colorectal cancer”,“repeat hepatectomy”,“repeat hepatic resection”,“second hepatic resection”,and“prognostic factors”.Additional articles were identified by a manual search of references from key articles.We retrieved a total of 1298 articles,including 385 non-English articles,which were excluded,and 58 were finally included for a comparative study.
Challenges faced in repeat hepatectomy in patients with CRLM
Curative-intent surgery has been established as the standard treatment for resectable or potentially resectable lesions in patients with CRLM [15].However,the treatment for hepatic recurrence is not standardized,and the different modalities used in clinical practice include repeat hepatectomy,locoregional therapy,systematic chemotherapy,and a multimodal approach with a combination of different modalities [16].Considering the favorable evidence for repeat hepatectomy,the National Comprehensive Cancer Network (NCCN) guidelines suggest that re-resection can be considered in select patients [17].
The indications for repeat hepatectomy are similar to those for initial hepatectomy.Although the specific contraindications for repeat hepatectomy have not been established,clinical experience guides patient selection.The latest NCCN Clinical Practice Guidelines in Oncology for colon cancer set the criteria for repeat hepatectomy as the presence of surgically resectable hepatic lesions,possible radical surgery,a sufficient future liver remnant volume(20% in “liver healthy” individuals and 30%–40% in patients with liver disease,i.e.,cirrhosis),sufficient inflow and outflow and biliary drainage of remnant liver segments,and the absence of contraindications to hepatic surgery [17].Unlike initial hepatectomy,repeat hepatectomy poses specific challenges owing to previous therapeutic management strategies despite advancements in surgical techniques.The specific challenges include adhesions,distortion of gross liver anatomy,and variations in the hepatobiliary anatomy of the hypertrophied remnant liver,which may affect perioperative parameters such as the operative duration and perioperative blood transfusion [14,18-22].In a retrospective study of 488 patients who underwent hepatectomy,71 underwent repeat hepatectomy,revealing that despite no statistically significant difference in the operative duration or perioperative blood transfusion between the initial and repeat hepatectomy groups,the repeat procedure tended to take more time (operative duration >300 min:95.8% vs.89.5%,P=0.097) and to require more frequent blood transfusions (31.0% vs.27.3%,P=0.512) [23].Other studies also confirmed significantly higher intraoperative bleeding and longer surgery time in repeat hepatectomy compared with those in initial hepatectomy [18,19,24].The observed difference in the duration of repeat resection may be due to the fragile nature of the liver parenchyma chemotherapy and/or regeneration postoperatively,as well as changes in liver texture after the initial hepatectomy.Moreover,the increased difficulty of liver clamping in repeat hepatectomy may lead to increased blood loss necessitating blood transfusion.
The challenges are also reflected in the number of major hepatectomies performed after initial hepatectomy.Evidence showed that the number of major hepatectomies (16.9% vs.40.0%) and anatomic resections (19.7% vs.40.6%) performed during repeat resection was significantly lower than that in the first resection [23].Another study also reported that 47% and 19% of patients with CRLM underwent major initial hepatectomy and repeat hepatectomies,respectively [20].The relative worsening of liver function after major hepatectomy during initial resection can be inferred to complicate the operation and limit the application of repeat hepatectomy in cases of hepatic recurrence.
Short-term outcomes of repeat hepatectomy
Considering that variations in the hepatobiliary anatomy of the hypertrophied remnant liver may cause potential surgical risks,the short-term outcomes of repeat hepatectomy may need to be evaluated by analyzing perioperative morbidity and mortality.A retrospective study analyzed short-term outcomes following initial and repeat hepatectomy for CRLM and reported no statistically significant difference with respect to morbidity (29.7% vs.21.1%,P=0.135),major complications (10.2% vs.8.5%,P=0.638),and 90-day mortality (2% vs.0,P=0.623) between initial and repeat hepatectomies [23].Another study retrospectively reviewed 718 patients who underwent initial hepatectomy,and 66 were subjected to repeat hepatectomy.Postoperative mortality (1.4% vs.0,P=0.387) and morbidity (26.1% vs.18%,P=0.172) were similar between the single hepatectomy and repeat hepatectomy groups,although the median blood loss was significantly higher during repeat resection (450 vs.350 mL,P=0.006) [24].Existing evidence supports that repeat hepatectomy does not result in significantly higher morbidity and mortality than initial hepatectomy.Moreover,quality of life was also not affected after repeat hepatectomy [25].
Multiple studies have also reported the associated mortality and morbidity of third and fourth hepatectomies for CRLM with favorable outcomes.In a previous retrospective study,42 patients underwent 55 (second: 42,third: 11,and fourth: 2) hepatectomies,and the reported morbidity rates for first,second and third repeat hepatectomies were 9.5%,14.3%,and 18.2%,respectively [19].In another study involving a total of 62 patients who underwent at least one repeat hepatectomy,no change in perioperative mortality was noted,and the morbidity increased from 16.1% for the first hepatectomy to 17.7%,26.7%,and 50.0% for the subsequent repeat hepatectomies [21].Considering this evidence,repeat hepatectomy in patients with recurrent CRLM can be construed as a relatively safe procedure despite increased morbidity with multiple repeat hepatectomies.
Long-term outcomes of repeat hepatectomy
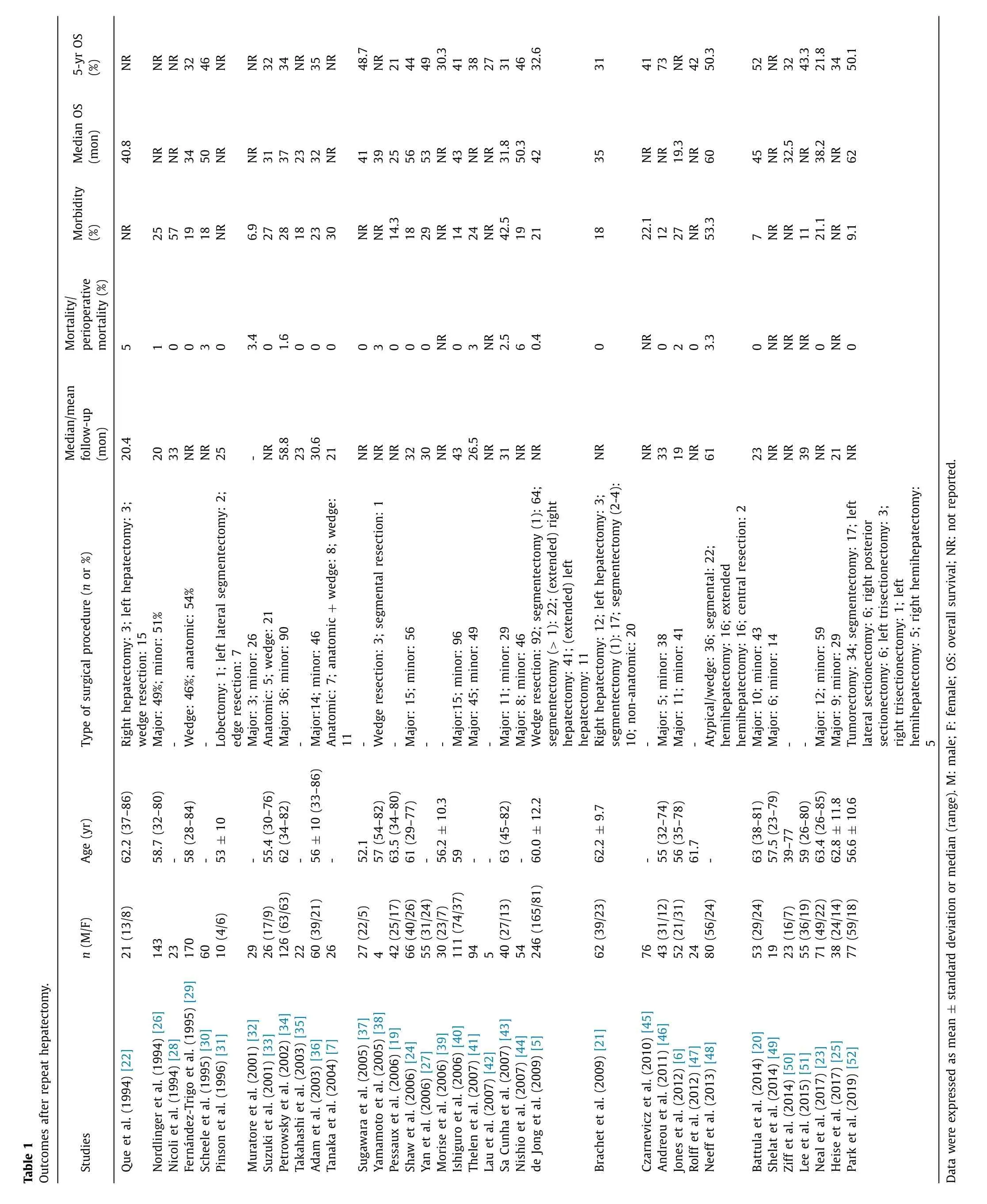
In the earliest study in the 1990s,when hepatic recurrence was found to be the main cause of treatment failure,repeat hepatectomy was performed in 21 patients with CRLM,with a reported median survival of 41 months and a 4-year survival rate of 43% [22].Furthermore,a cumulative rate of progression at 2 years after repeat hepatectomy was reported,which may have been due to limited margins after the initial hepatectomy and sparing of the vascular and biliary structures to maintain residual liver functions [22].Regardless of this limitation,the survival benefits were better than those of the palliative approaches available.In a subsequent French multi-institutional study,130 patients underwent 143 repeat hepatectomies for recurrent CRLM,116 of them had liver-only recurrence,and the estimated 2-and 3-year survival rates after the second resection were 57% and 33%,respectively [26].Subsequent to these studies,single-center and multicenter retrospective studies have reported survival outcomes after repeat hepatectomy,with a median overall survival(OS) ranging from 19.3 to 62 months and a 5-year OS of 21%–73%(Table 1) [5-7,19-52].The 5-year OS rates for the first,second,and third repeat hepatectomies were 33%,21%,and 36%,respectively,in a retrospective study [19],and another study reported 5-year OS rates of 40%,31%,and 44% after the first,second,and third hepatectomies,respectively [21].
As an alternative to hepatectomy,ablation is a minimally invasive approach that provides regional control of CRLM in patients who are unfit or unwilling to undergo major abdominal surgery [53].However,the therapeutic value of radiofrequency ablation (RFA) versus hepatectomy in CRLM remains controversial.In a meta-analysis of 14 studies,patients with CRLM undergoing hepatectomy experienced longer OS and progression-free survival than those treated with RFA,although ablation reduced morbidity [54].Another systematic review further confirmed that patients undergoing hepatectomy had significantly better OS and disease-free survival and a lower local recurrence rate than those undergoing RFA [55].The study suggested that ablation techniques should be used as an adjunct to surgery and not as single-modality treatment in patients with resectable CRLM for better long-term outcomes [55].The European Society for Medical Oncology (ESMO)consensus guidelines also recommend ablation with surgery to achieve an R0 resection and minimize the removal and destruction of healthy parenchyma associated with anatomical resection [15].Similar results can also be expected in patients with recurrent CRLM.A retrospective study stratified the OS of patients with recurrent CRLM by subsequent treatment and found that patients undergoing repeat hepatectomy had slightly higher 5-year OS than those undergoing RFA (70.0% vs.47.4%),but no statistically significant difference was observed,which might be due to the small sample size [11].In general,repeat hepatectomy is preferred in terms of survival benefits,and ablation can be used as a supplement to surgery.
Survival-related factors
Owing to the changes caused by initial resection and other therapeutic management strategies,the prognostic factors predicting survival after repeat hepatectomy might include factors related to initial and repeat hepatectomy [13].
Commonly reported prognostic factors
R0 resection during repeat hepatectomy has been reported to be associated with better survival outcomes [43].Although a 1-cm rule for a cancer-free resection margin in patients with CRLM was previously considered the minimum requirement for curative resection,the latest evidence suggests that a 1-mm cancer-free resection margin is sufficient to achieve a 5-year disease-free survival of 33% for CRLM,and an extra margin width does not provide additional survival benefits [56,57].Thus,achieving a margin greater than 1 mm may not be necessary for repeat hepatectomy.The carcinoembryonic antigen (CEA) level was also found to predict survival,where CEA >5 ng/mL at initial or repeat hepatectomy was associated with poorer survival [21,27,58,59].Other factors,including the presence of extrahepatic disease at repeat hepatectomy,a short disease-free interval (<6 or 12 months) between initial and repeat hepatectomy,the number (>1) and size (≥5 cm) of hepatic lesions at repeat hepatectomy,and the need for blood transfusion at repeat hepatectomy,have also been frequently reported to be poor prognostic factors [4,5,17,21,23,32](Fig.1).A study further suggested that a lack of adjuvant chemotherapy after initial hepatectomy and primary right-sided tumors were poor prognostic factors after repeat hepatectomy [60].Patients presenting with multiple poor prognostic factors tend to have a worse survival rate,which was confirmed by a retrospective study reporting high 5-year OS after repeat hepatectomy in patients with no risk factors(62%),followed by those with one (38%),two (19%) and all three risk factors (0) [40].

Fig.1.Prognostic factors and possible strategies.CEA: carcinoembryonic antigen;PSH: parenchyma-sparing hepatectomy;IOUS: intraoperative ultrasound.
Parenchyma-sparing hepatectomy (PSH)
In recent years,PSH has been proposed to preserve uninvolved functional liver parenchyma and is associated with fewer postoperative complications,uncompromised survival outcomes,and increased feasibility of future resections.The surgical principle involves the minimum sufficient surgical margins that can preserve maximum functional liver parenchyma [61].The findings based on 7081 patients in a meta-analysis by Deng et al.revealed a similar positive margin rate between the PSH and non-PSH groups [62].Similarly,in studies by Memeo et al.[63]and Margonis et al.[64],patients with CRLM undergoing PSH were compared to those undergoing non-PSH,and they showed similar rates of radical resection.
Most surgeons suggest repeat hepatectomy to achieve negative margins,preserving 30% of the functional liver remnant with sufficient vascular supply and biliary drainage [13].To reduce postoperative risks and improve outcomes,some studies emphasize performing PSH at the time of both initial hepatectomy and repeat resections,as well as adaptive techniques based on the size and site of recurrence to control intraoperative bleeding and hepatectomies at specialized liver surgery centers [13,65].In general,with improvements in surgical techniques and perioperative management,complications and mortality related to hepatectomy have been significantly reduced.
Recently,more emphasis on tumor biology rather than surgical margins as a reason for recurrence has led to a change in the surgical paradigm.In addition to increasing the scope for repeat hepatectomy in cases of recurrence,PSH,if combined with generally other local control strategies such as ablation,may also provide comparable long-term outcomes [66].A retrospective study from The University of Texas MD Anderson Cancer Center verified that patients with CRLM who underwent PSH had better survival than those who underwent non-PSH,especially from the date of diagnosis of the second hepatic recurrence (5-year OS: 73.6% vs.30.1%)owing to the greater chance of repeat hepatectomy [11].
Occult lesions and intraoperative ultrasound (IOUS)
Occult lesions are difficult to detect during routine radiological assessment and are considered one of the reasons for increased recurrence rates after initial resection in CRLM.IOUS is an effective method for the detection of CRLM [67],which has been reported to detect previously undetectable lesions that may change the surgical and therapeutic strategies and to reduce the early hepatic recurrence rate [28,68,69].Overall,10%–20% of patients have additional lesions identified with IOUS,whereas approximately 30% of patients have a change in the surgical strategy attributed to IOUS [59,70-73].IOUS not only helps detect additional liver metastases but also facilitates visualisation of vascular structures adjacent to the tumor during surgery,thus helping the surgeon’s decision-making to reduce blood loss during resection [59].Furthermore,tumor visualization using IOUS helps surgeons achieve negative resection margins and determine whether to follow parenchymal-preserving techniques based on feasibility,which improves disease-free survival [59].Hence,IOUS is suggested during hepatectomy.
Perioperative chemotherapy in repeat hepatectomy of CRLM
As previous studies have reported,patients with early recurrence tend to have unfavorable tumor biology for prognosis [38,39].The definition of early recurrence generally varies in studies from <6 months up to 2 years [58,69,74-77].A liver survey-based study of 6025 patients found that the 5-year survival was comparatively lower in patients with early recurrence(<6 months) than in patients with late recurrence (26.9% vs.49.4%) [69].The inability of most of the patients to undergo a repeat resection for recurrence within 6 months may explain the poor survival of patients with early recurrence to some extent [31,59].In the LiverMetSurvey study,36.6% of patients with early recurrence underwent repeat hepatectomy,with a 5-year OS of 47.2%,and those who had received chemotherapy before early recurrence resection showed further improvement in survival (5-year OS: 61.5% vs.43.7%),especially those who responded to preoperative chemotherapy (5-year OS: complete/partial 63.0% vs.stable/progressive 46.5%) [69].In another study by Adam et al.[78],patients with a tumor response to a fluorouracil-based chemotherapeutic regimen had better survival than those without a tumor response.The study also suggested that tumor progression after chemotherapy might be a contraindication for hepatectomy.This evidence suggests that chemotherapy can act as a test for the biological behavior of tumors with the goal of avoiding unnecessary surgery,and a multimodal approach involving aggressive chemotherapy and repeat hepatectomy might be the treatment of choice for patients with early recurrent CRLM.
In a study by Truant et al.[79],the prognostic factors for poor survival in patients with CRLM were related to aggressive tumor biology.A severe metastatic burden (CRLM size,number and synchronicity),the node status of the colorectal tumor and the presence of a rectal primary tumor played a role in the outcomes of CRLM.Therefore,identification of patients with molecular subsets of CRLM and subsequent prediction of the treatment response and OS improvement are essential to achieve the benefit of perioperative treatment.Evidence for the benefits of perioperative chemotherapy in CRLM patients with late hepatic recurrence is lacking;however,the beneficial role of perioperative chemotherapy in initial hepatectomy has been substantiated by the EORTC 40 983 study [80].Considering the presence of poor prognostic factors and occult lesions mentioned above,a multimodal treatment approach including repeat hepatectomy and chemotherapy warrants consideration in selected patients.Moreover,regional lymph node metastasis was reported to be more frequently observed in patients undergoing their second,third,and fourth hepatectomies(13.3%,25.0%,and 66.7%,respectively),rendering the curability of each hepatectomy more elusive [81].Although chemotherapy can control micrometastasis,which may contribute to better survival,it may also lead to liver damage,which might not be desirable for repeat hepatectomy.Therefore,the application of perioperative chemotherapy should be considered carefully.
Conclusions
Screening and appraisal of the evidence were performed nonsystematically,representing a limitation to the study.Nevertheless,the study showed that despite specific technical challenges,repeat hepatectomy can be considered a relatively safe and effective treatment for resectable,recurrent CRLM.Risk stratification based on the presence or absence of prognostic factors and formulation of a clinical risk score for repeat hepatectomy might assist in selecting patients for repeat hepatectomy and may improve short-and longterm outcomes.Moreover,multimodal approaches combining ablation techniques and innovative surgical methods such as PSH may also improve survival outcomes.Diagnostic modalities,including IOUS,may facilitate the identification of occult lesions,which can also lead to better R0 resection rates and longer OS.All the above approaches combined with appropriate perioperative chemotherapy may improve overall patient outcomes after repeat hepatectomy.
Acknowledgments
We thank Long-Hai Feng and Meng Chen for their scientific support to this manuscript.
CRediTauthorshipcontributionstatement
Jia-MinZhou:Data curation,Formal analysis,Investigation,Writing– original draft.LuWang:Conceptualization,Funding acquisition,Supervision,Writing– review &editing.An-RongMao:Conceptualization,Methodology,Project administration,Writing–review &editing.
Funding
This study was supported by a grant from the National Natural Science Foundation of China (No.81874182).
Ethicalapproval
Not needed.
Competinginterest
No benefits in any form have been received or will be received from a commercial party related directly or indirectly to the subject of this article.
 Hepatobiliary & Pancreatic Diseases International2023年6期
Hepatobiliary & Pancreatic Diseases International2023年6期
- Hepatobiliary & Pancreatic Diseases International的其它文章
- A new prognostic model for drug-induced liver injury especially suitable for Chinese population
- Post-hepatectomy liver failure: A timeline centered review
- INSTRUCTIONS FOR AUTHORS
- Older liver grafts from donation after circulatory death are associated with impaired survival and higher incidence of biliarynon-anastomotic structure
- Development and validation of a novel model to predict liver-related mortality in patients with idiosyncratic drug-induced liver injury
- Clinical-radiomics predictors to identify the suitability of transarterial chemoembolization treatment in intermediate-stage hepatocellular carcinoma: A multicenter study
