Flashback phenomenon and residual neurological deficits after the use of "bath salt" 3, 4-methylenedioxypyrovalerone
Aaron R. Mangold, Thomas P Bravo, Stephen J. Traub, Steven A. Maher, Christopher A. Lipinski,4
1Department of Dermatology, Mayo Clinic, Phoenix, Arizona, USA
2Department of Neurology, Mayo Clinic, Phoenix, Arizona, USA
3Department of Emergency Medicine, Mayo Clinic Hospital, Phoenix, Arizona, USA
4Department of Pharmacology, Mayo Clinic, Phoenix, Arizona, USA
Corresponding Author:Christopher A. Lipinski, Email: Lipinski.christopher@mayo.edu
Flashback phenomenon and residual neurological deficits after the use of "bath salt" 3, 4-methylenedioxypyrovalerone
Aaron R. Mangold1, Thomas P Bravo2, Stephen J. Traub3, Steven A. Maher3, Christopher A. Lipinski3,4
1Department of Dermatology, Mayo Clinic, Phoenix, Arizona, USA
2Department of Neurology, Mayo Clinic, Phoenix, Arizona, USA
3Department of Emergency Medicine, Mayo Clinic Hospital, Phoenix, Arizona, USA
4Department of Pharmacology, Mayo Clinic, Phoenix, Arizona, USA
Corresponding Author:Christopher A. Lipinski, Email: Lipinski.christopher@mayo.edu
BACKGROUND:The use and abuse of designer drugs has been recognized for decades; however there are many derivatives of compounds that make their way into the community. Abuse of compound(s) known on the street as "bath salt" is on the rise.
METHODS:We report the case of a 33-year-old man who complained of "flashbacks" and right arm shaking that followed a night of "bath salt" snorting. The active compound methylenedioxypyrovalerone methamphetamine (MDPV) was confirmed; however, analysis of three different "bath salt" products showed difference in their active components.
RESULTS:The patient's symptoms remained stable and he was discharged home after observation in the emergency department with instructions to return for any symptom progression.
CONCLUSION:Practitioners should be aware of the abuse of the compounds and that not all "bath salt" products contain MDPV.
Residual neurological deficits; Methylenedioxypyrovalerone methamphetamine; Emergency Department
INTRODUCTION
Designer drugs are chemical substances generally used for recreational purposes, but have no legitimate medicinal assignment.[1]The term "designer" signifies that the chemical compound represents a derivative of a controlled substance, one that is illicit, or sometimes to subvert a legal ban.[2]The 1980s saw the parallel emergence of designer derivatives of the opiate class (e.g. alpha-methyfentanyl, or "China white") and mescaline/phenethylamine class (e.g. methamphetamine, methylenedioxypyrovalerone methamphetamine [MDMA, or "ecstasy"]). The phenethylamine derivatives differ in the neuropharmacological effects they induce.[3]Amphetamine and methamphetamine are primarily potent central nervous system stimulants; whereas those compounds more chemically reminiscent of mescaline, such as MDMA, produce "entactogenic" effects. An entactogen (or empathogen) is a compound that induces feelings of "empathy" in the user.[4]Owing to their structural conservation to amphetamine, these molecules also have potent stimulant properties that make them useful as "party" or "rave" drugs of abuse. Current understanding of the mechanism of action of phenethylamines suggests that they alter primarily the dopaminergic/norepinephrine and serotonergic circuitry of the central nervous system by altering the neuronal cytoplasmic distribution(indirectly increasing synaptic concentrations) in the case of dopamine and norepinephrine[5]and activate the serotonergic 5-HT2A and 5-HT2C receptors.[6]Whether MDPV shares similar pharmacological activities is not yet known.
MDPV is the methylenedioxy ring substituted analog of the FDA schedule V drug pyrovalerone (Centroton, Thymergix) used infrequently in a medicinal capacity for the treatment of chronic fatigue or lethargy. MDPV wasfirst synthesized and patented in 1969 by Boehringer Ingelheim and was found to act as a norepinephrine (NE) and dopamine (DA) reuptake inhibitor.[7]The drug was originally used for the treatment of lethargy and chronic fatigue in the 1970s but was taken off of the market secondary to issues with abuse and dependence.[8]The recreational abuse of MDPV first started appearing in drug forums and chat rooms in 2005, and was later identified and seized by German customs officials in Saxony, Germany (2007) from a shipment originating from China. MDPV was first discovered by U.S. Customs agents in 2008.
In recent years, "bath salt" abuse in the United States has risen dramatically and various case reports show the dangers of chronic consumption and acute intoxication.[9–11]Users of these compounds experience symptoms of sympathetic arousal, delirium, and psychosis in acute intoxication. However, the long-term sequelae remain speculative. Moreover, the assumption is that products sold as "bath salts" contain as their active ingredient MDPV. To date, no cases have reported post intoxication neurological impairment or episodic recurrence, "flashbacks", of the previously intoxicated state. Here we describe a 33-year-old male patient presenting subacutely who claimed to have snorted a MDPV-containing "bath salt" called "Eight Ballz", obtained from a local "head shop". We briefly review the pertinent chemistry, pharmacology, and management of patients abusing MDPV.
CASE REPORT
A 33-year-old man with a history of polysubstance abuse, seizures secondary to traumatic brain injury, and hormonal transgender therapy presented to the emergency department (ED). He complained of episodes described as "spacing out" one day following intoxication with "bath salts". The patient reported snorting lines of a "bath salt" product called 8 Ballz every two-to-three hours, for a total of twelve hours. He stopped taking the drug approximately 36 hours prior to ED presentation. The patient was found to be tachycardic, diaphoretic, and euphoric during the period of intoxication. He denied any hallucinations. These symptoms lasted for one-totwo hours requiring repeat doses of the drug to maintain this "high" sensation. Within hours of the last dose, the patient felt disoriented, mildly depressed, and had difficulty in sleeping. Beginning approximately 12 hours after intoxication, the patient began to have two distinct sequelae. First, he had an episode with blurred vision, tachycardia, diaphoresis, confusion, and recurrence of depressive symptoms. Second, he complainted of "flashback" episodes every one-to-two hours prior to presentation to the ED. He described the flashbacks as reliving of the snorting of the drug, as though he was "back there". Beginning after the "flashbacks", the patient had episodes of spasticity beginning in the left hand and progressing to the left and right legs. This spasticity would last approximately 5 or 10 minutes and did not occur in conjunction with the "flashback" symptoms. During both types of episodes, the patient had no loss of consciousness, tongue biting, or visual disturbances. Upon arrival to the ED, the patient was complaining of wordfinding difficulty. He had a history of polysubstance abuse, including cannabis, GHB, ecstasy, methamphetamines, and cocaine. However, this is the first time the patient had used "bath salts." The patient denied concomitant use of any other illicit drugs in the last several months. He had seizures secondary to head trauma 4 years before, but was not on anti-epileptic medications.
Laboratory studies including a complete blood count, comprehensive metabolic panel, coagulation studies, urinalysis, and creatinine kinase were all unremarkable.Importantly, urine screening for substances of abuse was negative for cannabinoids, cocaine metabolite, amphetamines, tricyclic antidepressants, opiates, phencyclidine, and benzodiazepines. Magnetic resonance imaging (MRI) of the brain with and without contrast was unremarkable, except for a 1 cm pineal cyst. The patient was discharged home with extensive counseling regarding the dangers of "bath salts" and drug abuse. We purchased a 500 mg vial of "Eight Ballz" from the head shop that the patient reported purchasing the "Eight Ballz" from that he nasally insufflated. GC-MS analysis (Mayo Clinic, Rochester, MN) identified the sample as containing MDPV and benzocaine.
DISCUSSION
This case of "bath salt" intoxication represents a "variation on the theme" of designer drug abuse presentations. On the street, the assumption is that these products contain MDPV, which also goes by peevee, magic, or super coke. MDPV is a phenethylamine whose use is most commonly associated with hallucinatory delirium, psychiatric disturbances, and dysphoria.[9–11,16,17]Figure 1 illustrates the similarities between phenethylamine compounds that confer some similar pharmacology, but clearly some mechanistic differences must exist that account for varying "highs".[14]Users of MDPV report that the stimulant effects of the molecule are the most prevalent and similar to methylphenidate at dose ranges of 100–200 mg and cocaine at higher doses. These dose ranges may not however be usable for the "seasoned" consumer as the actual active compound, percentage composition of the active, and additional active components likely vary substantially between products and preparations. Three different "bath salts" products (Eight Ballz, Rave On, and Crazy Train) were analyzed by GC-MS and found that two contained MDPV and the third contained 4-fluoroamphetamine ("Flux"). Additionally, caffeine and benzocaine were also found in some of these products, but not all.
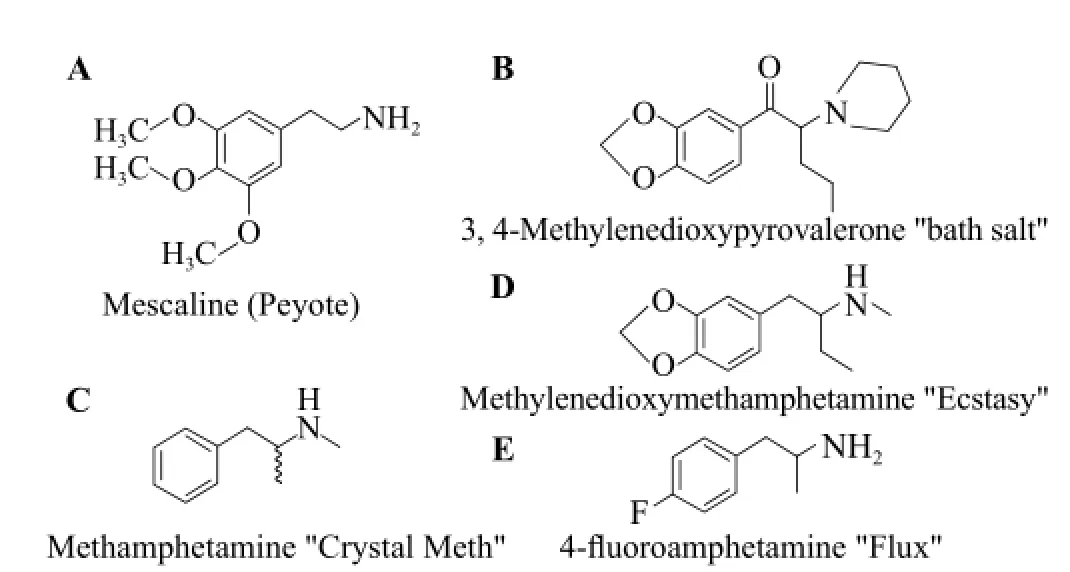
Figure 1. Chemical structures of several phenethylamines. The methylenedioxy-group phenyl-adduct of MDMA (B) and MDPV (D) renders these compounds structurally similar to mescaline (A). The phenethylamine backbone of MDMA and MDPV shares homology with amphetamine (C) as does 4-fluoroamphetamine (E).
Our patient reportedly ingested 2/3 of the 500 mg vial of "Eight-Ballz", or approximately 333 mg total, over 12 hours with each administration approximately 80 mg. However since we have not determined the MDPV percentage by weight in this product, the actual pharmacological dosage is suspected. He described "cocaine-like" effects, but suggested that the effects were much longer than he had experience with cocaine. It is likely that the addition of benzocaine to these products simulates the topical anesthetic properties found with nasal insufflation of cocaine. The drug induced "flashback" phenomena, which could have occurred either from the drug or from partial seizures (reported episodes of "hand shaking"). An MRI of the brain was essentially normal and ruled out a structural correlate for palsy of the right abducens nerve and postulated that this resulted from his previous traumatic injury to the brain.
The toxicological similarities exist between various phenethylamine/mescaline designer drugs, including methamphetamine, MDMA, and MDPV. Patients often present with features of adrenergic overstimulation including tachycardia, hypertension, agitation, hyperpyrexia, diaphoresis, mydriasis, and muscle rigidity. Treatment of the acutely intoxicated patient is mainly supportive with expected toxicity lasting in the range of hours. Hypertensive emergencies are best managed with benzodiazepines, followed if necessary, by vasodilators such as nitroglycerine, nitroprusside, or an alphaadrenergic blocking agent such as phentolamine. A report by Gay and Brown suggests that the mixed alpha-beta receptor blocker labetalol might also be effective, however many physicians avoid any beta-adrenergic blocking agent in such patients.[12]A recent report suggested that labetalol was superior to diltiazem in managing hypertensive crisis related to ingestion of adrenergic stimulant designer drugs.[13]Seizures and/or agitation are best managed with benzodiazepines (lorazepam). It has been suggested that protracted delusions or hallucinations can be managed with benzodiazepines, and can also be managed with perphenazine (Trilafon), clonidine, or roboxetine (Edronax). All patients presenting after recreational use of MDPV should be evaluated for rhabdomyolysis, but practitioners should realize that not all "bath salts" necessarily contain their advertized or implied active ingredient.[15]
Funding:None.
Ethical approval:Not needed.
矿区内地层倾向,由北而南,总的作北北东、北东东、南东东、(最南端又略转为北东东)的逐渐变化。倾角一般较缓(<30°),并由南西向北东地层递次变新,构成了较明显的向北东倾伏之背斜转折构造,幅向呈北东-南西,即为三峰庵—内招溪背斜的一部分。因矿区处于背斜的南东翼,地层刚大体作近东缓倾斜的单斜产状。
Conflicts of interest:We have no conflicts of interest to report.
Contributors:Mangold AR proposed the study and wrote the paper. All authors contributed to the design and interpretation of the study and to further drafts.
REFERENCES
1 Buchanan J, Brown C. 'Designer drugs'. A problem in clinical toxicology. Med Toxicol Adverse Drug Exp 1988; 3: 1–17.
2 Maurer H, Kraemer T, Springer D, Staack R. Chemistry, pharmacology, toxicology, and hepatic metabolism of designer drugs of the amphetamine (ecstasy), piperazine, and pyrrolidinophenone types: a synopsis. Ther Drug Monit 2004; 26: 127–131.
3 Kalant H. The pharmacology and toxicology of ‘ecstasy' (MDMA) and related drugs. CMAJ 2001; 165: 917–928.
4 Nichols D. Differences between the mechanism of action of MDMA, MBDB, and the classic hallucinogens. Identification of a new therapeutic class: entactogens. J Psychoactive Drugs 1986; 18: 305–313.
5 Simantov R. Multiple molecular and neuropharmacological effects of MDMA (Ecstasy). Life Sci 2004; 74: 803–814.
6 Nash JF, Roth BL, Brodkin JD, Nichols DE, Gudelsky GA. Effect of the R(–) and S(+) isomers of MDA and MDMA on phosphatidyl inositol turnover in cultured cells expressing 5-HT2A or 5-HT2C receptors. Neurosci Lett 1994; 177: 111–115.
7 Koppe H. 1-(3',4'-Methylenedioxy-phenyl)-2-pyrrolidinoalkanones-(1). U.S. Patent 3478050, filed April 26, 1966, and issued November 11, 1969.
8 Gardos G, Cole J. Evaluation of provalerone in chronically fatigued volunteers. Curr Ther Res Clin Exp 1971; 13: 631–635.
9 Penders T, Gestring R. Hallucinatory delirium following use of MDPV: "bath salts." Gen Hosp Psych. 2011 Jul 13 [Epub ahead of print]
10 Antonowicz J, Metzger A, Ramanujam S. Paranoid psychosis by consumption of methylenedioxypyrovalerone: two cases. Gen Hosp Psych 2011 May 25 [Epub ahead of print]
11 Centers for Disease control and prevention. Emergency department visits after use of a drug sold as "bath salts"—Michigan, November 13, 2010-March 31, 2011. MMWR. 2011; 60: 624–627.
12 Gay G, Loper K. The use of labetalol in the management of cocaine crisis. Ann Emerg Med 1988; 17: 282–283.
13 Hoskins MH, Leleiko RM, Ramos JJ, Sola S, Caneer PM, Khan BV. Effects of labetalol on hemodynamic parameters and soluble biomarkers of inflammation in acute coronary syndrome in patients with active cocaine use. J Cardiovasc Pharmacol Ther 2010; 15: 47–52.
14 Monte AP, Waldman SR, Marona-Lewicka D, Wainscott DB, Nelson DL, Sanders-Bush E, et al. Dihydrobenzofuran analogues of hallucinogens. 4. Mescaline derivatives. J Med Chem 1997; 40: 2997–3008.
15 Baron M, Elie M, Elie L. An analysis of legal highs-do they contain what it says on the tin? Drug Test Anal. 2011 May 19. [Epub ahead of print]
16 Spiller HA, Ryan ML, Weston RG, Jansen J. Clinical experience with and analytical confirmation of "bath salts" and "legal highs" (synthetic cathinones) in the United States. Clin Toxicol (Phila) 2011; 49: 499–505.
17 Ross EA, Watson M, Goldberger B. "Bath salts" intoxication. N Engl J Med 2011; 365: 967–968.
Received November 4, 2013
Accepted after revision January 12, 2014
World J Emerg Med 2014;5(1):63–66
10.5847/ wjem.j.issn.1920–8642.2014.01.011
 World journal of emergency medicine2014年1期
World journal of emergency medicine2014年1期
- World journal of emergency medicine的其它文章
- Wilderness medicine
- Lean techniques for the improvement of patients'flow in emergency department
- The knowledge level offinal year undergraduate health science students and medical interns about cardiopulmonary resuscitation at a university teaching hospital of Northwest Ethiopia
- Strategic planning and designing of a hospital disaster manual in a tertiary care, teaching, research and referral institute in India
- Effects of early rehabilitation therapy on patients with mechanical ventilation
- Bispectral index in predicting the prognosis of patients with coma in intensive care unit
