Time for a paradigm shift in the classi fication of muscle injuries
Bruce Hamilton,Juan-Manuel Alonso,Thomas M.Best*
aHigh Performance Sport New Zealand,Millennium Institute of Sport and Health,Mairangi Bay,Auckland 0110,New Zealand
bSports Medicine Department,Qatar Orthopaedic and Sports Medicine Hospital,Doha 22922,Qatar
cUHealth Sports Medicine Institute,University of Miami Miller School of Medicine,Miami,fl33136,USA
Time for a paradigm shift in the classi fication of muscle injuries
Bruce Hamiltona,b,Juan-Manuel Alonsob,Thomas M.Bestc,*
aHigh Performance Sport New Zealand,Millennium Institute of Sport and Health,Mairangi Bay,Auckland 0110,New Zealand
bSports Medicine Department,Qatar Orthopaedic and Sports Medicine Hospital,Doha 22922,Qatar
cUHealth Sports Medicine Institute,University of Miami Miller School of Medicine,Miami,fl33136,USA
Muscle injuries remain one of the most common injuries in sport,yet despite this,there is little consensus on how to either effectively describe or determine the prognosis of a speci fic muscle injury.Numerous approaches to muscle classi fication and grading of medicine have been applied over the last century,but over the last decade the limitations of historic approaches have been recognized.As a consequence,in the past 10 years, clinical research groups have begun to question the historic approaches and reconsider the way muscle injuries are classi fied and described.Using a narrative approach,this manuscript describes several of the most recent attempts to classify and grade muscle injuries and highlights the relative strengths and weaknesses of each system.While each of the new classi fication and grading systems have strengths,there remains little consensus on a system that is both comprehensive and evidence based.Few of the currently identi fied features within the grading systems have relevance to accurately determining prognosis.
©2017 Production and hosting by Elsevier B.V.on behalf of Shanghai University of Sport.This is an open access article under the CC BY-NC-ND license(http://creativecommons.org/licenses/by-nc-nd/4.0/).
Classi fication;Grading;Magnetic resonance imaging;Muscle injury;Return to play;Ultrasound
1.Introduction
Muscle injury remains one of the most common injuries in sport and of the muscle groups,the hamstrings are the most frequently injured.1–6In sports medicine,the ability to accurately diagnose,manage,and prognosticate,are routine expectations of practitioners.While numerous muscle injury classi fication and grading systems exist,there remains limited evidence or consensus on how to either describe a speci fic muscle injury,or determine the prognosis of any given injury, and this remains a frustration for both the clinician and the athlete.7
Injury“classi fication”refers to the process of describing or categorizing an injury(such as by its location,mechanism,or underlying pathology),while a“grade”provides an indication of severity.7While from the perspective of athletes and coaches the most relevant measure of injury severity is the length of time taken to return to full sports participation,severity may also be determined by symptoms,signs,and imaging findings.While the ability to predict return to play(RTP)is an expectation placed upon practitioners working with athletes,there is still incomplete evidence upon which to base decisions.8–12
In 1966,the American Medical Association(AMA)published a clinical grading system for muscle injuries as a means for determining injury severity.13Despite lacking an evidence base,the categorical grading approach of the AMA has remained popular and until recently largely unchanged in mainstream medical literature(Table 1).
More recently,speci fic clinical features such as the nature of pain onset,localised tenderness,pain severity,time to walk pain free,active range of motion of the knee and playing position in football,have all been identi fied as potential predictors of hamstring muscle injury severity,although the findings have been inconsistent,unreplicated,and often with limited relevance across all athletic levels of play.14–24For example,while time to walk pain free may be associated with either an early(less than 40 days)or late(greater than 40 days)RTP,25this duration is perhaps irrelevant in elite or competitive sport where a much more detailed prognosis is required,and where time for RTP may be expected to be signi ficantly less.26
The availability of magnetic resonance imaging(MRI) and ultrasound(US)imaging in the 1990s allowed for thevisualisation of underlying detail of muscle pathology,previously only speculated upon through clinical assessment.Radiologists could quickly correlate clinical findings with imaging characteristics and established early categorical radiological grading systems.27–30However,the initial literature was limited by small sample sizes and constrained by the clinical muscle injury grading paradigm established in the pre-imaging era. Typically the imaging systems lacked any data supporting a relationship between imaging appearance and prognosis.29–31
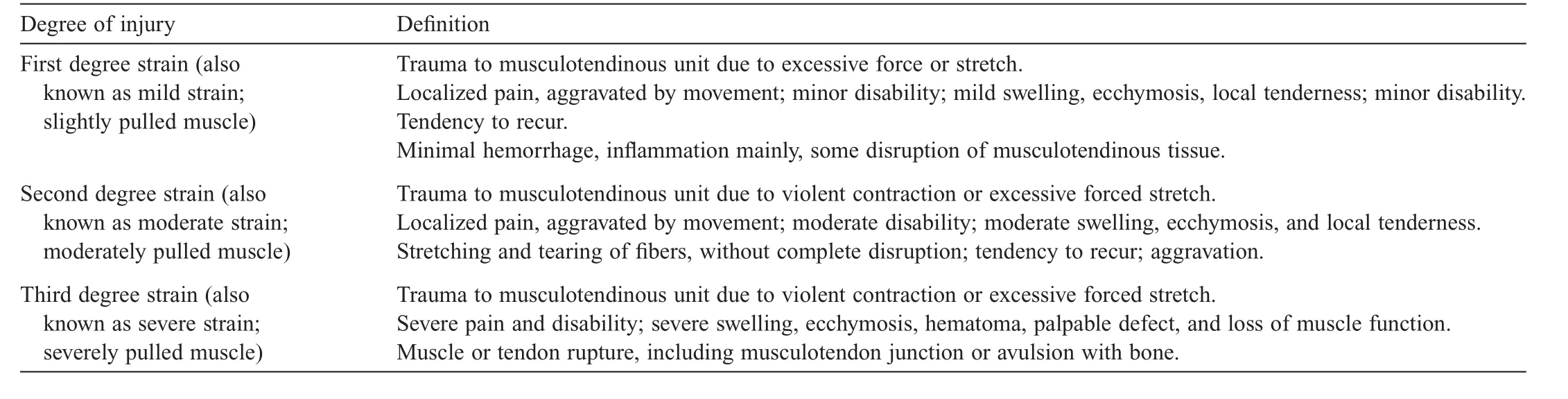
Table 1 Typical 1960-era muscle injury classi fication(based upon the American Medicine Association system for muscle injury classi fication).13
More recently,researchers have attempted to correlate categorical MRI grading systems27,28with clinical outcome.9,32Using a large cohort of professional footballers,Ekstrand et al.9observed that Grade 0(MRI negative for any observable abnormality)had a signi ficantly better prognosis than all other grades of injury,corroborating the findings of previous authors.18,19,22,23,33,34Later work from the same research group found a statistically signi ficant difference in clinical outcome between MRI determined Grades 1 and 2 muscle injury,with the authors concluding that traditional image-based categorical grading has prognostic validity.32However,while statistically signi ficant differences in RTP duration were documented,the wide variance observed in this measure likely limits the clinical utility of this approach,particularly in those settings where accurate prognostication is typically demanded by coaches and athletes.35
The early 21st century has seen increased cohort sizes utilised to evaluate the prognostic validity of both clinical and imaging observations.Typically estimated from MRI,injury length,cross-sectional area,and estimated volume of muscle injury have all been proposed as indicators of hamstring injury severity with larger lesions requiring a longer rehabilitation period.18,19,21,22,24Recently,a single study has highlighted that over and above any of the previously described radiological features,damage to the intra-muscular tendon may be the single most relevant predictor of RTP duration.8However,limitations in the design of the majority of MRI-based studies,including a high risk of bias,36means that many of these proposed prognostic indicators require further validation.
In recent years,there has been increasing attention and effort directed at developing a standardized and practical muscle injury classi fication and grading system.The purpose of this study was to review the recently proposed muscle injury classi fication and grading systems to identify areas of commonality and difference with the intent of identifying key gaps in our current knowledge.Speci fically,attention will be paid to the recently proposed Munich consensus,37British athletics,38and FC Barcelona39classi fications,as well as 2 additional novel radiological classi fications.40,41
2.Modern muscle injury classi fication systems
2.1.Munich consensus system
The Munich consensus statement resulted from a 1-day meeting of international clinical and basic science experts.37Based on the experience of the attendees,and the results of 19 completed pre-meeting questionnaires,the authors described a comprehensive classi fication and grading system for muscle injury.
The classi fication initially distinguishes direct(contusion and laceration)from indirect muscle injury.Indirect muscle injuries are then classi fied as either functional or structural injuries,sub-classi fied further into a type of injury,and finally sub classi fied into either a diagnostic group(e.g.,fatigue induced muscle disorder;delayed onset muscle soreness (DOMS);or muscle or spine related neuromuscular disorder)or severity grade(minor partial,moderate,subtotal,complete,or avulsion).Each classi fication or grade is provided with a de finition,as well as classical symptoms,signs,and imaging findings.A validation study con firmed that structural injuries (largely determined by those that are MRI positive for muscle damage)have a greater time loss than functional injuries,and that moderate and sub or total injuries have a worse prognosis than minor partial muscle tears.42
The Munich consensus approach addresses muscle injury in a comprehensive manner,which includes the incorporation of acute,overuse,direct,and indirect injury descriptors.In this regard,the Munich consensus may be considered a highly comprehensive approach to the study of muscle injury.
Underlying the construction of this classi fication and grading system are principles and assumptions that are not universally accepted.For example,the use of the term functional in this classi fication has a speci fic meaning,quite distinct to its use in other areas of medicine and as a result its application remains challenging to traditionally conservative practitioners.43While the use of the term“functional injuries”may be clinically appealing,there remains only limited academicbasis upon which to base functional diagnoses such as“spine-related neuromuscular muscle disorder”and“musclerelated neuromuscular muscle disorder”.44It could be argued that the microscopic damage and in flammatory response observed DOMS suggests that it would be more appropriately classi fied as a structural injury.Similarly,because edema reflects cellular activity,any condition determined as functional (by the de finition of Munich consensus being MRI negative for a muscle“tear”),but which has edema present raises the question of whether there is cellular or anatomic damage inherent in the process,and therefore could be considered structural in nature.Furthermore,the Munich consensus does not allow for the potential of focal structural muscle damage to exist below the current resolution of the MRI.
Of note,for the non-contact muscle injuries,the Munich consensus utilizes a mixed approach of 3 classi fications.37Minor and moderate partial tears(Type 3A and 3B)are differentiated taxonomically from subtotal muscle tears or tendinous avulsions(Type 4).There is no distinction based on the speci fic tissue involved,rather the separation is based on the extent of the injury as determined by imaging and clinical appearance, and bears many similarities to the nomenclature of the 1960s.13
In the authors’own validation of their work,MRI was performed in 215 of the 393 recorded injuries.42Unfortunately, the MRI report was only available in 52 of the 215 cases, making any assessment of the validity of the relationship between clinical and radiological validation questionably limited.
A closer look at the minor partial(3A),moderate(3B),and subtotal tears reveal RTP durations of 3–132 days,8–111 days, and 52–61 days,respectively.These data suggest a broad range of outcomes for each classi fication,and therefore limited value from a prognostic perspective,particularly in the distinction between Grades 3A and 3B.42Similarly,while there was a difference between average outcomes for functional and structural injuries,the range of RTP outcomes(functional 1–100 days,structural 2–156 days)suggests ongoing dif ficulty with effectively predicting outcome in any given individual.Hence, many functional injuries may have a worse prognosis than structural injuries,challenging the prognostic and pathologic validity of the initial classi fication.
MRI negative injuries were shown to have an improved prognosis relative to muscle“tears”,but there was no prognostic distinction between the speci fic sub-classi fications of functional injury.Taken together,there appears rationale from a prognostic perspective for distinguishing between MRI negative,minor or moderate tears,and complete tears of the muscle, but currently no prognostic justi fication for distinguishing categories of injury beyond this.
2.2.British athletics system
Utilizing their experience working with elite track and field athletes,Pollock et al.38proposed a novel classi fication system speci fically for non-contact muscle injuries.The authors describe a system that initially Grades injury 0–4 based on a combination of clinical and MRI quanti fied features,before sub-classifying the injury to re flect the principle anatomic structures involved.Speci fically,Grades 1–3 are sub-classi fied into“a”,“b”,or“c”to re flect myofascial,muscle tendon junction,or intra-tendinous tears(the latter only found in Grade 3 injuries).
Grade 0 injuries are considered those injuries that are MRI negative,thereby re flecting either a“focal neuromuscular injury”or muscle injury consistent with DOMS.The additional differentiator of“N”may be applied when there is a“suspicion of a neural component”to the injury.As described by Pollock et al.,38Grades 1–3 injuries re flect small,moderate,or extensive“tears”respectively to the muscle tissue,as primarily determined by the extent of edema and tissue disruption,but also by the tissue involved.Grade 4 injuries are considered complete tears to either the muscle or the tendon.
A subsequent study performed by the authors illustrated acceptable levels of intra-and inter-rater reliability.45In order to validate the grading system,the authors retrospectively reviewed the medical records of 44 athletes sustaining 65 hamstring injuries,assessing the time to return to full training (TRFT)and recurrence rate versus the grade of injury.46MRI negative(Grade 0)injuries were associated with a shorter TRFT than all other injury grades.Grades 1 and 2 injuries did not differ in TRFT,but Grade 3(extensive injuries)and intra-tendinous injuries had a prolonged TRFT.Furthermore, intra-tendinous injuries were associated with a higher risk of recurrence than any other classi fication.No Grade 4 injuries were reported.
Pollock et al.38developed a novel system for both classi fication and grading of non-contact muscle injuries in track and field athletes,speci fically relevant to the hamstring muscle.The degree of anatomic detail provided by the system is intuitively attractive and may be relevant for determining best practice treatment modalities.The approach has been shown to be reliable and is based upon the available evidence of prognostic elements involved in muscle injury.
By allocating a Grade 0,the authors recognize that noncontact muscle injuries are not limited to either acute stretch or contraction related injury,but also incorporates distinct etiological processes such as DOMS(Grade 0b).Etiologically and pathologically,DOMS is a distinct classi fication from Grade 0a (the latter believed to re flect either microscopic muscle damage or nerve“irritation”)and Grades 1–4,which re flect degrees of pathologic and radiological severity of the same injury type.It is of note that Pollock et al.38chose to classify 2(presumably) distinct etiological and pathologic processes together,seemingly on the basis of the MRI negative status and the known prognostic implications of outcome-negative MRI,re flecting a mixed approach to grading and classi fication.
By contrast,contusions(which could also be graded in terms of both imaging and outcome-based severity),are ignored in this model of muscle injury(but relevant in sports such as football).The non-inclusion of contusion injury in this system presents as a limitation to its broader application beyond hamstring injuries.
The authors have been unable to demonstrate a difference in prognosis between Grades 1(small tear)and 2(moderate tear), or between myofascial and myotendinous junction injuries. Grade 3(extensive tear)to the muscle and intra-tendinous inju-ries had a worse prognosis than all other grades but no other characteristics of the classi fication were able to discriminate RTP duration.46Hence,while anatomic classi fication and subclassi fication appears of scienti fic and academic interest,the results of their own validation process highlight that from the perspective of both prognosis and re-injury,a more limited grading process that incorporates Grade 0,Grade 1(mild to moderate),and Grade 2(severe)(there were no Grade 4 cases to consider),with a sub-classi fication of intra-tendinous injuries only could be considered.
2.3.Barcelona system
The Medical Department of FC Barcelona in collaboration withinternationalcolleagueshaverecentlyproposeda consensus-based classi fication for muscle injury.39Utilizing the participants,clinical experience they propose a muscle injury classi fication and grading system based on 4 taxonomic layers. Based on clinical history,the first identi fier distinguishes the mechanism of injury as either direct(D)or indirect(I),with indirect injuries additionally identi fied as sprinting or stretch related.The second and third major identi fiers are MRI variables describing the anatomic location and grade of the injury, respectively.The grade of the injury is determined by speci fic characteristics of edema and hemorrhage,and the crosssectional area of signal hyper-intensity.The final identi fier(R) relates to the re-injury status.
The stated purpose of this work was to create a classi fication system that effectively describes muscle strain injuries with clinically relevance and prognostic value and is easy to utilize and learn.39The authors attempted to avoid areas of limited evidence by avoiding language such as tear and strain,eliminating descriptors of MRI negative injuries,and identifying predictive elements with injury history and imaging finding that have a relatively strong evidence base.
Unique to this system is the incorporation of re-injury status into the grading.While not necessarily directly related to injury severity and therefore RTP durations,the presence of recurrent re-injury may in fluence rehabilitation progression and RTP decisions,and likely re flect an important adjunct.
While the detailed approach to the injury description supports the effective understanding of the injury nature as a result of the comprehensive nature of its approach,there exists a complexity in the nomenclature utilized that may limit the attractiveness of the system to the broader sports medicine community.To date,there remains no radiological reliability or validity study on the potential of this system to provide distinguishing prognoses.
2.4.Chan system
Based primarily on the authors,experience and incorporation of continuous data from previous imaging studies,Chan et al.40have proposed a 3-layered anatomic classi fication system to enhance the traditional grading systems available for muscle injury.The novel aspects of this classi fication pertain to the accurate MRI-based description of the injuries’anatomic location.Initially radiologically classi fied as proximal musculotendinous junction(MTJ),muscle,or distal MTJ,the injury is then further sub-classi fied as proximal,middle,or distal, before being de fined by the principle tissue involved;speci fically,intramuscular,myofascial,myofascial or perifascial, myotendinous,or combined.
Primarily an image-based classi fication system,this approach restricts its remit to acute non-contact muscle injuries and attempts primarily to add anatomic diagnostic clarity.40Despite this goal,there is no descriptor for primary tendon injury,and as such it is unclear where a proximal or distal muscle tendon rupture,where the rupture may occur proximal or distal to the MTJ of the muscle,would be considered. Furthermore,the use of the terminology“MTJ”and“myotendinous”at the first and third levels of classi fication respectively is somewhat confusing,and the system makes no allowance for the extent of injury observed.Finally,it is unclear how the anatomic classi fication is applied when more than one muscle is involved,which is a frequent occurrence.47
Beyond the value of accurate injury description,the authors provide no evidence that this approach will enhance patient management.At this stage,the combination of anatomic clarity and historical grading proposed has no inherent validity for predicting outcome and appears to have limitations in its capacity to incorporate the range of muscle injuries observed.
2.5.Cohen system
Cohen et al.41developed a hamstring injury classi fication system for professionalAmerican football players that incorporates a novel scoring system based on age and a range of MRI variables.Speci fically,the MRI variables included in the scoring system were the number of muscles involved(1–3), location(proximal,middle,or distal),insertional involvement (yes or no),cross-sectional percentage of muscle involvement, amount of muscle retraction(cm),and long-axis muscle involvement.Each variable was allocated a score and the total score considered for severity assessment.
To assess the validity of their proposal,Cohen et al.41performed a retrospective analysis of 43 National Football League injuries over a 10-year period,assessed the relationship between their“total MRI score”,and the number of games lost to injury. The authors concluded that a rapid RTP was more likely in those injuries with an MRI score of less than 10,compared to a score of greater than 10.Indicators of a poor prognosis included multiple muscle involvement,a higher percentage(>75%)of transverse muscle involvement,more than 10 cm of craniocaudal involvement,and muscle retraction.Ultimately,they concluded that their MRI score was useful in determining injury severity and predicting RTP duration in professional footballers.
The work of Cohen et al.has several key limitations,including its 10-year retrospective nature,limited subject numbers, lack of detail regarding the RTP process and to date no external validation.
3.Discussion
Many examples exist in sports medicine where there is little consensus on systems for injury classi fication.Two of the perhaps more high visibility examples of this challenging dilemma include non-contact anterior cruciate ligament injuries and stress fractures.48As with the muscle injury classi fication systems described herein,approaches to classi fication of these 2 injury types emphasize imaging and anatomy,with little focus on clinical parameters.We contend that a lack of universally accepted classi fication in key areas of sports injury represents an important de ficit in the field that warrants immediate attention.Until the criteria for classi fication are clearly de fined, clinicians and investigators alike will be unable to contribute in a compelling way to advance our understanding of the prevention,diagnosis,and treatment of muscle injury because they cannot evaluate whether studies are comparing“apples and oranges”.Each of the classi fications discussed were developed after careful consideration,review of previous literature,and synthesizing their own experiences,and yet the variation in outcome is evident from the above discussion.Each system has merit and it is not our intention to criticize the approach of the authors,rather to highlight ongoing challenges that would bene fit from further consideration.
Although there is some agreement between systems regarding the features that comprise the classi fication and grading approaches(Table 2),there is discordance with regard to the use of language,inclusion of clinical criteria,and,to date,inconsistency in both reliability and validity evaluation.
For a classi fication or grading system to be valid,there should be a testable rationale for each taxonomic subclassi fication.For grading of homogenously classi fied injuries, the validity equates to assessment of injury severity,which may be determined in a range of means,from the intensity of symptoms or signs,degree of abnormality on imaging,or most importantly from the duration required to RTP.
Only the Munich consensus system and Barcelona system incorporate a comprehensive,multi-faceted approach to the description of all muscle injuries.For example,contact type muscle injuries may account for up to 8%of muscle injuries,3have a distinct etiology,clinical appearance,imaging and pathologic appearance,and treatment from non-contact injuries.By not incorporating non-contact injuries into a classi fication system, the application of that system may be limited.38,40,41
While the broader elements of the Munich consensus, British athletics,and Barcelona systems may be quite distinct,on closer inspection components of their approaches are remarkably similar(Table 3),as seen in the terminology utilized in the grading of sprint type MRI positive muscle injury.
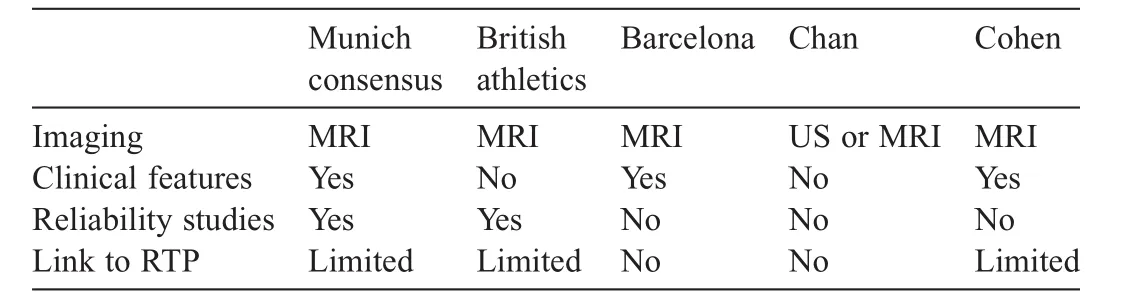
Table 2 Comparison of features of modern muscle injury classi fication systems.

Table 3 Summary of 3 currently utilized muscle grading systems.
Both the British athletics and Barcelona systems have the apparent advantage of sub-classi fication of muscle injury into the speci fic tissue involved within each grading level.However, the validation study of Pollock et al.38has suggested that there is no prognostic advantage to this approach,beyond identifying intra-muscular tendon involvement.46This is consistent with previous data,which show the strongest associations with RTP being MRI negative or positive status18,19,22,23,33,34and the involvement of the intra-muscular tendon.8However,while increased anatomic detail in the classi fication and grading systems may not relate to prognostic validity,this does not invalidate the approach.It is possible that this enhanced detail will facilitate appropriate injury understanding,allow enhanced homogeneity of injury groups,and allow for tissue-speci fic treatment strategies to be developed,challenged,and enhanced.
MRI negative muscle injuries are recognized to have a favorable outcome in comparison to MRI positive injuries18,19,22,23,33,34and the Munich consensus,37Barcelona,39and British athletics38systems all account for this important differentiator in their approach.Failure to incorporate acute,MRI negative injuries into a classi fication system is a signi ficant limitation to its effectiveness,given that up to 14%of clinically diagnosed muscle injuries may be of this type.23While the Barcelona system makes no attempt to distinguish the etiology of MRI negative injury,the Munich consensus system provides a detailed breakdown of potential etiology and pathology of injury in the absence of local MRI findings.Similarly,the British athletics classi fication of MRI negative injuries differentiates DOMS from either microscopic(i.e.,below the sensitivity of MRI)muscle damage or peripheral nerve irritation.38While DOMS is well established diagnostically,pathologically, and from a management perspective,49the remaining proposed MRI negative diagnoses do not have the same underlying academic rigor.
A signi ficant ongoing challenge facing the establishment of any consensus on the nomenclature for muscle injury is a consistent approach to language.As can be seen above,there are broad similarities in the understanding of the classic sprintinginjury but variability in the descriptions applied(e.g.,tear, strain,injury).The Munich consensus statement argued against the use of strain to describe non-contact muscle injury due to its confusing history and implied etiology,and preferentially utilize the term tear.37The use of“tear”is also the preferred approach of the British athletics system,while Chan continues to utilize strain,and both Barcelona and Cohen utilize the neutral term“muscle injury”.Given the current knowledge constraints,we consider that“muscle injury”appears the most pervasive term for this most common of injuries.
However,there remain signi ficant areas of divergence in language that may not be so easily reconciled.These include the use of non-standardized terminology such as functional, muscle-related neuro muscular disorder,and other diagnoses that potentially re flect the range of experience of clinicians involved in the classi fications development and other factors that may challenge consensus.43
The ability to provide an accurate estimate of RTP duration is a fundamental rationale for classifying and grading muscle injuries.However,it is well recognized that the RTP process is multi-factorial,involving not only pathophysiological healing times,but also social and psychological factors.50This more comprehensive paradigm is not accounted for in any of the systems we have discussed herein.Furthermore,it appears counterintuitive that a single time point assessment of an injury,no matter how comprehensive,provides an accurate prediction of an RTP time some weeks into the future.Indeed, Wangensteen et al.12illustrated that the initial history and physical examination may only account for 29%of variation in RTP duration following hamstring muscle injury.The addition of MRI to this clinical assessment accounted for only a total of 31%of RTP variability.Furthermore,Jacobsen et al.11have shown that serial assessment enhances the accuracy of RTP estimates beyond the value of an initial evaluation.11However, while evidence based,this approach may not be aligned with the expectations of athletes and coaches,who typically expect accurate predictions of RTP duration early in the recovery from injury.As such,practitioners have traditionally simpli fied muscle injuries into categorical taxonomies that neither exist pathologically nor have any validity in assessing RTP.
4.Conclusion
As this review illustrates,on the basis of increased MRI technology and availability and ongoing challenges of high injury rates,a range of classi fication and grading systems for muscle injury have been proposed.Each of these systems has unique strengths,weaknesses,and ability to be incorporated into widespread use,but the inconsistencies in approach to muscle injury description currently available continue to thwart a universal approach to addressing muscle injury prognostication and management effectively.
The prediction of RTP in the acute,MRI positive muscle injury continues to be a challenge,and to date,none of the described classi fication and grading systems effectively address this.Only MRI negative status and the involvement of intramuscular tendon have been consistently illustrated to impact RTP duration,and yet a range of anatomic factors are described in the increasingly complex systems included in this review. Given the multi-factorial complexity of RTP decisions,the continuous nature of anatomic injury severity,and the range of healing times associated with different tissues involved in muscle injury,the categorical approach to muscle injury grading,for the purposes of predicting RTP duration,is unlikely to be successful.
We propose that while establishing a uniform classi fication system for muscle injuries must be a priority for sports medicine,its approach should be targeted to facilitating optimal management strategies rather than attempting to predict RTP durations.The clear description of anatomy and pathology through careful history,examination,and appropriate imaging will facilitate an accurate management strategy for every injury. In addition,we propose that careful serial clinical assessments and shared decision making in the process of RTP will move us closer to our target of an accurate prediction for time to RTP. While this approach may not satisfy the expectations of coaches and athletes for an immediate prognosis,it is consistent with the current evidence.
Authors’contributions
BH,JMA,and TMB all participated in the drafting,writing, and revisions of the manuscript.All authors have read and approved the final version of the manuscript,and agree with the order of presentation of the authors.
Competing interests
The authors declare that they have no competing interests.
1.Bennell KL,Crossley K.Musculoskeletal injuries in track and field: incidence,distribution and risk factors.Aust J Sci Med Sport 1996;28: 69–75.
2.Brooks JH,Fuller CW,Kemp SP,Reddin DB.Incidence,risk,and prevention of hamstring muscle injuries in professional rugby union.Am J Sports Med 2006;34:1297–306.
3.Ekstrand J,Hagglund M,Walden M.Epidemiology of muscle injuries in professional football(soccer).Am J Sports Med 2011;39:1226–32.
4.Ekstrand J,Hagglund M,Walden M.Injury incidence and injury patterns in professional football:the UEFA injury study.Br J Sports Med 2011;45: 553–8.
5.Gabbe B,Finch C,Bennell K,Wajswelner H.Risk factors for hamstring injuries in community level Australian football.Br J Sports Med 2005;39: 106–10.
6.Hawkins RD,Fuller CW.A prospective epidemiological study of injuries in four English professional football clubs.Br J Sports Med 1999;33: 196–203.
7.Hamilton B,Valle X,Rodas G,Til L,Grive RP,Rincon JA,et al. Classi fication and grading of muscle injuries:a narrative review.Br J Sports Med 2015;49:306.
8.Comin J,Malliaras P,Baquie P,Barbour T,Connell D.Return to competitive play after hamstring injuries involving disruption of the central tendon.Am J Sports Med 2013;41:111–5.
9.Ekstrand J,Healy JC,Walden M,Lee J,English B,Hagglund M. Hamstring muscle injuries in professional football:the correlation of MRI findings with return to play.Br J Sports Med 2012;46:112–7.
10.Schut L,Wangensteen A,Maaskant J,Tol JL,Bahr R,Moen M.Can clinical evaluation predict return to sport after acute hamstring injuries?A systematic review.Sports Med 2017;47:1123–44.
11.Jacobsen P,Witvrouw E,Muxart P,Tol JL,Whiteley R.A combination of initial and follow-up physiotherapist examination predicts physiciandetermined time to return to play after hamstring injury,with no added value of MRI.Br J Sports Med 2016;50:431–9.
12.Wangensteen A,Almusa E,Boukarroum S,Farooq A,Hamilton B, Whiteley R,et al.MRI does not add value over and above patient history and clinical examination in predicting time to return to sport(RTS)after acute hamstring injuries:a prospective cohort of 180 male athletes.Br J Sports Med 2015;49:1579–87.
13.Rachun A.Standard nomenclature of athletic injuries.1st ed.Chicago,IL: American Medical Association;1966.p.157.
14.Askling C,Saartok T,Thorstensson A.Type of acute hamstring strain affects flexibility,strength,and time to return to pre-injury level.Br J Sports Med 2006;40:40–4.
15.Askling CM,Tengvar M,Saartok T,Thorstensson A.Acute first-time hamstringstrainsduringslow-speedstretching:clinical,magnetic resonance imaging,and recovery characteristics.Am J Sports Med 2007;35:1716–24.
16.Askling CM,Tengvar M,Saartok T,Thorstensson A.Acute first-time hamstring strains during high-speed running:a longitudinal study including clinical and magnetic resonance imaging findings.Am J Sports Med 2007;35:197–206.
17.Balius R,Maestro A,Pedret C,Estruch A,Mota J,Rodriguez L,et al. Central aponeurosis tears of the rectus femoris:practical sonographic prognosis.Br J Sports Med 2009;43:818–24.
18.Connell DA,Schneider-Kolsky ME,Hoving JL,Malara F,Buchbinder R, Koulouris G,et al.Longitudinal study comparing sonographic and MRI assessments of acute and healing hamstring injuries.AJRAm J Roentgenol 2004;183:975–84.
19.Gibbs NJ,Cross TM,Cameron M,Houang MT.The accuracy of MRI in predicting recovery and recurrence of acute grade one hamstring muscle strains within the same season in Australian Rules football players.J Sci Med Sport 2004;7:248–58.
20.Peterson J,Thorborg K,Nielsen M,Skjodt T,Bolvig L,Bang N,et al.The diagnostic and prognostic value of ultrasonography in soccer players with acute hamstring injuries.Am J Sports Med 2014;42:399–404.
21.Schneider-Kolsky ME,Hoving JL,Warren P,Connell D.A comparison between clinical assessment and magnetic resonance imaging of acute hamstring injuries.Am J Sports Med 2006;34:1008–15.
22.SlavotinekJP,VerrallGM,FonGT.Hamstringinjuryinathletes:usingMR imaging measurements to compare extent of muscle injury with amount of time lost from competition.AJRAm J Roentgenol 2002;179:1621–8.
23.Verrall GM,Slavotinek JP,Barnes PG,Fon GT.Diagnostic and prognostic valueofclinical findingsin83athleteswithposteriorthighinjury:comparison of clinical findings with magnetic resonance imaging documentation of hamstring muscle strain.Am J Sports Med 2003;31:969–73.
24.Verrall GM,Slavotinek JP,Barnes PG,Fon GT,Esterman A.Assessment of physical examination and magnetic resonance imaging findings of hamstring injury as predictors for recurrent injury.J Orthop Sports Phys Ther 2006;36:215–24.
25.Guillodo Y,Here-Dorignac C,Thoribe B,Madouas G,Dauty M,Tassery F,et al.Clinical predictors of time to return to competition following hamstring injuries.Muscles Ligaments Tendons J 2014;4:386–90.
26.Hamilton B,Tol JL,Almusa E,Boukarroum S,Eirale C,Farooq A,et al. Platelet-rich plasma does not enhance return to play in hamstring injuries: a randomised controlled trial.Br J Sports Med 2015;49:943–50.
27.Peetrons P.Ultrasound of muscles.Eur Radiol 2002;12:35–43.
28.Peetrons P,Creteur P.Echographies et traumatismes musculaires aigus.In: Chevrot A,Kahn M,Morvan G,editors.Imagerie Des Parties Molles De L’Appareil Locomoteur:Sauramps Medical.Montpellier:Sauramps Medical;1993.p.229–35.
29.Pomeranz SJ,Heidt Jr RS.MR imaging in the prognostication of hamstring injury.Work in progress.Radiology 1993;189:897–900.
30.Takebayashi S,Takasawa H,Banzai Y,Miki H,Sasaki R,Itoh Y,et al. Sonographic findings in muscle strain injury:clinical and MR imaging correlation.J Ultrasound Med 1995;14:899–905.
31.Fleckenstein JL,Weatherall PT,Parkey RW,Payne JA,Peshock RM. Sports-related muscle injuries:evaluation with MR imaging.Radiology 1989;172:793–8.
32.Hallen A,Ekstrand J.Return to play following muscle injuries in professional footballers.J Sports Sci 2014;32:1129–36.
33.Verrall GM,Slavotinek JP,Barnes PG,Fon GT,Spriggins AJ.Clinical risk factors for hamstring muscle strain injury:a prospective study with correlation of injury by magnetic resonance imaging.Br J Sports Med 2001;35:435–9.
34.Askling CM,Tengvar M,Thorstensson A.Acute hamstring injuries in Swedish elite football:a prospective randomised controlled clinical trial comparing two rehabilitation protocols.Br J Sports Med 2013;47:953–9.
35.Reurink G,Whiteley R,Tol JL.Hamstring injuries and predicting return to play:‘bye-bye MRI?’.Br J Sports Med 2015;49:1162–3.
36.Reurink G,Brilman EG,de Vos RJ,Maas M,Moen MH,Weir A,et al. Magnetic resonance imaging in acute hamstring injury:can we provide a return to play prognosis?Sports Med 2015;45:133–46.
37.Mueller-Wohlfahrt HW,Haensel L,Mithoefer K,Ekstrand J,English B, McNally S,et al.Terminology and classi fication of muscle injuries in sport:the Munich consensus statement.Br J Sports Med 2013;47:342–50.
38.Pollock N,James SL,Lee JC,Chakraverty R.British athletics muscle injury classi fication:a new grading system.Br J Sports Med 2014;48: 1347–51.
39.Valle X,Alentorn-Geli E,Tol JL,Hamilton B,Garrett Jr WE,Pruna R, et al.Muscle injuries in sports:a new evidence-informed and expert consensus-based classi fication with clinical application.Sports Med 2016;doi:10.1007/s40279-016-0647-1
40.Chan O,Del Buono A,Best T,Maffulli N.Acute muscle strain injuries: a proposed new classi fication system.Knee Surg SportsTraumatolArthrosc 2012;20:2356–62.
41.Cohen SB,Towers JD,Zoga A,Irrgang JJ,Makda J,Deluca PF,et al. Hamstring injuries in professional football players:magnetic resonance imaging correlation with return to play.Sports Health 2011;3:423–30.
42.Ekstrand J,Askling C,Magnusson H,Mithoefer K.Return to play after thigh muscle injury in elite football players:implementation and validation of the Munich muscle injury classi fication.Br J Sports Med 2013;47: 769–74.
43.Tol JL,Hamilton B,Best TM.Palpating muscles,massaging the evidence? An editorial relating to‘Terminology and classi fication of muscle injuries in sport:the Munich consensus statement’.Br J Sports Med 2013;47: 340–1.
44.Orchard JW,Farhart P,Leopold C.Lumbar spine region pathology and hamstring and calf injuries in athletes:is there a connection?Br J Sports Med 2004;38:502–4.
45.Patel A,Chakraverty J,Pollock N,Chakraverty R,Suokas AK,James SL. British athletics muscle injury classi fication:a reliability study for a new grading system.Clin Radiol 2015;70:1414–20.
46.Pollock N,Patel A,Chakraverty J,Suokas A,James SL,Chakraverty R. Time to return to full training is delayed and recurrence rate is higher in intratendinous(‘c’)acute hamstring injury in elite track and field athletes: clinical application of the BritishAthletics Muscle Injury Classi fication.Br J Sports Med 2016;50:305–10.
47.Crema MD,Guermazi A,Tol JL,Niu J,Hamilton B,Roemer FW.Acute hamstring injury in football players:association between anatomical location and extent of injury-A large single-center MRI report.J Sci Med Sport 2016;19:317–22.
48.McInnis KC,Ramey LN.High-Risk stress fractures:diagnosis and management.PM R 2016;8(Suppl.3):S113–24.
49.Evans GF,Haller RG,Wyrick PS,Parkey RW,Fleckenstein JL. Submaximal delayed-onset muscle soreness:correlations between MR imaging findings and clinical measures.Radiology 1998;208:815–20.
50.Creighton DW,Shrier I,Shultz R,Meeuwisse WH,Matheson GO. Return-to-play in sport:a decision-based model.Clin J Sport Med 2010;20:379–85.
14 December 2016;revised 20 February 2017;accepted 10 March 2017
Available online 27 April 2017
Peer review under responsibility of Shanghai University of Sport.
*Corresponding author.
E-mail address:txb440@med.miami.edu(T.M.Best)
http://dx.doi.org/10.1016/j.jshs.2017.04.011
2095-2546/©2017 Production and hosting by Elsevier B.V.on behalf of Shanghai University of Sport.This is an open access article under the CC BY-NC-ND license(http://creativecommons.org/licenses/by-nc-nd/4.0/).
 Journal of Sport and Health Science2017年3期
Journal of Sport and Health Science2017年3期
- Journal of Sport and Health Science的其它文章
- Rehabilitation and return to sport after hamstring strain injury
- Risk factors for hamstring injuries in Australian male professional cricket players
- Relationships among hamstring muscle optimal length and hamstring flexibility and strength
- The effect of hamstring flexibility on peak hamstring muscle strain in sprinting
- Motivation dimensions for running a marathon:A new model emerging from the Motivation of Marathon Scale(MOMS)
- The ethics of exercise in eating disorders:Can an ethical principles approach guide the next generation of research and clinical practice?
