Rehabilitation and return to sport after hamstring strain injury
Lauren N.Erickson,Marc A.Sherry*
Sports Rehabilitation,University of Wisconsin Hospital and Clinics,Madison,WI 53718,USA
Rehabilitation and return to sport after hamstring strain injury
Lauren N.Erickson,Marc A.Sherry*
Sports Rehabilitation,University of Wisconsin Hospital and Clinics,Madison,WI 53718,USA
Hamstring strain injuries are common among sports that involve sprinting,kicking,and high-speed skilled movements or extensive muscle lengthening-type maneuvers with hip flexion and knee extension.These injuries present the challenge of signi ficant recovery time and a lengthy period of increased susceptibility for recurrent injury.Nearly one third of hamstring strains recur within the first year following return to sport with subsequent injuries often being more severe than the original.This high re-injury rate suggests that athletes may be returning to sport prematurely due to inadequate return to sport criteria.In this review article,we describe the epidemiology,risk factors,differential diagnosis,and prognosis of an acute hamstring strain.Based on the current available evidence,we then propose a clinical guide for the rehabilitation of acute hamstring strains and an algorithm to assist clinicians in the decision-making process when assessing readiness of an athlete to return to sport.
©2017 Production and hosting by Elsevier B.V.on behalf of Shanghai University of Sport.This is an open access article under the CC BY-NC-ND license(http://creativecommons.org/licenses/by-nc-nd/4.0/).
Acute;Muscle;Performance;Physical therapy;Recurrence;Re-injury;Thigh
1.Introduction
There is a wide spectrum of hamstring-related injuries that can occur in the athlete.These include hamstring strains,complete and partial proximal hamstring tendon avulsions,ischial apophyseal avulsions,proximal hamstring tendinopathy,and referred posterior thigh pain.1,2Of these,hamstring strains are the most prevalent hamstring-related injury resulting in loss of time for athletes at all levels of competition.1–7Acute hamstring strains often result in signi ficant recovery time and have a lengthy period of increased susceptibility for recurrent injury.4,8Approximately one-third of hamstring strains will recur,with the highest risk for injury recurrence being within the first 2 weeks of return to sport.2,4–9This high recurrence rate is suggestive of an inadequate rehabilitation program,a premature return to sport,or a combination of both.The consequences of recurrence are high as recurrent hamstring strains have been shown to result in signi ficantly more time lost than first time hamstring strains.10Therefore,the purpose of this review article was to provide a summary of the current evidence for clinicians to improve the quality of rehabilitation and decision-making for return to sport after a hamstring-related injury.
2.Epidemiology
There is an increased risk for acute hamstring strains in sports that involve sprinting,kicking,or high-speed skilled movements, such as football,soccer,rugby,and track,1,4,6–9,11–15and in sports that involve extensive muscle lengthening-type maneuvers,such as dancing.1,6,8Acute hamstring strains have been found to be more common in field sports(football,soccer,and field hockey) than in court sports(basketball,volleyball),7,9more common in competition than in practice,7,13,14and more common in preseason than regular season and postseason.7Most hamstring strains are from non-contact mechanisms7,14with the most common mechanisms being running and sprinting activities occurring during sport.7Male athletes are 64%more likely to sustain an acute hamstring strain than female athletes.7,9,12,15
A National Football League team published injury data, including data from preseason training camp from 1998 to 2007,and found that hamstring strains were the most common muscle strain and were the second most common injury,only surpassed by knee sprains.13Hamstring strains were most common in running backs,defensive backs or safeties,and wide receivers.13Injury data published from 51 professional soccer teams showed that hamstring strains were the most common injury,representing 12%of all injuries.14Track and field injury data from the Penn Relays Carnival showed that hamstring strains were the most common injury,accounting for24.1%of all injuries and greater than 75%of all lower extremity strain injuries.15
With running and sprinting being the most common activities of hamstring strain injury,identifying the alterations of gait mechanicsthatmayberesponsiblehasreceivedattention.During theterminalswingphaseoftherunninggaitcycle,thehamstrings incur the greatest stretch and are active,eccentrically contracting to decelerate the lower limb in preparation for foot contact.6,16–20It is important to note that hamstring length is not representative of muscle fiber strain.Fiorentino and colleagues19showed that whole- fiber length change relative to the musculotendon unit length change remains relatively constant with increasing speed; however,peak local fiber strain relative to the strain of the musculotendon unit increases with speed,with the highest peak local fiberstrainrelativetothewholemuscle fiberstrainoccurring at the fastest speed(100%maximum).Peak hamstring force and negative work also occur during this phase,most notably to the biceps femoris,and increase signi ficantly with speed.16–21Chumanovandcolleagues16showedthatpeakhamstringforceand negative work increased to the largest extent as sprinting speed wasincreasedfromsubmaximaltomaximalsprintingspeeds.The average peak net hamstring force and negative work increased from36N/kgand1.4J/kgat80%speedto52N/kgand2.6J/kgat 100%speed,respectively.Furthermore,Silder and colleagues22showedthatasspeedincreasedfrom80%to100%,bicepsfemoris activity during the terminal swing phase increased an average of 67%,while the semimembranosus and semitendinosus showed a 37%increase.The results of these studies offer insights and provide a possible explanation for the tendency of the biceps femoris to be more often injured than the semimembranosus and semitendinosus when running at high speed.In addition,these injuries typically occur along the intramuscular tendon and the adjacent muscle fibers.6,23
In sports that involve extreme stretching movements,such as dancing,the semimembranosus is more commonly involved. Injury data published by Askling and colleagues24on 15 professional dancers showed that all dancers were injured during slow hip flexion movements with knee extension,with the injury most commonly involving the semimembranosus(87%). More detailed anatomic and biomechanical studies are needed to further investigate the preference of injury to the semimembranosus vs.the semitendinosus and biceps femoris.These injuries typically occur more often at the proximal free tendon as opposed to the intramuscular tendon.2,6,24,25
3.Risk factors
Acute hamstring strains often result in signi ficant recovery time and have a lengthy period of increased susceptibility for recurrent injury.4,8Approximately one third of the hamstring injuries will recur with the highest risk for injury recurrence being within the first 2 weeks of return to sport.2,4–9This finding had led some to speculate that athletes may be returning to sport at a suboptimal level of performance due to ineffective rehabilitation or returning to sport prematurely due to inadequate return to sport criteria.2,4,6,7,11Several other factors likely contribute to the high rate of recurrent injury,such as persistent weakness in the injured muscle,reduced extensibility of the musculotendinous unit due to residual scar tissue,and adaptive changes in the biomechanics and motor patterns of sporting movements following the original injury.5,6
Previous research has identi fied multiple risk factors for hamstring injury.Non-modi fiable risk factors include older age and prior history of hamstring strain.1,26–32A prospective cohort study of male soccer players showed that 10.5%of players with a previous hamstring injury and 4.6%of players without a previous hamstring injury experienced a new hamstring injury during the season,indicating that athletes with a prior hamstring injury are at more than twice as high a risk of sustaining a new hamstring injury.28Modi fiable risk factors include hamstring weakness and fatigue,31–35imbalances in hamstring eccentric and quadriceps concentric strength,34,36,37decreased quadriceps flexibility,26reduced hip flexor flexibility,26and strength and coordination de ficits of the pelvic and trunk musculature.4,38–40It is speculated that addressing each of these modi fiable risk factors through rehabilitation programs could potentially decrease re-injury risk.Height,weight,and body mass index have been shown to have no in fluence on the incidence of hamstring strain injuries.29,30,41,42
4.Differential diagnosis
Determining the exact source of injury is critical in determining the most appropriate treatment and expediting safe return to play.Considering the potential causes of posterior thigh pain,the differential diagnosis for acute hamstring strain injury includes hamstring tendon avulsions,ischial apophyseal avulsions,proximal hamstring tendinopathies,and referred posterior thigh pain.
Complete and partial avulsions of the proximal hamstring tendon are uncommon injuries,but can occur during sporting activities that generate forceful hip flexion moments while the knee is extending.Common sporting mechanisms include water skiing,43–46bull riding,44tackling associated with rugby and football,47and slips or falls associated with cross-country and downhillskiing.46Theathletemayreportanaudiblepopandhave signi ficantpainwithimmediatelossoffunction.Theathleteoften presentswithaninabilityorsigni ficantdif ficultywithperforming apronelegcurl,aninabilitytofullyextendandbearweightonthe involved side,and signi ficant gait abnormality.44–47Acutely,signi ficantecchymosisandalargehematomaareseenintheposterior thigh46–48which will likely limit a clinician’s ability to discern a palpable defect.In the subacute and chronic phases,once the hematoma has resolved,a palpable defect is often noted with activeorresistedknee flexion,whichproducesadistalbulgeinthe retracted muscle.46–48Another way to assess hamstring tendon integrity in the acute phase is to evaluate for the presence of a positive bowstring sign(absence of palpable tension in the distal hamstring tendons when the knee actively holds a flexed position due to lack of proximal hamstring tendon integrity).43Magnetic resonance imaging(MRI)is the most accurate imaging modality for the diagnosis of proximal hamstring avulsions.46–49
Ischial apophyseal avulsions are more likely to occur in young athletes(13–16 years)when the apophysis has the least amount of bony bridging or fusion(open growth plate).49,50The mechanism of injury typically involves a forceful low-velocityoverstretch,often with combined hip flexion and knee extension, which is common in dance and kicking.49,50The athlete may report an audible pop and have deep achy pain,especially when sitting.49Clinical examination will likely reveal ischial tenderness,pain and weakness with strength testing of the hamstrings and gluteals,and pain with active and passive knee extension testing.Once pain has been controlled,length or flexibility testingofthehamstringsmayactuallyrevealnode ficitduetoloss of the hamstring origin anchor point.If an ischial apophyseal avulsion is suspected,an anteroposterior radiograph of the pelvis can be utilized for de finitive diagnosis.1,49
Proximalhamstringtendinopathy,orhighhamstring tendinopathy,is often insidious with a gradual onset of pain.51,52Pain in the proximal hamstring region is experienced during activity,when sitting on firm surfaces,or with prolonged sitting.51–53Evidence suggests that it more commonly affects middle-aged athletes52and endurance athletes(long distance runners,cross country skiers,and cyclists).51–53Most athletes with proximal hamstring tendinopathy have tenderness to palpation on the ischial tuberosity,local discomfort with minimal to no weakness of the hamstrings and gluteals,and local discomfort with flexibility testing with minimal to no limitation of hamstring length.51–53Speci fic clinical tests for high hamstring tendinopathy include the Puranen-Orava test,the bent-knee stretch test,and the modi fied bent-knee stretch test.54,55
Causes of referred posterior thigh pain include piriformis syndrome,neural tension,lumbar disc herniation,or lumbar facet syndrome,which causes nerve root compression,sacroiliac joint dysfunction,and spondylogenic lesions.53,56,57Athletes with referred posterior thigh pain will commonly have variable symptoms within the low back region,ranging from no back pain to signi ficant back pain.Other symptoms include posterior thigh muscle cramping and tightness,numbness,tingling,and shooting pain.53,56Clinical examination will likely reveal reduced range of motion(ROM)or pain provocation with movement of the lumbar spine,tenderness or stiffness over the lumbar intervertebral or sacroiliac joints,a positive slump test,or a positive lumbar quadrant test.56If clinical examination suggests a diagnosis of referred posterior thigh pain and advanced imaging for the hamstrings is negative, advance imaging for the spine may be warranted.
5.Prognosis
The severity of hamstring strains ranges on a continuum from very mild to very severe.When evaluating the prognosis for acute hamstring strains,important outcomes include potential time away from sport,return to pre-injury level of sport performance,and likelihood of re-injury.Attempts to determine the likelihood of these outcomes have centered on imaging of the injured muscle tendon unit,patient symptoms,speci fic clinical tests,and functional clinical tests.
Advancedmusculoskeletalimaging,includingMRIandultrasound,are being implemented in an attempt to better identify and determine prognosis.These techniques provide a more objective measure and are frequently used to assess the severity and extent of injury with professional athletes.MRI studies of hamstring strains indicate that the length and cross-sectional area of the injury are directly proportional to the time for recovery from injury,with increased length and cross-sectional area resulting in greater time for recovery.11,58–60However,multiple MRI studies demonstrate that the severity of the initial injury is ineffective in predicting re-injury.61,62Thus,MRI of hamstring strains appears usefulinestimatingtimeforrecoveryfrominjury,butislimitedin identifying individuals at risk for re-injury.Ultrasound as a prognosticindicatoroftimetorecoverfrominjuryshouldbeusedwith caution as a recent publication investigating soccer players with acutehamstringinjuriesshowednocorrelationbetweenlengthof injury area,injury severity,and time to return to play.63
Various clinical criteria,when assessed within the first 5 days of initial injury,have been associated with a long recovery time(>40 days to return to sport),such as an initial visual analog scale pain score of greater than 6,pain during everyday activities for more than 3 days,popping sound during the injury, bruising,and greater than 15°difference in passive straightening of the injured limb compared to the uninjured limb.64The time to walk test,which assesses an athlete’s ability to walk without pain post-injury,has also been used to assess recovery time.65,66Australian Rules football players taking more than 1 day to walk pain-free following injury were 4 times more likely to take longer than 3 weeks to return to sport when compared with those walking pain-free within 1 day.65
The active ROM test assesses an athlete’s ability to extend the knee while the hip is flexed at 90°in supine.Injury data published on 165 elite track and field athletes showed that athletes with a greater active knee extension ROM de ficit required longer recovery.67,68When comparing active knee extension ROM de ficit with full rehabilitation time,the average time to return to sport after initial injury was 6.9 days for<10° de ficit,11.7 days for 10°–19°de ficit,25.4 days for 20°–29° de ficit,and 55.0 days for≥30°de ficit.67,68This test is traditionally used to assess hamstring flexibility.The formation of scar tissue does not occur until the proliferation stage of tissue healing69and thus an acute active knee extension de ficit is most likely related to pain and neurophysiological mechanisms occurring during the in flammatory stage of tissue healing.
The resisted ROM test can be used to assess an athlete’s ability to resist knee extension at 90°,45°,and 15°of knee flexion in prone.54,70Based on the length-tension curve and the internal torque-joint angle curve,it is expected that the hamstrings will demonstrate the greatest force at 90°due to the hamstrings being at optimum length and leverage.71As the hamstrings are lengthened,such as when placed at 45°and 15°of knee flexion,the number of potential crossbridges decreases and the mechanical advantage decreases so that lesser amounts of active force are generated,even under conditions of full activation and effort.71,72Sole and colleagues72showed that athletes with a recent hamstring injury demonstrate signi ficantly decreasedknee flexiontorqueinthelengthenedrange of contraction(approximately 5°–25°knee flexion).Athlete’s demonstrating full isometric knee flexion force at 90°,with incremental reductions in isometric knee flexion force at 45°and 15°,haveabetterprognosisthanathlete’sdemonstratingreduced isometric knee flexion force at 90°with further incremental reductions in isometric knee flexion force at 45°and 15°.Thelatter scenario indicates that the athlete has reduced force output even when the hamstrings are at optimum length and leverage.
Thelocationofthepointofmaximumtendernesstopalpation relative to the ischial tuberosity is associated with the recovery time.The more proximal the site of maximum pain,the longer thetimeneededtoreturntopre-injurylevel.23,24,73Inaddition,the mechanism of injury and tissues injured have important prognostic value in estimating the duration of recovery needed to returntopre-injurylevelofperformance.23–25,73,74Injuriesinvolving the intramuscular tendon and the adjacent muscle fibers (such as the biceps femoris during high-speed running23,25)typically require a shorter recovery period than those involving the proximal free tendon(such as the semimembranosus during dance and kicking24,25,74).In 2007,Askling and colleagues23,24demonstrated that hamstring injuries occurring from sprintingtype activities resulted in an average of 16 weeks to return to pre-injury level in elite sprinters23whereas hamstring injuries occurring from stretching-type activities resulted in an average of 50 weeks to return to pre-injury level in professional dancers.24More recent data have demonstrated that return to sport may not be as lengthy as originally reported.In 2013, Askling and colleagues75demonstrated that hamstring injuries occurringfromsprinting-typeactivitiesresultedinanaverageof 23 days to return to sport whereas hamstring injuries occurring from stretching-type activities resulted in an average of 43 days to return to sport in elite football players.
Despite the differences in mechanism of injury,tissues involved,and recovery rates,current rehabilitation approaches do not differ greatly when treating high-speed running vs.overstretch injuries.2,75–77This topic is an area for future research and investigation as there seems to be room for developing rehabilitation exercises that are more speci fic with respect to injury type and location.Through examining the intensity and pattern of hamstring muscle activation in commonly used rehabilitation exercises,Mendiguchia and colleagues78have shown that different rehabilitation exercises affect different patterns of muscle recruitment and that the degree of response differs between proximal and distal regions.Although these conclusions are based on unpublished data,they may suggest that the prescribed intervention will depend on the injured muscle and its speci fic anatomic location.
6.Current evidence of rehabilitation program interventions
The primary goal of the rehabilitation for hamstring strain injury is to allow the athlete to return to sport at a level of performance before the injury with minimal risk of recurrence of the injury.To do so,a rehabilitation program should address modi fiable risk factors,such as hamstring weakness and fatigue;31–35,79imbalances in hamstring eccentric and quadriceps concentric strength;34,36,37decreased quadriceps flexibility;26reduced hip flexor flexibility;26and strength and coordination de ficits of the pelvic and trunk musculature.4,38–40Currently, there is no clear explanation or robust model that consistently demonstrates how all of these risk factors interact.Future research to look into the interrelationship between these different factors involved in hamstring strains would provide a better understanding of this multifactorial injury and may improve prevention and decrease risk for re-injury.
Arehabilitationprogramshouldaddresspsychosocial factors,such as fear and apprehension.Insecurity when performing a ballistic hamstring flexibility test has been observed at the time of return to sport testing despite having passed common clinical strength and flexibility tests.Speci fically,Askling and colleagues80showed that there was a feeling of insecurity when performing this test with the injured leg in 95%of athletes.
Without adequate rehabilitation,athletes may experience persistent weakness in the injured muscle,3,5,22,72,81–83reduced extensibility of the musculotendinous unit due to residual scar tissue,5,59,83–85and adaptive changes in the biomechanics and motor patterns of sporting movements due to altered neuromuscular control.5,16,22,72,83,86,87
San filippo and colleagues3showed de ficits in isokinetic knee flexion strength of the injured limb(9.6%de ficit in peak torque and 6.4%de ficit in work)at return to sport compared to the uninjured limb.Sole and colleagues72showed de ficits in eccentric flexor torque toward the hamstring lengthened range of the injured limb compared to the uninjured limb,especially in the fourth quartile(approximately 5°to 25°knee flexion).A recent study examining elite Australian footballers showed that previously injured athletes displayed smaller increases in eccentric hamstring strength compared with athletes who had no history of hamstring strain injuries.81A shift in the isokinetic knee strength pro file has been identi fied in previously injured limbs, indicating that athletes with a previous hamstring injury are at a greater than normal susceptibility for eccentric damage.88,89The mean optimum angle of peak torque for the previously injured hamstring muscles was at a signi ficantly shorter muscle length(12.1°±2.7°,i.e.,a more flexed knee)than for the hamstring muscles with no history of injury.88A shorter than normal optimum length means that more of the muscle’s working range is in the region of instability and damage on the length-tension curve,which could contribute to risk for re-injury.
Silder and colleagues85showed that increased mechanical strains arise near the proximal biceps femoris musculotendinous junction during relatively low-load lengthening contractions,and that subjects with a prior hamstring injury presented with signi ficantly greater muscle tissue strains when compared to those withoutapriorhamstringstrain.Scartissuehasbeenobservedas early as 6 weeks after an initial injury59and found to persist on a long-termbasis(atleast5–23monthspostinjury).84Scartissueis often observed along the musculotendinous junction adjacent to the site of prior injury,which may alter muscle contraction mechanics.In particular,the collagen fibers comprising remodeled tendon tend to be less well organized with different stiffness properties than normal tendon.84Speci fically,scar tissue may increase the overall mechanical stiffness of the tissue it replaces, whichmayrequirethemuscle fiberstolengthenagreateramount to achieve the same overall musculotendon length relative to the pre-injurystate.84Thissuggeststhatresidualscartissueatthesite of a prior musculotendon injury may adversely affect local tissue mechanics in a way that could contribute to risk for re-injury.
One of the most important components of rehabilitation is neuromuscular control.Sole and colleagues86showed that therewasanearlieronsetofactivationofthehamstringmusclesduring the transition from double-to single-leg stance in those with a previous hamstring injury compared to those without a previous hamstring injury.This suggests that there is an alteration in lower-limb proprioception and neuromuscular control following a hamstring injury.Neuromuscular control of the muscles affecting the length–tension relationship of the hamstrings based on their origin to the trunk and pelvis also needs to be addressed during rehabilitation.For example,Opar and colleagues15found that the incidence of hamstring strains in track and field athletes were signi ficantly greater in the 4×400 m relay when compared with the 4×100 m relay.This leads to speculation that there are important trunk and pelvic positional changes affecting the hamstrings that occur while sprinting on a curve vs.sprinting on a straightaway.The relationship between trunk and pelvic control to hamstring strain injury was con firmed by Chumanov and colleagues16,87who showed that the contralateral hip flexors(iliopsoas)have as large an in fluence on hamstring stretch as the hamstrings themselves.This in fluence occurs because the iliopsoas directly induces an increase in anterior pelvic tilt,which in turn necessitates greater hamstring stretch.Hip flexor muscle force induces hip flexion and a small amount of knee extension on the opposite limb,both of which act to increase hamstring stretch.Otherproximalmusclesaffectingpelvisposition,suchas the abdominal obliques and erector spinae,also substantially in fluence hamstring stretch.16,87This in fluence demonstrates the importance of inter-segmental dynamics in which muscles can generate substantial accelerations about joints they do not span.
Determining the type of rehabilitation program that most effectively promotes muscle tissue and functional recovery is essentialtominimizetheriskofre-injuryandtoimproveathlete performance.Both eccentric strength training10,23,24,36,90–92and neuromuscular control exercises4,38–40,86have been shown to reduce the likelihood of hamstring injury and are advocated by many as a part of the rehabilitation program following an acute hamstring strain.Askling and colleagues75,76demonstrated a signi ficant reduction in time to return to sport when individuals with an acute hamstring injury were treated using a program aimed at loading the hamstrings during controlled lengthening (eccentric)exercises(L-protocol)compared to a program with less emphasis on eccentric exercises(C-protocol).In addition to a conventional hamstring rehabilitation program,each protocol consistedof3differentexercisesuniquetoeachprotocol,where Exercise1wasaimedmainlyatincreasing flexibility,Exercise2 was a combined exercise for strength and trunk and pelvis stabilization,and Exercise 3 was more of a speci fic strength training exercise.All exercises were performed in the sagittal plane.In elite football players,75the L-protocol resulted in a mean of 28 days to return to sport and no re-injuries within 12 months whereas the C-protocol resulted in a mean of 51 days to returntosportand1re-injurywithin12months.Inelitesprinters and jumpers,76the L-protocol resulted in a mean of 49 days to return to sport and no re-injuries within 12 months whereas the C-protocol resulted in a mean of 86 days to return to sport and2re-injurieswithin12months.Onthisbasis,arehabilitation program consisting of mainly eccentric exercises is more effective than a rehabilitation program with less emphasis on eccentric exercises in promoting return to sport after acute hamstring injury.Proske and colleagues88have shown that the performance of controlled eccentric exercises can facilitate a shift in peak force development to longer musculotendon lengths.Their initial data suggest that the incorporation of such exercises into rehabilitation may reduce hamstring re-injury rates as this shift in peak force development may help to restore optimal musculotendon length for tension production.
One common criticism of rehabilitation programs that only emphasize eccentric strength training is the lack of attention to musculature adjacent to the hamstrings.Neuromuscular control of the lumbopelvic region has been indicated as an important component for optimal function of the hamstrings during sporting activities16,87and should be an integral part to a comprehensive rehabilitation program.Sherry and Best4demonstrated a signi ficant reduction in injury recurrence when individuals with an acute hamstring injury were treated using a progressive agility and trunk stabilization(PATS)program compared to a progressive stretching and strengthening(STST)program.The PATS program consisted of primarily neuromuscular control exercises,beginning with early active mobilization in the frontal and transverse planes,and then progressing to movements in the sagittal plane.The average time required to return to sport for athletes in the PATS group was 22.2 days,while the average time for athletes in the STST group was 37.4 days. Compared to the STST group,there was a statistically signi ficant reduction in injury recurrence in the PATS groups at 2 weeks(STST:54.5%vs.PATS:0%)and at 1 year(STST:70% vs.PATS:7.7%)after return to sport.
Silder and colleagues11compared the PATS program to a progressive running and eccentric strengthening(PRES) program.No signi ficant differences were found in time to return to sport when individuals with an acute hamstring injury were treated using a PATS program compared to a PRES program.The average time to return to sport for athletes in the PATS group was 25.2 days,while the average time for athletes in the PRES group was 28.8 days.Overall re-injury rates were low with 1 of 16 athletes in the PATS group and 3 of 13 athletes in the PRES group experiencing a re-injury within 12 months. Although both rehabilitation programs demonstrated excellent clinical results,no athlete showed complete resolution of injury as assessed on MRI following completion of rehabilitation despite meeting clinical clearance to return to sport(no pain, full ROM,and full strength).Therefore,regardless of the rehabilitation employed,clinical determinants of recovery as measured during the physical examination do not adequately represent complete muscle recovery and readiness for return to sport.This finding highlights the importance of a graduated return to the demands of full sporting activity and continued independent rehabilitation after return to sport to aid in minimizing re-injury risk.
Neural mobilization techniques have been recommended as part of the rehabilitation program if a positive active slump test is found during the examination.93For those diagnosed with a hamstring strain with mild disruption of the muscle fibers,the inclusion of the slump stretch has been shown to reduce time away from sport.94The use of neural mobilization techniques inthe rehabilitation of more severe hamstring strains has not been investigated.
7.Proposed rehabilitation guideline
A guideline was proposed for the rehabilitation of hamstring strain injury(see Appendix in online version)based on current available evidence,including the integration of components of the PATS and the PRES rehabilitation programs.2,4,6,11This rehabilitation guideline is divided into 3 phases,with speci fic treatment goals and progression criteria for phase advancement and returntosport.ThefocusforPhase1isminimizationofpainand edema,restoration of normal neuromuscular control at slower speeds,and prevention of excessive scar tissue formation while protecting the healing fibers from excessive lengthening.Phase 2 allows for increased intensity of exercise,neuromuscular trainingatfasterspeedsandlargeramplitudes,andtheinitiation ofeccentricresistancetraining.Phase3progressestohigh-speed neuromuscular training and eccentric resistance training in a lengthened position in preparation for return to sport.
Symptom exacerbation due to exercise intensity and ROM is a potential complication of this rehabilitation guideline.All exercises should be progressed based on the athlete’s tolerance and progression should be limited if the athlete reports pain,increased stiffness,or anxiety with movement.Clinical decision-making is crucial for safe progression of exercises without risking undue harm to the recovering athlete.It should be noted that this rehabilitation guideline(Appendix)is based primarilyontheliterature pertaining to hamstring strain injuries involving the intramuscular tendon and adjacent muscle fibers4,11,23,25,75,76,91as there is a lack of published rehabilitation programs for those that involve the proximal free tendon.Modifications to the exercises,sports-speci fic movement,and progression criteria may need to be considered for injuries involving the proximal free tendons of the hamstring muscles.
8.Factors and criteria for return to sport
Currently,there is no consensus within the literature concerningreturntosportdecision-makinggiventhelackofstandardization and clear objective criteria.Often times,recommendations are vague,stating that athletes can be cleared to return to sport once full ROM,strength,and functional abilities(jumping, running,and cutting)can be performed without complaints of pain or stiffness.95Askling and colleagues80reported that the clinical examination of the injured leg should reveal no signs of remaining injury.These signs include no pain on palpation of the injured muscle,no difference in manual muscle testing between legs with no pain provocation,and<10%de ficit with passive flexibility tests to that of the uninjured leg with no pain provocation.No pain on palpation of the injured muscle has been further validatedasanimportantcriteriaforreturntosportbyDeVosand colleagues,61whofoundthatathleteswithlocalizeddiscomforton hamstringpalpationattimeofreturntosportwerealmost4times more likely to sustain a re-injury compared with athletes with absenceofdiscomfortonpalpation.Arecentmeta-analysisfound that de ficits in isometric strength and flexibility tend to resolve within 20–50 days following initial hamstring strain injury; however,de ficits for dynamic measures of strength(concentric andeccentricstrength,conventionalandfunctionalhamstring-toquadricep strength ratios)were present at return to sport.82This evidence suggests that it may be appropriate to monitor isometric strength and flexibility throughout rehabilitation,while dynamic measures of strength may hold more value at return to play.
Isokinetic strength testing should be performed under both concentricandeccentricconditions.Malliaropoulosand colleagues68reported that isokinetic strength testing,measured at 60°/s and 180°/s,should result in a de ficit of less than 5%compared with the injured side for clearance to return to sport.Multiple studies have also reported on the hamstring-to-quadricep strengthratioandhavereportedthatlessthana5%bilateralde ficit should exist in the ratio of eccentric hamstring strength(30°/s)to concentric quadriceps strength(240°/s).3,96In addition,the knee flexionangleatwhichpeakconcentricknee flexiontorqueoccurs should be similar between limbs.88,89More speci fically,the angle ofpeaktorqueshouldbewithin5°2,72,89andthetimetopeaktorque should be within 10%2,86of the uninjured side.Delvaux and colleagues97found that muscle strength performance was the second most common criteria(most common criteria was completepainrelief)forreturntosportthatiscurrentlybeingusedby sportsmedicinecliniciansofprofessionalsoccerteams.Themost common methods of strength assessment were manual muscle testing(80%)and isokinetic strength testing(75%)with 40% assessing eccentric quadricep strength,60%assessing concentric quadricepstrength,75%assessingconcentrichamstringstrength, and 85%assessing eccentric hamstring strength.Although clinical research indicates comparison of a mixed ratio(eccentric hamstring strength to concentric quadriceps strength)to be the ideal method of assessment,only 30%of clinicians utilized this method.When assessing whether an athlete is ready to return to sport,57%of clinicians reported tolerating≤10%difference compared to the uninjured side whereas only 22%of clinicians reported tolerating≤5%difference compared to the uninjured side.Thissigni fiesthatthereisaclearlackofconsensusaboutthe choice of assessment parameters and the speci fic values for whether or not to return an athlete to sport.An effort should be made to integrate clinical research results with those in actual sports medicine practice.
The active hamstring test,or H-test,is completed by performing a straight leg raise as fast as possible to the highest point withoutfearofinjury.Asklingandcolleagues80foundafeelingof insecurity in 95%of the athletes when performing this test on the injured leg and that the mean angular hip flexion velocity was signi ficantly lower in the injured leg compared to the uninjured leg.If insecurity is reported while performing this test,it is recommended that an additional 1–2 weeks of rehabilitation be allowed and the test repeated.This process then continues until no insecurity is reported.75,76,80This test has been shown to be reliable and valid for detecting de ficits in athletes with hamstring strainsandprovidesusefuladditionalinformationtothecommon clinical examination before returning an athlete to sport.80
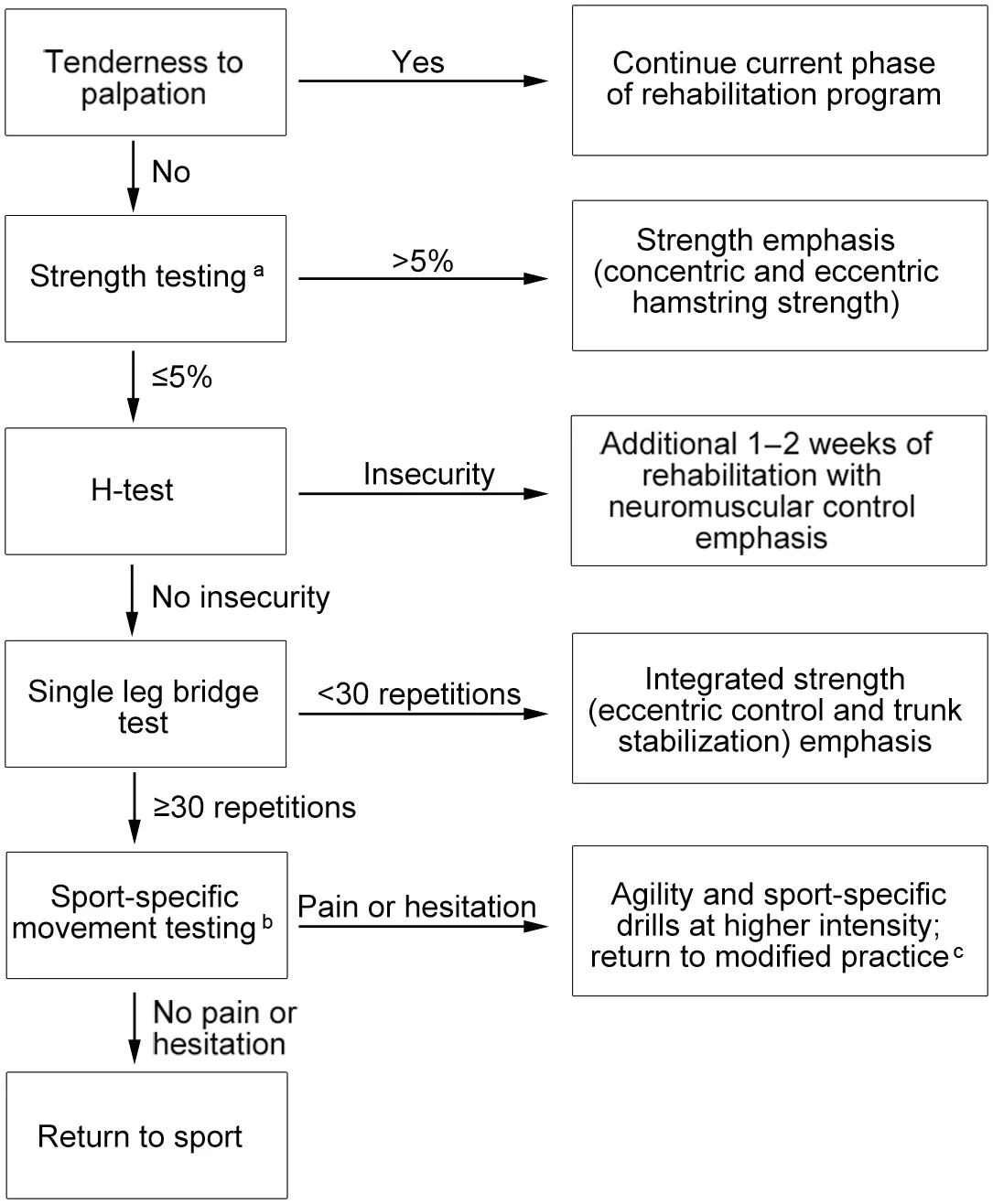
Fig.1.Algorithm for return to sport.aClinicians should utilize objective methodsofstrengthassessment,includingisokineticstrengthtesting (concentrichamstringstrength,eccentrichamstringstrength,eccentric hamstring strength to concentric quadriceps strength)or manual muscle testing with hand-held dynamometry or Kiio force sensors.bClinicians should incorporate movement speci fic to the athlete’s sport,which may include accelerations,decelerations,rotations,sprinting,cutting,pivoting,jumping, and hopping.The movements should be performed with intensity and speed near maximum.cReturn to modi fied practice includes dynamic warm-up, sport-speci fic agility drills,and non-contact activities.
An athlete’s ability to return to sport may also be predicted by certain functional testing,such as the ability to perform a single leg hamstring bridge.Australian Rules football players demonstrating low hamstring strength,assessed via the single leg hamstring bridge test,were at increased risk for hamstring injury. A score of less than 20 repetitions is considered poor,25 repetitions is considered average,and greater than 30 repetitions is consideredgood.Theplayerswhosustainedahamstringinjuryin this study were close to or below the poor level.32Functional testing should also incorporate sport-related movements speci fic to the athlete with intensity and speed near maximum.2,6,97All tasks should be completed without pain,limitation,or hesitation in order for the athlete to return to sport.
There is currently no strong evidence for MRI findings to serve as criteria for time to return to sport after an acute hamstring strain.61,66,98Reurink and colleagues99showed that fibrosis on MRI at return to sport after acute hamstring injury is not associated with re-injury risk.More speci fically,16 of 67(24%) subjects without fibrosis on MRI and 10 of 41(24%)subjects with fibrosis on MRI sustained a re-injury.These results emphasize that clinical and functional tests seem to be better associated with determining return to sport and risk of re-injury than findings on MRI.The authors of this review article have devised an algorithm to assist clinicians in the decision-making process when returning an athlete to sport(Fig.1).
9.Summary
Hamstringstraininjuriesareoneofthemostcommonreasons for loss of playing time in athletes at all levels of competition.A comprehensive evaluation assists in coming to an accurate diagnosis and determining the type of rehabilitation program that mosteffectivelypromotesmuscletissueandfunctionalrecovery, which is essential to minimize the risk of re-injury and to optimize athlete performance.Without adequate rehabilitation, athletes may experience persistent weakness in the injured muscle and adaptive changes in the biomechanics and motor patternsofsportingmovements.Thereismountingevidencethat rehabilitation strategies incorporating neuromuscular control; progressiveagilityandtrunkstabilization;andeccentricstrength training are more effective at promoting return to sport and minimize the risk of re-injury.Dynamic clinical and functional testscanbeusedtoassessreadinessforreturntosport;however, an athlete should continue independent rehabilitation after return to sport to aid in minimizing re-injury risk.
Authors’contributions
LNE and MAS conceived of the article ideas and design; LNE drafted,revised,and edited the manuscript;MAS assisted in revising and editing the manuscript.Both authors have read and approved the final version of the manuscript,and agree with the order of the presentation of the authors.
Competing interests
The authors declare that they have no competing interests.
Appendix:Supplementary material
Supplementary data to this article can be found online at doi:10.1016/j.jshs.2017.04.001
1.Sherry M.Examination and treatment of hamstring related injuries.Sports Health 2012;4:107–14.
2.Sherry MA,Johnston TS,Heiderscheit BC.Rehabilitation of acute hamstring strain injuries.Clin Sports Med 2015;34:263–84.
3.San filippo JL,Silder A,Sherry MA,Tuite MJ,Heiderscheit BC.Hamstring strength and morphology progression after return to sport from injury.Med Sci Sports Exerc 2013;45:448–54.
4.Sherry MA,Best TM.A comparison of 2 rehabilitation programs in the treatment of acute hamstring strains.J Orthop Sports Phys Ther 2004;34:116–25.
5.Orchard J,Best TM.The management of muscle strain injuries:an early return versus the risk of recurrence.Clin J Sport Med 2002;12:3–5.
6.Heiderscheit BC,Sherry MA,Silder A,Chumanov ES,Thelen DG. Hamstring strain injuries:recommendations for diagnosis,rehabilitation, and injury prevention.J Orthop Sports Phys Ther 2010;40:67–81.
7.Dalton SL,Kerr ZY,Dompier TP.Epidemiology of hamstring strains in 25 NCAA sports in the 2009–2010 to 2013–2014 academic years.Am J Sports Med 2015;43:2671–9.
8.Sherry MA,Best TM,Silder A,Thelen DG,Heiderscheit BC.Hamstring strains:basic science and clinical research applications for preventing the recurrent injury.Strength Cond J 2011;33:56–71.
9.Cross KM,Gurka KK,Conaway M,Ingersoll CD.Hamstring strain incidence between genders and sports in NCAA athletics.Athl Ther Today 2010;2:124–30.
10.Brooks JH,Fuller CW,Kemp SP,Reddin DB.Incidence,risk,and prevention of hamstring muscle injuries in professional rugby union.Am J Sports Med 2006;34:1297–306.
11.Silder A,Sherry MA,San filippo J,Tuite MJ,Hetzel SJ,Heiderscheit BC. Clinical and morphological changes following 2 rehabilitation programs for acute hamstring strain injuries:a randomized clinical trial.J Orthop Sports Phys Ther 2013;43:284–99.
12.Cross KM,Gurka KK,Saliba S,Conaway M,Hertel J.Comparison of hamstring strain injury rates between male and female intercollegiate soccer athletes.Am J Sports Med 2013;41:742–8.
13.Feeley BT,Kennelly S,Barnes RP,Muller MS,Kelly BT,Rodeo SA,et al. Epidemiology of national football league training camp injuries from 1998 to 2007.Am J Sports Med 2008;36:1597–603.
14.Ekstrand J,Hägglund M,Waldén M.Epidemiology of muscle injuries in professional football(soccer).Am J Sports Med 2011;39:1226–32.
15.Opar DA,Drezner J,Shield A,Williams M,Webner D,Sennett B,et al. Acute hamstring strain injury in track-and- field athletes:a 3-year observational study at the Penn Relay Carnival.Scand J Med Sci Sports 2014;24:e254–9.
16.Chumanov ES,Heiderscheit BC,Thelen DG.The effect of speed and in fluence of individual muscles on hamstring mechanics during the swing phase of sprinting.J Biomech 2007;40:3555–62.
17.Chumanov ES,Heiderscheit BC,Thelen DG.Hamstring musculotendon dynamics during stance and swing phases of high-speed running.Med Sci Sports Exerc 2011;43:525–32.
18.Thelen DG,Chumanov ES,Best TM,Swanson SC,Heiderscheit BC. Simulation of biceps femoris musculotendon mechanics during the swing phase of sprinting.Med Sci Sports Exerc 2005;37:1931–8.
19.Fiorentino NM,Rehorn MR,Chumanov ES,Thelen DG,Blemker SS. Computational models predict larger muscle tissue strains at faster sprinting speeds.Med Sci Sports Exerc 2014;46:776–86.
20.Schache AG,Dorn TW,Blanch PD,Brown NA,Pandy MG.Mechanics of the human hamstring muscles during sprinting.Med Sci Sports Exerc 2012;44:647–58.
21.Higashihara A,Ono T,Kubota J,Okuwaki T,Fukubayashi T.Functional differences in the activity of the hamstring muscles with increasing running speed.J Sports Sci 2010;28:1085–92.
22.Silder A,Thelen DG,Heiderscheit BC.Effects of prior hamstring strain injury on strength, flexibility,and running mechanics.Clin Biomech (Bristol,Avon)2010;25:681–6.
23.Askling CM,Tengvar M,Saartok T,Thorstensson A.Acute first-time hamstring strains during high-speed running:a longitudinal study including clinical and magnetic resonance imaging findings.Am J Sports Med 2007;35:197–206.
24.Askling CM,Tengvar M,Saartok T,Thorstensson A.Acute first-time hamstringstrainsduringslow-speedstretching:clinical,magnetic resonance imaging,and recovery characteristics.Am J Sports Med 2007;35:1716–24.
25.Askling C,Saartok T,Thorstensson A.Type of acute hamstring strain affects flexibility,strength,and time to return to pre-injury level.Br J Sports Med 2006;40:40–4.
26.Gabbe BJ,Bennell KL,Finch CF,Wajswelner H,Orchard JW.Predictors of hamstring injury at the elite level ofAustralian football.Scand J Med Sci Sports 2006;16:7–13.
27.Verrall GM,Slavotinek JP,Barnes PG,Fon GT,Spriggins AJ.Clinical risk factors for hamstring muscle strain injury:a prospective study with correlation of injury by magnetic resonance imaging.Br J Sports Med 2001;35:435–40.
28.Engebretsen AH,Myklebust G,Holme I,Engebretsen L,Bahr R.Intrinsic risk factors for hamstring injuries among male soccer players:a prospective cohort study.Am J Sports Med 2010;38:1147–53.
29.Foreman TK,Addy T,Baker S,Burns J,Hill N,Madden T.Prospective studies into the causation of hamstring injuries in sport:a systematic review.Phys Ther Sport 2006;7:101–9.
30.Orchard JW.Intrinsic and extrinsic risk factors for muscle strains in Australian football.Am J Sports Med 2001;29:300–3.
31.Worrell TW.Factors associated with hamstring injuries:an approach to treatment and preventative measures.Sports Med 1994;17:338–45.
32.Freckleton G,Cook J,Pizzari T.The predictive validity of a single leg bridge test for hamstring injuries in Australian Rules football players.Br J Sports Med 2014;48:1–5.
33.Agre JC.Hamstring injuries.Proposed aetiological factors,prevention,and treatment.Sports Med 1985;2:21–33.
34.Croisier J,Ganteaume S,Binet J,Genty M,Ferret J.Strength imbalances and prevention of hamstring injury in professional soccer players:a prospective study.Am J Sports Med 2008;36:1469–75.
35.Schache AG,Crossley KM,Macindoe IG,Fahmer BB,Pandy MG.Can a clinical test of hamstring strength identify football players at risk of hamstring strain?Knee Surg Sports Traumatol Arthrosc 2011;19:38–41.
36.Arnason A,Andersen TE,Holme I,Engebretsen L,Bahr R.Prevention of hamstring strains in elite soccer:an intervention study.Scand J Med Sci Sports 2008;18:40–8.
37.Yeung SS,Suen AM,Yeung EW.A prospective cohort study of hamstring injuries in competitive sprinters:preseason muscle imbalance as a possible risk factor.Br J Sports Med 2009;43:589–94.
38.Cameron ML,Adams RD,Maher CG,Misson D.Effect of the HamSprint Drills training programme on lower limb neuromuscular control in Australian football players.J Sci Med Sport 2009;12:24–30.
39.Kuszewski M,Gnat R,Saulicz E.Stability training of the lumbo-pelvo-hip complex in fluence stiffness of the hamstrings:a preliminary study.Scand J Med Sci Sports 2009;19:260–6.
40.Panayi S.The need for lumbar–pelvic assessment in the resolution of chronic hamstring strain.J Bodyw Mov Ther 2010;14:294–8.
41.deVisser HM,Reijman M,Heijboer MP,Bos PK.Risk factors of recurrent hamstring injuries:a systematic review.Br J Sports Med 2012;46:124–30.
42.van Beijsterveldt AM,van de Port IG,Vereijken AJ,Backx FJ.Risk factors for hamstring injuries in male soccer players:a systematic review of prospective studies.Scand J Med Sci Sports 2013;23:253–62.
43.Birmingham P,Muller M,Wickiewicz T,Cavanaugh J,Rodeo S,Warren R.Functional outcome after repair of proximal hamstring avulsions.J Bone Joint Surg Am 2011;93:1819–26.
44.Chakravarthy J,Ramisetty N,Pimpalnerkar A,Mohtadi N.Surgical repair of complete proximal hamstring tendon ruptures in water skiers and bull riders:a report of four cases and review of the literature.Br J Sports Med 2005;39:569–72.
45.Sallay PI,Fiedman RL,Coogan PG,Garrett WE.Hamstring muscle injuries among water skiers:functional outcome and prevention.Am J Sports Med 1996;24:130–6.
46.Sarimo J,Lempainen L,Mattila K,Orava S.Complete proximal hamstring avulsions:a series of 41 patients with operative treatment.Am J Sports Med 2008;36:1110–5.
47.Konan S,Haddad F.Successful return to high level sports following early surgical repair of complete tears of the proximal hamstring tendons.Int Orthop 2010;34:119–23.
48.Wood DG,Packham I,Trikha SP,Linklater J.Avulsion of the proximal hamstring origin.J Bone Joint Surg Am 2008;90:2365–74.
49.Gidwani S,Bircher MD.Avulsion injuries of the hamstring origin:a series of 12 patients and management algorithm.Ann R Coll Surg Engl 2007;89:394–9.
50.Wootton JR,Cross MJ,Holt KW.Avulsion of the ischial apophysis:the case for open reduction and internal fixation.J Bone Joint Surg Br 1990;72:625–7.
51.Cacchio A,Rompe JD,Furia JP,Susi P,Santilli V,De Paulis F.Shockwave therapy for the treatment of chronic proximal hamstring tendinopathy in professional athletes.Am J Sports Med 2011;39:146–53.
52.Lempainen L,Sarimo J,Mattila K,Vaittinen S,Orava S.Proximal hamstringtendinopathy:resultsofsurgicalmanagementand histopathologic findings.Am J Sports Med 2009;37:727–34.
53.Fredericson M,Moore W,Guillet M,Beaulieu C.High hamstring tendinopathy in runners:meeting the challenges of diagnosis,treatment, and rehabilitation.Phys Sportsmed 2005;33:32–52.
54.Reiman MP,Loudon JK,Goode AP.Diagnostic accuracy of clinical tests for assessment of hamstring injury:a systematic review.J Orthop Sports Phys Ther 2013;43:222–31.
55.Cacchio A,Borra F,Severini G,Foglia A,Musarra F,Taddio N,et al. Reliability and validity of three pain provocation tests used for thediagnosis of chronic proximal hamstring tendinopathy.Br J Sports Med 2012;46:883–7.
56.Brunker P,Kahn K.Clinical sports medicine.2nd ed.Sydney,NSW: McGraw-Hill;2001.
57.Saikku K,Vasenius J,Saar P.Entrapment of the proximal sciatic nerve by the hamstring tendons.Acta Orthop Belg 2010;76:321–4.
58.Cohen SB,Towers JD,Zoga A,Irrgang JJ,Makda J,Deluca PF,et al. Hamstring injuries in professional football players:magnetic resonance imaging correlation with return to play.Sports Health 2011;3:423–30.
59.Connell DA,Schneider-Kolsky ME,Hoving JL,Malara F,Buchbinder R, Koulouris G,et al.Longitudinal study comparing sonographic and MRI assessments of acute and healing hamstring injuries.AJRAm J Roentgenol 2004;183:975–84.
60.Slavotinek JP,Verrall GM,Fon GT.Hamstring injury in athletes:using MR imaging measurements to compare extent of muscle injury with amount of time lost from competition.AJR Am J Roentgenol 2002;179: 1621–8.
61.De Vos RJ,Reurink G,Goudswaard GJ,Moen MH,Weir A,Tol JL. Clinical findings just after return to play predict hamstring re-injury,but baseline MRI findings do not.Br J Sports Med 2014;48:1377–84.
62.Koulouris G,Connell DA,Brukner P,Schneider-Kolsky M.Magnetic resonance imaging parameters for assessing risk of recurrent hamstring injuries in elite athletes.Am J Sports Med 2007;35:1500–6.
63.Petersen J,Thorborg K,Nielsen MB,Skjødt T,Bolvig L,Bang N,et al. The diagnostic and prognostic value of ultrasonography in soccer players with acute hamstring injuries.Am J Sports Med 2014;42:399–404.
64.Guillodo Y,Here-Dorignac C,Thoribe B,Madouas G,Dauty M,Tassery F,et al.Clinical predictors of time to return to competition following hamstring injuries.Muscles Ligaments Tendons J 2014;4:386–90.
65.Warren P,Gabbe BJ,Schneider-Kolsky M,Bennell KL.Clinical predictors of time to return to competition and of recurrence following hamstring strain in elite Australian footballers.Br J Sports Med 2010;44:415–9.
66.Jacobsen P,Witvrouw E,Muxart P,Tol JL,Whiteley R.A combination of initial and follow-up physiotherapist examination predicts physiciandeterminedtimetoreturntoplayafterhamstringinjury,withnoaddedvalue of MRI.Br J Sports Med 2016;50:431–9.
67.Malliaropoulos N,Papacostas E,Kiritsi O,Papalada A,Gougoulias N, Maffulli N.Posterior thigh muscle injuries in elite track and field athletes. Am J Sports Med 2010;38:1813–9.
68.Malliaropoulos N,Isinkaye T,Tsitas K,Maffulli N.Reinjury after acute posterior thigh muscle injuries in elite track and field athletes.Am J Sports Med 2011;39:304–10.
69.Jarvinen TA,Jarvinen TL,Kaariainen M,Kalimo H,Jarvinen M.Muscle injuries:biology and treatment.Am J Sports Med 2005;33:745–64.
70.Starkey C,Ryan L.Evaluation of orthopedic and athletic injuries.2nd ed. Philadelphia,PA:F.A.Davis Company;2002.
71.Neumann DA.Kinesiology of the musculoskeletal system:foundations for rehabilitation.2nd ed.St.Louis,MD:Mosby/Elsevier;2010.
72.Sole G,Milosavljevic S,Nicholson HD,Sullivan SJ.Selective strength loss and decreased muscle activity in hamstring injury.J Orthop Sports Phys Ther 2011;41:354–63.
73.Askling CM,Malliaropoulos N,Karlsson J.High-speed running type or stretching-type of hamstring injuries makes a difference to treatment and prognosis.Br J Sports Med 2012;46:86–7.
74.Askling CM,Tengvar M,Saartok T,Thorstensson A.Proximal hamstring strains of stretching type in different sports:injury situations,clinical and magnetic resonance imaging characteristics,and return to sport.Am J Sports Med 2008;36:1799–804.
75.Askling CM,Tengvar M,Thorstensson A.Acute hamstring injuries in Swedish elite football:a prospective randomised controlled clinical trial comparing two rehabilitation protocols.Br J Sports Med 2013;47:953–9.
76.Askling CM,Tengvar M,Tarassova O,Thorstensson A.Acute hamstring injuries in Swedish elite sprinters and jumpers:a prospective randomised controlled clinical trial comparing two rehabilitation protocols.Br J Sports Med 2014;48:532–9.
77.DeWitt J,Vidale T.Recurrent hamstring injury:consideration following operative and non-operative management.Int J Sports Phys Ther 2014; 9:798–812.
78.Mendiguchia J,Alentorn-Geli E,Brughelli M.Hamstring strain injuries: are we heading in the right direction?Br J Sports Med 2012;46:81–5.
79.Fousekis K,Tsepis E,Poulmedis P,Athanasopoulos S,Vagenas G. Intrinsic risk factors of non-contact quadriceps and hamstring strains in soccer:a prospective study of 100 professional players.Br J Sports Med 2011;45:709–14.
80.Askling CM,Nilsson J,Thorstensson A.A new hamstring test to complement the common clinical examination before return to sport after injury.Knee Surg Sports Traumatol Arthrosc 2010;18:1798–803.
81.Opar DA,Williams MD,Timmins RG,Hickey J,Duhig SJ,Shield AJ.The effect of previous hamstring strain injuries on the change in eccentric hamstring strength during preseason training in eliteAustralian footballers. Am J Sports Med 2015;43:377–84.
82.Maniar N,Shield AJ,Williams MD,Timmins RG,Opar DA.Hamstring strength and flexibility after hamstring strain injury:a systematic review and meta-analysis.Br J Sports Med 2016;50:909–20.
83.Fyfe JJ,Opar DA,Williams MD,Shield AJ.The role of neuromuscular inhibition in hamstring strain injury recurrence.J Electromyogr Kinesiol 2013;23:523–30.
84.Silder A,Heiderscheit BC,Thelen DG,Enright T,Tuite MJ.MR observationsoflong-termmusculotendonremodelingfollowinga hamstring strain injury.Skeletal Radiol 2008;37:1101–9.
85.Silder A,Reeder SB,Thelen DG.The in fluence of prior hamstring injury on lengthening muscle tissue mechanics.J Biomech 2010;43:2254–60.
86.Sole G,Milosavljevic S,Nicholson H,Sullivan SJ.Altered muscle activation following hamstring injuries.Br J Sports Med 2012;46:118–23.
87.ThelenDG,ChumanovES,SherryMA,HeiderscheitBC. Neuromusculoskeletal models provide insights into the mechanisms and rehabilitation of hamstring strains.Exerc Sport Sci Rev 2006;34:135–41.
88.Proske U,Morgan DL,Brockett CL,Percival P.Identifying athletes at risk of hamstring strains and how to protect them.Clin Exp Pharmacol Physiol 2004;31:546–50.
89.Brockett CL,Morgan DL,Proske U.Predicting hamstring strain injury in elite athletes.Med Sci Sports Exerc 2004;36:379–87.
90.Schache A.Eccentric hamstring muscle training can prevent hamstring injuries in soccer players.J Physiother 2012;58:58.doi:10.1016/S1836-9553(12)70074-7
91.Schmitt B,Tim T,McHugh M.Hamstring injury rehabilitation and prevention of reinjury using lengthened state eccentric training:a new concept.Int J Sports Phys Ther 2012;7:333–41.
92.Askling C,Karlsson J,Thorstensson A.Hamstring injury occurrence in elite soccer players after preseason strength training with eccentric overload.Scand J Med Sci Sports 2003;13:244–50.
93.Turl SE,George KP.Adverse neural tension:a factor in repetitive hamstring strain?J Orthop Sports Phys Ther 1998;27:16–21.
94.Kornberg C,Lew P.The effect of stretching neural structures on grade one hamstring injuries.J Orthop Sports Phys Ther 1989;10:481–7.
95.van der Horst N,van de Hoef S,Reurink G,Huisstede B,Backx F.Return to play after hamstring injuries:a qualitative systematic review of de finitions and criteria.Sports Med 2016;46:899–912.
96.Croisier JL,Forthomme B,Namurois MH,Vanderthommen M,Crielaard JM.Hamstring muscle strain recurrence and strength performance disorders.Am J Sports Med 2002;30:199–203.
97.Delvaux F,Rochcongar P,Bruyere O,Bourlet G,Daniel C,Diverse P, et al.Return-to-play criteria after hamstring injury:actual medicine practice in professional soccer teams.J Sports Sci Med 2014;13:721–3.
98.Reurink G,Brilman EG,de Vos RJ,Maas M,Moen MH,Weir A,et al. Magnetic resonance imaging in acute hamstring injury:can we provide a return to play prognosis?Sports Med 2015;45:133–46.
99.Reurink G,Almusa E,Goudswaard GJ,Tol JL,Hamilton B,Moen MH, et al.No association between fibrosis on magnetic resonance imaging at return to play and hamstring reinjury risk.Am J Sports Med 2015; 43:1228–34.
16 November 2016;revised 25 January 2017;accepted 24 February 2017
Available online 10 April 2017
Peer review under responsibility of Shanghai University of Sport.
*Corresponding author.
E-mail address:MSherry@uwhealth.org(M.A.Sherry)
http://dx.doi.org/10.1016/j.jshs.2017.04.001
2095-2546/©2017 Production and hosting by Elsevier B.V.on behalf of Shanghai University of Sport.This is an open access article under the CC BY-NC-ND license(http://creativecommons.org/licenses/by-nc-nd/4.0/).
 Journal of Sport and Health Science2017年3期
Journal of Sport and Health Science2017年3期
- Journal of Sport and Health Science的其它文章
- Time for a paradigm shift in the classi fication of muscle injuries
- Risk factors for hamstring injuries in Australian male professional cricket players
- Relationships among hamstring muscle optimal length and hamstring flexibility and strength
- The effect of hamstring flexibility on peak hamstring muscle strain in sprinting
- Motivation dimensions for running a marathon:A new model emerging from the Motivation of Marathon Scale(MOMS)
- The ethics of exercise in eating disorders:Can an ethical principles approach guide the next generation of research and clinical practice?
