垂体转移性肺非典型类癌
阎晓玲 唐帆 韩竹语 张学斌 金树梅
·临床病理报告·
垂体转移性肺非典型类癌
阎晓玲 唐帆 韩竹语 张学斌 金树梅
目的报道1例垂体转移性肺非典型类癌患者的临床资料,总结此类肿瘤的临床病理学特征及诊断与鉴别诊断要点。方法与结果女性患者,81岁,临床表现为头痛,突然失明;头部MRI提示鞍区占位性病变。遂行经鼻蝶入路鞍区占位性病变切除术,术中可见肿瘤位于鞍内,呈灰红色,直径约2 cm,质地柔软,血运不丰富,无包膜,边界欠清晰,沿边缘手术全切除肿瘤。组织学形态观察,肿瘤组织由形态较单一、大小较一致的小圆形细胞构成,呈巢片状弥漫性分布,可见核分裂象和灶性坏死。免疫组织化学染色,肿瘤细胞弥漫性表达突触素、CD56,部分表达甲状腺转录因子⁃1、广谱细胞角蛋白、P53,不表达生长激素、泌乳素、促肾上腺皮质激素、卵泡刺激素、促甲状腺激素、黄体生成素、S⁃100蛋白、甲状腺球蛋白、降钙素,Ki⁃67抗原标记指数约为33%。结论垂体转移瘤临床少见,垂体转移性肺非典型类癌更为罕见,明确诊断依靠临床病史、组织学形态和免疫表型。
肺肿瘤; 类癌瘤; 肿瘤转移; 垂体; 免疫组织化学; 病理学
垂体转移瘤临床罕见[1⁃3],近年随着肿瘤患者生存期的延长和神经影像学的发展,病例数有所增加,发生率约占全部垂体肿瘤的 1%[2,4⁃5],女性乳腺和男性肺部为最常见的肿瘤原发灶[1⁃2,6]。本文报告1例垂体转移性肺非典型类癌患者,通过复习相关文献,对其组织形态学特点、免疫组织化学表型、诊断与鉴别诊断、治疗及预后等临床病理学特征进行总结。
病历摘要
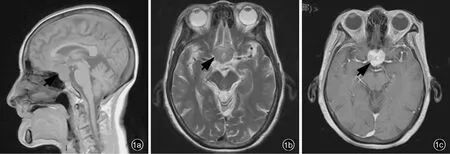
图1 头部MRI检查所见 1a 矢状位T1WI显示,鞍内和鞍上占位性病变,信号强度不均匀,其内可见小片状低信号影(箭头所示) 1b 横断面T2WI显示,鞍上病变呈等信号,其内可见小片状高信号影(箭头所示) 1c 横断面增强T1WI显示,病灶呈明显不均匀强化(箭头所示)Figure 1 Head MRI imaging findings Sagittal T1WI showed intrasellar and suprasellar space occupying lesion uneven signal strength.Intralesional findings strip hypointense signal area(arrow indicates,Panel 1a).Axial T2WI showed suprasellar lesion equisignal.There were strip hyperintense signal shadow(arrow indicates,Panel 1b).Axial T1WI enhanced demonstrated a significant enhancement(arrow indicates,Panel 1c).
患者 女性,81岁,主因间断性头痛10余年、视力下降1个月、失明1周,于2015年5月21日入院。患者10余年前无明显诱因出现间断性头痛,可自行缓解,未予处理;1个月前因结肠炎行结肠镜检查后3 d出现双眼视物模糊,视物成双,视力进行性下降,左眼症状较重,无意识障碍、头晕、呕吐,外院诊断与治疗(具体不详)后视力无明显改善;1周前突然失明,甚至无光感,无意识障碍、肢体活动障碍,外院头部MRI显示鞍区占位性病变。为求进一步诊断与治疗,至我院就诊。患者自发病以来,精神、饮食尚可,睡眠较差,大小便正常,体重无明显减轻。
既往史、个人史及家族史 患者既往有冠心病病史20余年,药物控制较佳(具体方案不详);高血压病史3余年,经药物控制(具体方案不详)为120/70 mm Hg(1 mm Hg=0.133 kPa)左右,已停药1年;余无特殊。个人史及家族史均无特殊。
体格检查 患者体温36.5℃,脉搏75次/min,呼吸15次/min,血压 135/86 mm Hg;神志清楚,对答切题,高级神经功能正常;头部无畸形;双侧瞳孔等大、等圆,直径约3 mm;伸舌居中,无口角歪斜;无颈项强直;余脑神经检查未见异常。四肢肌力5级、肌张力正常,感觉和共济运动未见明显异常,腱反射强阳性,病理反射未引出。
辅助检查 实验室检查血常规和凝血功能试验均于正常值范围;血清脂质:总胆固醇(TC)为5.90 mmol/L(0~5.70 mmol/L),白蛋白为37.60 g/L(40~55 g/L),低密度脂蛋白胆固醇(LDL⁃C)水平3.48 mmol/L(0~3.12 mmol/L);垂体激素:泌乳素(PRL)45.97 ng/ml(4.79~23.30 ng/ml),余均于正常值范围。头部MRI显示,鞍内和鞍上占位性病变,呈T1WI等或稍低信号,T2WI等或高信号,累及左侧海绵窦;增强扫描病灶呈明显强化,约为2.80 cm×2.40 cm×2.20 cm(图1)。
诊断与治疗经过 临床诊断为垂体占位性病变,考虑垂体瘤可能性大。于2015年5月25日在全身麻醉下行经鼻蝶入路鞍区占位性病变切除术。术中可见肿瘤位于鞍内,呈灰红色,直径约为2 cm,质地柔软,血运不丰富,无包膜,边界欠清晰,沿边缘手术全切除肿瘤,行组织病理学检查。(1)大体标本观察:手术切除标本呈灰红色破碎组织一堆,约2.00 cm×1.00 cm×0.50 cm。经体积分数为3.70%中性甲醛溶液固定,常规脱水、石蜡包埋,4μm连续切片,分别行HE染色和免疫组织化学染色。(2)HE染色:光学显微镜观察显示,垂体正常结构破坏,肿瘤组织由巢片状分布的小至中等大小细胞构成,形态较单一、大小较一致,胞核呈圆形或卵圆形,染色质呈细颗粒状,核仁不明显,胞质较少,核分裂象为5~7个/10高倍视野(HPF),可见局部小灶性坏死;无包膜,与周围正常垂体组织界限欠清晰(图2)。(3)免疫组织化学染色:采用EnVision二步法进行检测,检测用Ⅰ抗、Ⅱ抗、显色剂和染色系统参见表1。结果显示,肿瘤细胞胞质弥漫性表达突触素(Syn,图3a)、CD56,部分表达甲状腺转录因子⁃1(TTF⁃1,图3b)、广谱细胞角蛋白(PCK)、P53,不表达生长激素(GH)、PRL、促肾上腺皮质激素(ACTH)、卵泡刺激素(FSH)、促甲状腺激素(TSH)、黄体生成素(LH)、S⁃100蛋白(S⁃100)、甲状腺球蛋白(TG)、降钙素,Ki⁃67抗原标记指数约33%(图3c)。初步病理诊断为:(鞍区)小蓝圆细胞恶性肿瘤,考虑转移性神经内分泌肿瘤。术后为明确病因建议进一步行胸部CT检查,显示左肺下叶心缘旁团状软组织密度影(图4)。最终病理诊断为(鞍区)转移性肺非典型类癌。患者自动出院后经多所医院会诊,未再进一步治疗,3个月后去世。
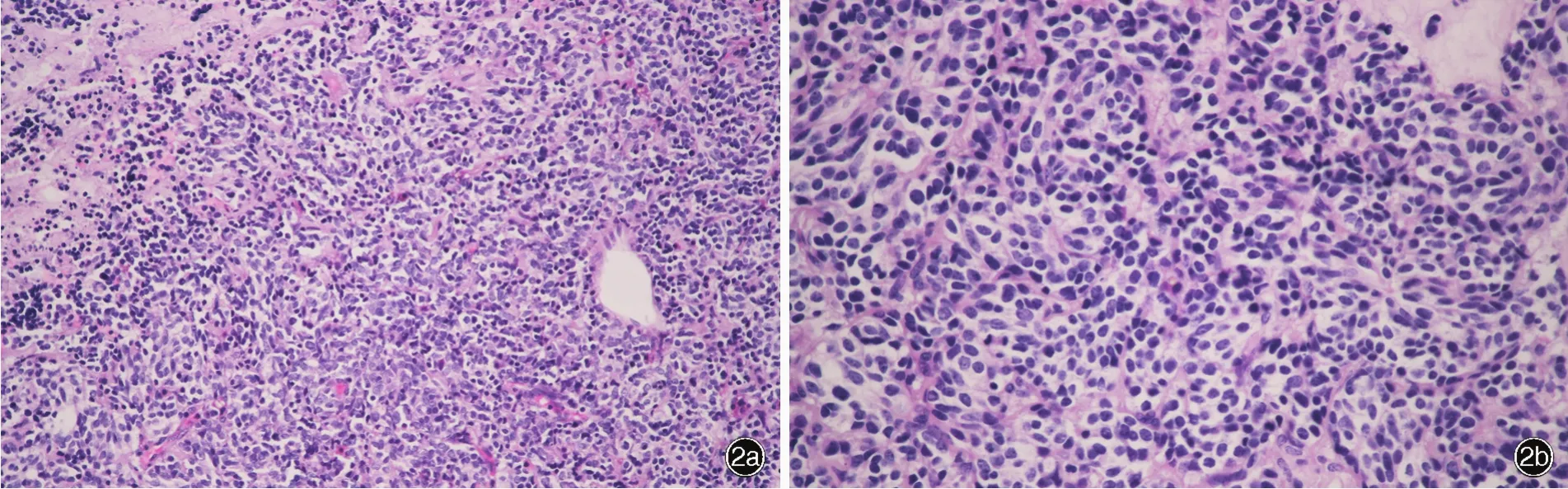
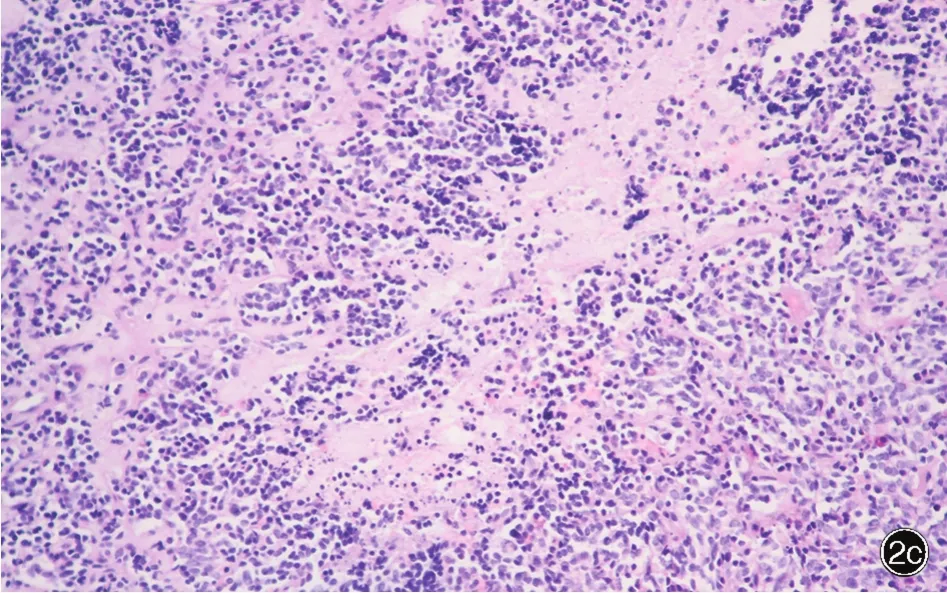
图2 光学显微镜观察所见 HE染色 2a 肿瘤细胞呈巢片状弥漫性分布,大小较一致,胞质呈嗜酸性 ×200 2b肿瘤细胞胞核呈圆形,染色质细颗粒状,核仁不明显,核分裂象可见 ×400 2c 部分区域可见坏死 ×200Figure 2 Optical microscopy findings HE staining The tumor was composed of small cells densely growing in sheet⁃like or nesting growth pattern with eosinophilic cytoplasm(Panel 2a). ×200 Small to intermediate sized round cells nesting arranged,with fine granular chromatin and mitotic figures,nucleolus were not obvious(Panel 2b). ×400 Focal necrosis was seen(Panel 2c).×200
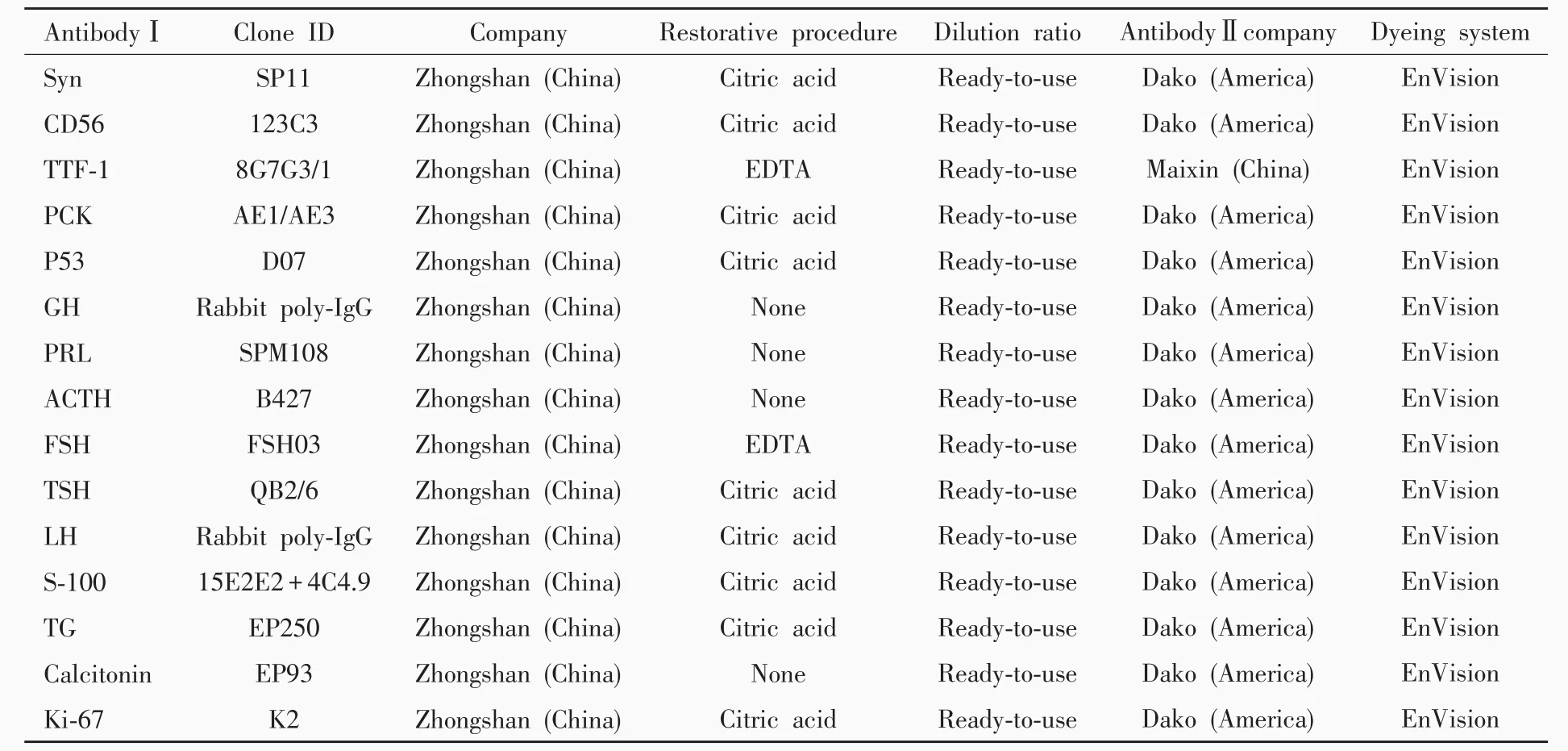
表1 肿瘤免疫组织化学检测各项抗体列表Table 1.Antibodies used for immunohistochemical examination


图3 光学显微镜观察所见 免疫组织化学染色(EnVision二步法) ×200 3a 肿瘤细胞弥漫性表达Syn 3b 肿瘤细胞部分表达TTF⁃1 3c Ki⁃67抗原标记指数约为33%Figure 3 Optical microscopy findings Immunohistochemical staining(EnVision) ×200 The tumor cells were diffusely immunopositive for Syn(Panel 3a)and TTF⁃1(Panel 3b).Ki⁃67 labeling index was about 33%(Panel 3c).
讨 论
垂体转移瘤临床罕见[1⁃3],近年来随着肿瘤患者生存期的延长和影像学技术的发展,病例数有所增加,其发生率约占全部垂体肿瘤的 1%[2,4⁃5],女性乳腺和男性肺部为最常见的肿瘤原发灶[1⁃2,6],亦可见腮腺腺样囊性癌[7]、甲状腺癌[8⁃9]、肝癌[1,10]、胃肠道肿瘤[1,11]、肾细胞癌[12]、绒癌[13]、前列腺癌[14]、淋巴瘤[15]、横纹肌肉瘤[16]和皮肤 Merkel细胞癌[17]垂体转移的病例。肺非典型类癌属于神经内分泌肿瘤,在2015年的世界卫生组织(WHO)肺和胸膜肿瘤分类[18⁃19]中,肺神经内分泌肿瘤作为上皮组织肿瘤,与鳞状细胞癌和腺癌并列,再一次明确非典型类癌的诊断标准:具有类癌组织学形态特征,核分裂象2~10个/2 mm2或坏死(通常为点状或斑点状),其生物学行为和预后为中级别。
肺类癌占所有原发性肺肿瘤的2%,典型类癌与非典型类癌的发病比例约为9∶1,平均发病年龄50~60岁,尽管有文献报道非典型类癌以男性为主,但大多数学者认为女性常见[19]。非典型类癌主要表现为周围型,更具侵袭性,有40%~50%患者存在淋巴结转移,约20%出现远处转移,5和10年生存率分别为60%和35%[19],而发生垂体转移的病例仅为个案报道[20⁃23]。近50%的支气管肺类癌为体格检查时偶然发现,最常见症状是咳嗽和咯血,是与支气管堵塞有关的典型症状。类癌综合征少见,仅见发生广泛转移时。如果不考虑原发肿瘤,发生垂体转移的患者通常为无症状,偶尔因垂体受累引起的症状与体征考虑垂体疾病而就诊,而70%的症状性患者可出现尿崩症[24],23%出现垂体激素降低[22],6.30%出现高泌乳素血症,其他表现还包括视野缺损[21]、脑神经麻痹和头痛,偶可见原发性神经内分泌肿瘤(肺和胰腺)垂体转移后分泌ACTH和生长激素释放激素(GHRH)致Cushing综合征和肢端肥大症[25⁃26]。本文患者为老年女性,以视力下降、突然失明的垂体占位征象入院,血清泌乳素水平升高,可能是垂体柄受压所致。也有个案报道,泌乳素>250 ng/ml影响临床诊断与治疗[26],临床应予以注意。术后为进一步明确诊断,胸部CT显示呈周围型肺非典型类癌。

图4 胸部CT显示,左肺下叶心缘旁团块状软组织密度影,边缘毛糙(箭头所示)Figure 4 Axial chest CT scan suggested a soft tissue density masses on the left lower lobe beside the heart,with roughen edges(arrow indicates).
典型神经内分泌肿瘤(类癌和小细胞癌)具有独特的组织学形态特点,但垂体转移性肺非典型类癌目前仅见个案报道。免疫组织化学染色,胞核部分表达TTF⁃1。研究显示,TTF⁃1常表达于肺典型和非典型类癌,而不表达于其他器官类癌[23],Penman等[27]认为,表达于结肠癌和直肠癌肿瘤细胞胞核的TTF⁃1克隆号为SPT24,而克隆号为8G7G1的TTF⁃1呈阴性,这也是采用TTF⁃1这一生物学标志物进行鉴别诊断时应注意的。
当肿瘤细胞数目较少、分化较差、病史不典型时,易出现诊断困难或误诊,应注意与以下疾病相鉴别:(1)垂体腺瘤。最常发生于蝶鞍的肿瘤,发病年龄随腺瘤类型的不同而各异。MRI表现为均质性,T1WI呈低信号。肿瘤细胞丰富,呈弥漫性生长,胞核呈圆形、染色质纤细,胞质中等,核分裂象不常见;肿瘤细胞胞质表达Syn、嗜铬素A(CgA)和相应垂体激素,Ki⁃67抗原标记指数通常<3%。(2)垂体增生。可由多种生理性或病理性原因导致,影像学表现为鞍区球形占位效应,一般以中线为主,界限清晰,垂体上缘膨隆,高度增加。传统认为,CT所示垂体增高>10 mm伴或不伴鞍底侵犯和垂体柄偏移是诊断垂体腺瘤的标准,故弥漫性垂体增生与垂体腺瘤难以鉴别;MRI显示垂体信号不均匀,垂体柄偏斜。增生细胞因类型不同而形态各异,组织学形态可见结节性和弥漫性增生,结节性增生表现为腺泡扩张,而细胞相对单一,对周围组织无挤压,界限清晰;弥漫性增生表现为垂体细胞数目增加,但无腺泡结构改变,有时需行细胞计数以明确诊断。核分裂象罕见。Ki⁃67抗原标记指数均较低。网织纤维染色可见正常腺泡结构,有助于区分正常垂体组织、增生垂体组织与垂体腺瘤。(3)副节瘤。副节瘤常发生于特定解剖部位,易与类癌的器官样结构相混淆,但可见S⁃100阳性的包绕小叶的支柱细胞,主细胞细胞角蛋白(CK)呈阴性,而类癌细胞CK呈阳性。(4)其他转移性肿瘤。组织学形态、免疫组织化学染色和临床病史有助于鉴别诊断。
垂体转移瘤的诊断与治疗主要是原发灶的诊断与治疗以及对症治疗,虽然可以选择放射治疗或药物化疗,但对于症状性患者,如本文患者有头痛、失明表现,外科手术以缓解症状是必须的。研究显示,是否外科手术解除垂体占位效应无明显差异[1],生存期根据原发肿瘤的侵袭性和分期通常为6个月至 1 年[26,28⁃29]。
垂体转移瘤临床罕见,迄今文献报道的垂体转移性肺非典型类癌病例仅为个案报道,应注意诊断与鉴别诊断。由于组织学形态和生物学行为均存在异质性,对其治疗与预后尚待进一步研究。本文患者自动出院后经多所医院会诊,但未进一步治疗,3个月后死亡。
[1]He W,Chen F,Dalm B,Kirby PA,Greenlee JD.Metastatic involvement of the pituitary gland:a systematic review with pooled individual patient data analysis.Pituitary,2015,18:159⁃168.
[2]Rotondo F,Kovacs K,Macdonald RL,Prud'homme GJ,Latta E,Munoz D.Non⁃small cell bronchial carcinoma metastasizing into a prolactin⁃producing pituitary adenoma.Int J Surg Pathol,2013,21:68⁃71.
[3]Hsiao CH,Wang CY,Chung MT,Yang MS.Diabetes insipidus due to pituitary metastasis in a woman with lung adenocarcinoma:a case report.Central Eur J Med,2011,6:475⁃479.
[4]Musolino NR,Vilar L,Kodaira S,Bronstein MD.Diagnóstico diferencial das massas selares//Vilar L.Endocrinologia clínica.Rio de Janeiro:Guanabara Koogan,2013:3⁃23.
[5]Ozturk MA,Eren OO,Sarikaya B,Aslan E,Oyan B.Pituitary metastasis of colon adenocarcinoma:a rare occurrence.J Gastrointest Cancer,2014,45 Suppl 1:85⁃87.
[6]Case records of the Massachusetts General Hospital.Case 35⁃2001:an 81⁃year⁃old man with hypothermia,bradycardia,and confusion.N Engl JMed,2001,345:1483⁃1488.
[7]D Hughes J,Retzlaff A,Sims J,O'Brien E,Giannini C,Huston J 3rd,Van Gompel JJ.Adenoid cystic carcinoma metastatic to the pituitary:a case report and discussion of potential diagnostic value of magnetic resonance elastography in pituitary tumors.World Neurosurg,2016,91:669.
[8]Vianello F,Mazzarotto R,Taccaliti A,Lora O,Basso M,Servodio O,Mian C,Sotti G.Follicular thyroid carcinoma with metastases to the pituitary causing pituitary insufficiency.Thyroid,2011,21:921⁃925.
[9]Lim W,Lim DS,Chng CL,Lim AY.Thyroid carcinoma with pituitary metastases:2 case reports and literature review.Thyroid,2010,20:823⁃830.
[10]Tanaka T,Hiramatsu K,Nosaka T,Saito Y,Naito T,Takahashi K,Ofuji K,Matsuda H,Ohtani M,Nemoto T,Suto H,Yamamoto T,Kimura H,Nakamoto Y.Pituitary metastasis of hepatocellular carcinoma presenting with panhypopituitarism:a case report.BMCCancer,2015,15:863.
[11]Thewjitcharoen Y,Shuangshoti S,Lerdlum S,Siwanuwatn R,Sunthornyothin S.Colorectal cancer manifesting with metastasis to prolactinoma:report of a case involving symptoms mimicking pituitary apoplexy.Intern Med,2014,53:1965⁃1969.
[12]Magnoli F,Finzi G,Riva C,Capella C.Renal cell carcinoma metastatic to a pituitary FSH/LH adenoma:case report and review of the literature.Ultrastruct Pathol,2014,38:430⁃437.
[13]Liu H,Xiao YD,Peng SP,Zhou SK,Liu J.Pituitary metastasis of choriocarcinoma:a case report.Oncol Lett,2016,11:1517⁃1520.
[14]Riemenschneider MJ,Beseoglu K,Hänggi D,Reifenberger G.Prostate adenocarcinoma metastasis in the pituitary gland.Arch Neurol,2009,66:1036⁃1037.
[15]Yang J,Zhao N,Zhang G,Zheng W.Clinical features of patients with non⁃Hodgkin's lymphoma metastasizing to the pituitary glands.Oncol Lett,2013,5:1643⁃1648.
[16]Ismail E,Issam L,Hamid M.Pituitary metastasis of rhabdomyosarcoma:a case report and review of the literature.J Med Case Rep,2014,8:144.
[17]Feletti A,Marton E,Rossi S,Canal F,Longatti P,Billeci D.Pituitary metastasis of Merkel cell carcinoma.J Neurooncol,
[18]2010,97:295⁃299.Travis WD,Brambilla E,Nicholson AG,Yatabe Y,Austin JH,Beasley MB,Chirieac LR,Dacic S,Duhig E,Flieder DB,Geisinger K,Hirsch FR,Ishikawa Y,Kerr KM,Noguchi M,Pelosi G,Powell CA,Tsao MS,Wistuba I;WHO Panel.The 2015 World Health Organization classification of lung tumors:impact of genetic,clinical and radiologic advances since the 2004 classification.JThorac Oncol,2015,10:1243⁃1260.
[19]Travis WD,Brambilla E,Burke AP,Marx A,Nicholson AG.WHO classification of tumours of the lung,pleura,thymus and heart.4th ed.Lyon:International Agency for Research on Cancer,2015:63⁃85.
[20]Campbell D,Amponsah N,Mott R,Ellis T.Carcinoid tumor of the lung metastatic to a previously identified pituitary adenoma.JSurg Case Rep,2012,(10):12.
[21]Shimon I,Hadani M,Nass D,Zwas ST.Malignant bronchial carcinoid tumor metastatic to the pituitary in a thyroid carcinoma patient: successful treatment with surgery,radiotherapy and somatostatin analog.Pituitary,2004,7:51⁃57.
[22]Jonnakuty CG,Mezitis SG.Pulmonary atypical carcinoid tumor with metastatic involvement of the pituitary gland causing functional hypopituitarism.Endocr Pract,2007,13:291⁃295.
[23]Moshkin O,Rotondo F,Scheithauer BW,Soares M,Coire C,Smyth HS,Goth M,Horvath E,Kovacs K.Bronchial carcinoid tumors metastatic to the sella turcica and review of the literature.Pituitary,2012,15:160⁃165.
[24]Reddy P,Kalemkerian GP.Unusual presentations of lung cancer.Case 1:diabtes insipidus as the initial manifestation of non⁃small⁃cell lung cancer.JClin Oncol,2002,20:4597⁃4602.
[25]Nasr C,Mason A,Mayberg M,Staugaitis SM,Asa SL.Acromegaly and somatotroph hyperplasia with adenomatous transformation due to pituitary metastasis of a growth hormone⁃releasing hormone⁃secreting pulmonary endocrine carcinoma.J Clin Endocrinol Metab,2006,91:4776⁃4780.
[26]Sanno N,Teramoto A,Osamura RY,Genka S,Katakami H,Jin L,Lloyd RV,Kovacs K.A growth hormone⁃releasing hormone⁃producing pancreatic islet cell tumor metastasized to the pituitary is associated with pituitary somatotroph hyperplasia and acromegaly.JClin Endocrinol Metab,1997,82:2731⁃2737.
[27]Penman D,Downie I,Roberts F.Positive immunostaining for thyroid transcription factor⁃1 in primary and metastatic colonic adenocarcinoma:a note of caution.J Clin Pathol,2006,59:663⁃664.
[28]Siqueira PF,Mathez AL,Pedretti DB,Abucham J.Pituitary metastasis of lung neuroendocrine carcinoma:case report and literature review.Arch Endocrinol Metab,2015,59:548⁃553.
[29]Heshmati HM,Scheithauer BW,Young WF Jr.Metastases to the pituitary.Endocrinologist,2002,12:45⁃49.
Atypical lung carcinoid metastasis to the pituitary gland
YAN Xiao⁃ling,TANG Fan,HAN Zhu⁃yu,ZHANG Xue⁃bin,JIN Shu⁃mei
Department of Pathology,Tianjin Huanhu Hospital,Tianjin 300350,China
Corresponding author:YAN Xiao⁃ling(Email:ll934065@126.com)
ObjectiveTo study clinicopathological features,diagnosis and differential diagnosis of atypical lung carcinoid metastasis to the pituitary gland based on clinical data of one patient.Methods and ResultsA 81⁃year⁃old female presented headache and sudden blindness,and head MRI showed that there was a lesion at the saddle area.The tumor was detected at intrasellar and in grayish red during surgery.The diameter of tumor was 2 cm.The tumor was soft with no envelop at and well⁃defined margins,and insufficiency in blood supply.The tumor was removed completely along its edge.Under optical microscopy,the tumor was consisted of small round cells of the same size.Tumor cells were distributed around blood vessels in a nest manner or diffuse manner with brisk mitotic activity and focal necrosis. By using immunohistochemical staining,the tumor cells were diffusely positive for synaptophysin(Syn),CD56 and thyoid transcription factor⁃1(TTF⁃1),focal positive for cytokeratin(CK)and P53,and negative for growth hormone(GH),prolactin(PRL),adrenocorticotropic hormone(ACTH),follicle stimulating hormone(FSH),thyroid stimulating hormone(TSH),luteinizing hormone(LH),S⁃100 protein(S⁃100),thyroglobulin(TG)and calcitonin.Ki⁃67 labeling index was about 33%.ConclusionsPituitary metastasis is a rare tumor,and only a few cases of atypical lung carcinoid metastasis to the pituitary gland have been reported.Definite diagnosis could be made by history,typical histopathological characteristics and immunohistochemical expressions.
Lung neoplasms; Carcinoid tumor; Neoplasm metastasis; Pituitary gland;Immunohistochemistry;Pathology
10.3969/j.issn.1672⁃6731.2017.09.010
300350天津市环湖医院病理科
阎晓玲(Email:ll934065@126.com)
2017⁃06⁃22)
——中国居民收入分配中的逆向调节机制

