Effect of moxibustion on CRF and CRFR1 expressions in hypothalamus of TNBS-induced experimental colitis rats
Li Zhi-yuan (李志元), Huang Yan (黄燕), Zhang Ji (张霁), Yang Yan-ting (杨延婷), Wu Li-jie (吴丽洁),Zhi Fang-yuan (智方圆), Wu Dan-yan (吴丹艳), Li Xi-ying (李茜莹), Zhang Cui-hong (张翠红), Hong Jue (洪珏),Zhao Yue (赵越), Zhou Ci-li (周次利), Zhang Dan (张丹), Ma Xiao-peng (马晓芃),
Abstract Objective: To observe the effect of moxibustion on the protein and mRNA expressions of corticotropin-releasing factor (CRF)and corticotropin-releasing factor receptor 1 (CRFR1) in hypothalamus of trinitrobenzene sulfonic acid (TNBS)-induced experimental colitis rats, and to explore the central mechanisms of moxibustion in improving visceral pain and the pain-related emotions in experimental colitis rats.Methods: Thirty-six Sprague-Dawley (SD) rats were randomly divided into a normal group (NG), a model group (MG), a herb-partitioned moxibustion group (HPMG) and a sham herb-partitioned moxibustion group (SHPMG). Except the NG, rats in the remaining three groups all received TNBS enema to establish experimental colitis models. The HPMG received herb-partitioned moxibustion (HPM) at bilateral Tianshu (ST 25) and Qihai (CV 6) for intervention; for the SHPMG, the herbal cakes and moxa cones were only placed on the acupoints but not ignited; rats in the MG and NG were only fixed in the same way as those in the HPMG but did not receive any treatment. At the end of the intervention, the abdominal withdrawal reflex (AWR) score, the open field test (OFT) score and the elevated plus maze (EPM) score were observed to measure the changes in visceral pain and pain-related emotions of the rats. The enzyme-linked immunosorbent assay (ELISA)was used to examine the expressions of CRF and CRFR1 proteins in hypothalamus; the fluorescence-based quantitative polymerase chain reaction (PCR) was used to detect the expressions of CRF and CRFR1 mRNAs in hypothalamus.Results: Compared with the NG, the AWR score increased significantly and the OFT and EPM scores dropped significantly in the MG (all P<0.05), and the expressions of hypothalamic CRF and CRFR1 proteins and mRNAs increased significantly (all P<0.01). Compared with the MG and SHPMG, the AWR score dropped significantly and the OFT and EPM scores increased significantly in the HPMG (all P<0.01), and the expressions of hypothalamic CRF and CRFR1 proteins and mRNAs decreased significantly (all P<0.05). There were no significant differences between the MG and the SHPMG (all P>0.05).Conclusion: HPM can down-regulate the abnormally increased expressions of CRF and CRFR1 proteins and mRNAs in hypothalamus of the TNBS-induced experimental colitis rats, which is plausibly one of its action mechanisms in mitigating visceral pain and the pain-related emotions in the experimental colitis rats.
Keywords: Moxibustion Therapy; Point, Tianshu (ST 25); Point, Qihai (CV 6); Visceral Pain; Emotions; Corticotropin-releasing Factor; Corticotropin-releasing Factor Receptors; Rats
Inflammatory bowel disease (IBD), including Crohn disease (CD) and ulcerative colitis (UC), is an autoimmune disease, mainly manifested by abdominal pain, diarrhea, and mucus-like feces with pus or blood,etc[1]. Studies have shown that chronic pain might aggravate anxious emotion and the anxious emotion would trigger and maintain the pain, forming a vicious cycle[2-3]. Our previous study adopted the trinitrobenzene sulfonic acid (TNBS)-induced experimental colitis rat model to observe rat’s pain behaviors and pain-related emotions. The experiment found significant changes in rat’s pain behaviors and pain-related emotions in the model group compared with those in the normal group, presented by increased abdominal withdrawal reflex (AWR) score, and decreased mechanical withdrawal threshold (MWT),thermal withdrawal latency (TWL), open field test (OFT)score and elevated plus maze (EPM) score. The results showed that TNBS-induced colitis rats had obvious pain behaviors and pain-related emotions such as anxiety and depression, and these behaviors and emotions could be significantly eased by moxibustion[4]. Besides,numerous clinical and experimental studies have also proved that moxibustion can produce valid efficacy for colitis, mitigating the symptoms including abdominal pain and diarrhea[5-8]. Moxibustion may play its role in releasing the pain due to inflammatory bowel via regulating multiple targets in different ways and from different aspects, such as the expressions of inflammatory cytokines, proteins and genes, to correct the colonic mucus lesions[9]. However, it is still unclear how exactly moxibustion works to mitigate the negative emotions induced by visceral pain, and the relevant studies are rarely seen.
Corticotropin-releasing factor (CRF) is a 41-amino acid neuropeptide. As a crucial regulator in stress reactions, it activates various systems to respond to stress after binding with CRF receptor 1 (CRFR1) and CRF receptor 2 (CRFR2)[10]. It has been demonstrated that the production of pain and pain-related negative emotions are associated with CRF and its receptors[11].The increased production of CRF is considered associated with anxiety and affective disorders in pathophysiology and etiology[12]. An animal experiment also suggested that the hyper-expression of CRF could be to blame for typical symptoms related to stress,including anxiety, insomnia, decrease in appetite, low libido, and irritability[13]. Therefore, based on the previous study results, this experiment was to observe how hypothalamic CRF and CRFR1 change in an experimental colitis rat model and the regulatory effect of herb-partitioned moxibustion (HPM) on their expressions, for exploring the central mechanism of HPM in improving visceral pain and pain-related emotions in experimental colitis rats based on CRF and CRFR1.
1 Materials and Methods
1.1 Animals
Thirty-six healthy adult male Sprague-Dawley (SD)rats weighing (150±20) g were purchased from Shanghai Sippr-BK Laboratory Animal Co., Ltd., China [license number: SCXK(Hu)2013-0016]. The rats were housed in a room with a light/dark cycle (08:00-20:00 light;20:00-08:00 dark) at (20±1) ℃ with a relative humidity of 50%. After 1 week of adaptive feeding, the rats with normal behavior for ingestion and drinking were included in the investigation. This experiment was approved by the Ethics Committee on Use of Experimental Animals in Teaching and Research,Shanghai University of Traditional Chinese Medicine.
1.2 Main reagents and instruments
The following reagents and instruments were used:5% TNBS and pentobarbital (Sigma, USA); trizol(Invitrogen, USA); diethyl pyrocarbonate [DEPC, Jrdun Biotechnology (Shanghai), China]; chloroform,isopropanol and absolute ethyl alcohol (Sinopharm Chemical Reagent Co., Ltd., China); polymerase chain reaction (PCR) kits and reverse transcription kit(Thermal Cooperation, USA); RNaseI (Fermentas,Lithuania); PCR primers (Shanghai Generay Biotech Co.,Ltd., China); enzyme- linked immunosorbent assay(ELISA) kits (Wuhan Jiyinmei Biotechnology Co., Ltd.,China); centrifuge (model: 3K15, Sigma, USA); real-time detection system (model: mABI-7300, Biosystems, USA);microplate reader (Labsystems, Finland).
1.3 Methods
1.3.1 Model preparation and verification
By using a completely randomized grouping design,the 36 SD rats were allocated to one of the 4 groups: a normal group (NG), a model group (MG), a herb-partitioned moxibustion group (HPMG) and a sham herb-partitioned moxibustion group (SHPMG),with 9 rats in each group. Except the NG, the other three groups were developed into TNBS-induced experimental colitis models[14-15]. The rats were fasted for 24 h before the preparation of models. 50% ethanol was made from the mixture of absolute ethanol and double distilled water. Then TNBS and 50% ethanol were mixed at 2:1 to make TNBS enema solution. The rats were weighed and then anesthetized with 2%pentobarbital sodium intraperitoneally at 30 mg/(kg·bw)The TNBS enema solution was administered at 3 mL/(kg·bw) with the needle inserted into anus by 6-8 cm with a 1 mL syringe while the rat was held upside down. After enema, the rats were placed upside down for 1 min to prevent from leakage of the enema solution. The enema was conducted once every 7 d for 4 times in total. At the end of modeling, the rats were subjected to AWR test. Each group randomly contributed a rat for histopathological observation of colon [hematoxylin-eosin (HE) staining]. Interventions started once the model was confirmed a success.
1.3.2 Grouping and interventions
The NG and MG received no treatment but the same grasping and fixing as the HPMG.
The HPMG was intervened by HPM at Tianshu (ST 25)(bilateral) and Qihai (CV 6) points[16-17], 2 moxa cones for each point per time (about 10 min), once a day for 7 times in total. The herbal cakes were majorly made of Fu Zi (Aconiti Praeparata) powder which was mixed with yellow wine right before moxibustion. By using a specific mold, moxa wools were made into moxa cones,weighing 90 mg each. One moxa cone was placed on one herbal cake to ignite for moxibustion (Figure 1).
The SHPMG received same grasping and fixing as the HPMG[18-19]. The herbal cakes and moxa cones were only placed on Tianshu (ST 25) (bilateral) and Qihai (CV 6) but the moxa was not ignited, 10 min each time,once a day for 7 times.
1.3.3 Sample collection
Once the interventions were over, the rats were subjected to AWR test, OFT and EPM test. After anesthetic overdose, the hypothalamus tissues of rats were collected and kept at –80 ℃. Colons were collected (from the level of pubic symphysis to cecum)and opened longitudinally to remove membranes and connective tissues. Then 3 cm of each colon was remained and cut into 3 pieces after rinsed by 4 ℃normal saline. Two pieces were temporarily kept in liquid nitrogen and then transferred to an –80 ℃fridge after the sampling. One piece of colon was fixed in 4% formaldehyde, waiting for dehydration and embedding.

Figure 1. Illustration of HPM
1.4 Statistical methods
The SPSS version 18.0 software was used for statistical analysis. The data were first examined for normal distribution and homogeneity of variance. The measurement data that conformed to normal distribution were expressed as mean ± standard deviation (±s); those not conforming to normal distribution were expressed as median (min, max). For data in normal distribution, inter-group comparisons were analyzed by one-way ANOVA, and least significant different (LSD) was used for those with homogeneity of variance while Games-Howell was used for those with heterogeneity of variance. For data not conforming to normal distribution, a rank-sum test was employed.P<0.05 was indicative of statistical significance.
1.5 Observation items and detection methods
1.5.1 AWR
AWR was measured according to the method of Al-Chaer ED, et al[20]by giving a series of colorectal distending (CRD) stimuli: 20 mmHg, 40 mmHg,60 mmHg and 80 mmHg. Each rat was measured three times with each stimulus lasting 20 s at an interval of 5 min. The average value of the three measurements was considered as the final record.
1.5.2 OFT[21]
The detection room was kept quiet with stable room temperature and relative humidity. The rats were remained in cages for 30 min before placed in the operation box (90 cm × 90 cm × 90 cm) for OFT. The connected counter and computer were turned on to automatically record the number of horizontal and upright activities. Each rat was tested 5 min. Once a rat finished the test, the board inside the detection box would be cleaned with glacial acetic acid by a dry towel.The total distance and number of upright activities were subjected to statistical analysis.
1.5.3 EPM[22]
The rats were brought to the detection room 1 h prior to the test. The room was quiet and comparatively dark with stable temperature and humidity. Each rat was tested 5 min. The maze was cleaned every time at the interval with glacial acetic acid. The rat was placed at the platform which was in the center of the maze with its head right facing to one open arm. Then the rat was released to record its entry times into the open arm and the closed arm as well as the remaining time within the 5 min: open arm entry (OE), open arm time (OT),closed arm entry (CE) and closed arm time (CT). The percentage of open arm entry OE% = OE ÷ (OE + CE) ×100%; the ratio of the remaining time in the open arm OT% = OT ÷ (OT + CT) × 100%.
1.5.4 Histopathological observation of colon
The colon tissues were stained with HE and observed under light microscope to see the histopathological changes.
1.5.5 Detection of the protein contents of CRF and CRFR1 in rat’s hypothalamus
ELISA was used to determine the protein contents of CRF and CRFR1 in the hypothalamus by following the instruction.
1.5.6 Detection of the mRNA expressions of CRF and CRFR1 in rat’s hypothalamus
Fluorescence-based quantitative PCR was adopted to detect the expressions of CRF and CRFR1 mRNAs. The major steps included: extraction of total RNA;elimination of DNA in total RNA; reverse transcription of cDNA; real-time PCR amplification. The primers and probes are listed in Table 1.
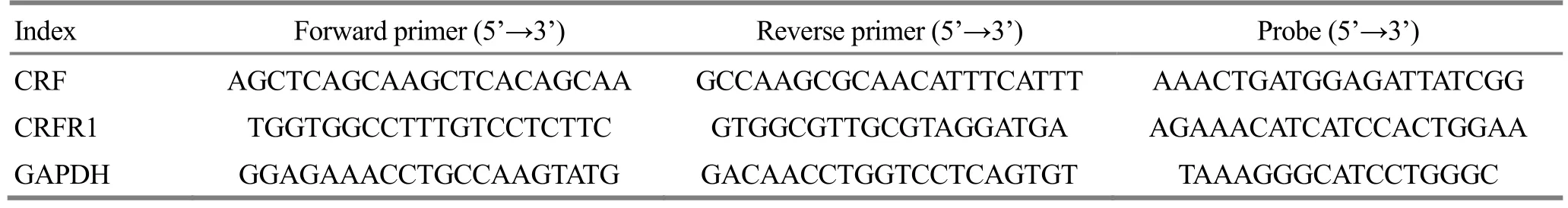
Table 1. PCR primers and probes of CRF and CRFR1 mRNAs
2 Results
2.1 Comparison of visceral pain and pain-related emotions
2.1.1 Comparison of the AWR score
The AWR scores were significantly higher in the MG than in the NG at different levels of CRD (all P<0.05).After the intervention, the AWR scores in the HPMG were significantly lower compared with those in the MG at different levels of CRD (all P<0.01). There were no significant differences in the AWR scores between the MG and SHMPG (all P>0.05). Compared with the HPMG,the AWR scores were markedly higher in the SHPMG at different levels of CRD (all P<0.01), (Figure 2).
2.1.2 Comparison of the OFT result
Compared with the NG, the total distance (horizontal movement value) and upright frequency (vertical movement value) were significantly reduced in the MG(both P<0.05). Compared with the MG, the total distance and upright frequency were significantly increased in the HPMG (both P<0.01). There were no significant differences in the total distance and upright frequency between the MG and SHPMG (both P>0.05).Compared with the HPMG, the total distance and upright frequency were significantly reduced in the SHPMG (both P<0.01), (Figure 3).
2.1.3 Comparison of the EPM result
Compared with the NG, OE% and OT% were significantly lower in the MG (both P<0.05). Compared with the MG, OE% and OT% were significantly increased in the HPMG after the intervention (both P<0.01). There were no significant differences in OE% and OT%between the MG and SHPMG (both P>0.05). Compared with the HPMG, OE% and OT% were significantly reduced in the SHPMG (both P<0.05), (Figure 4).
2.2 Histopathological changes in colon
In the NG, the colonic epithelium presented clear structure, complete mucosa, and well-arrayed glands,without congestion, swelling or ulcer (Figure 5-A).
In the MG, the colonic structure was significantly damaged with defect of mucosa; inflammatory cells infiltrated into mucosa and submucosa (Figure 5-B).
In the HPMG, the colonic structure was fine with substantially complete mucosa and well-arrayed glands;inflammatory cells could be seen in mucosa, together with mild swelling (Figure 5-C).
In the SHPMG, the colonic shape was irregular with obvious defect of mucosa; inflammatory cells infiltrated into mucosa and submucosa (Figure 5-D).
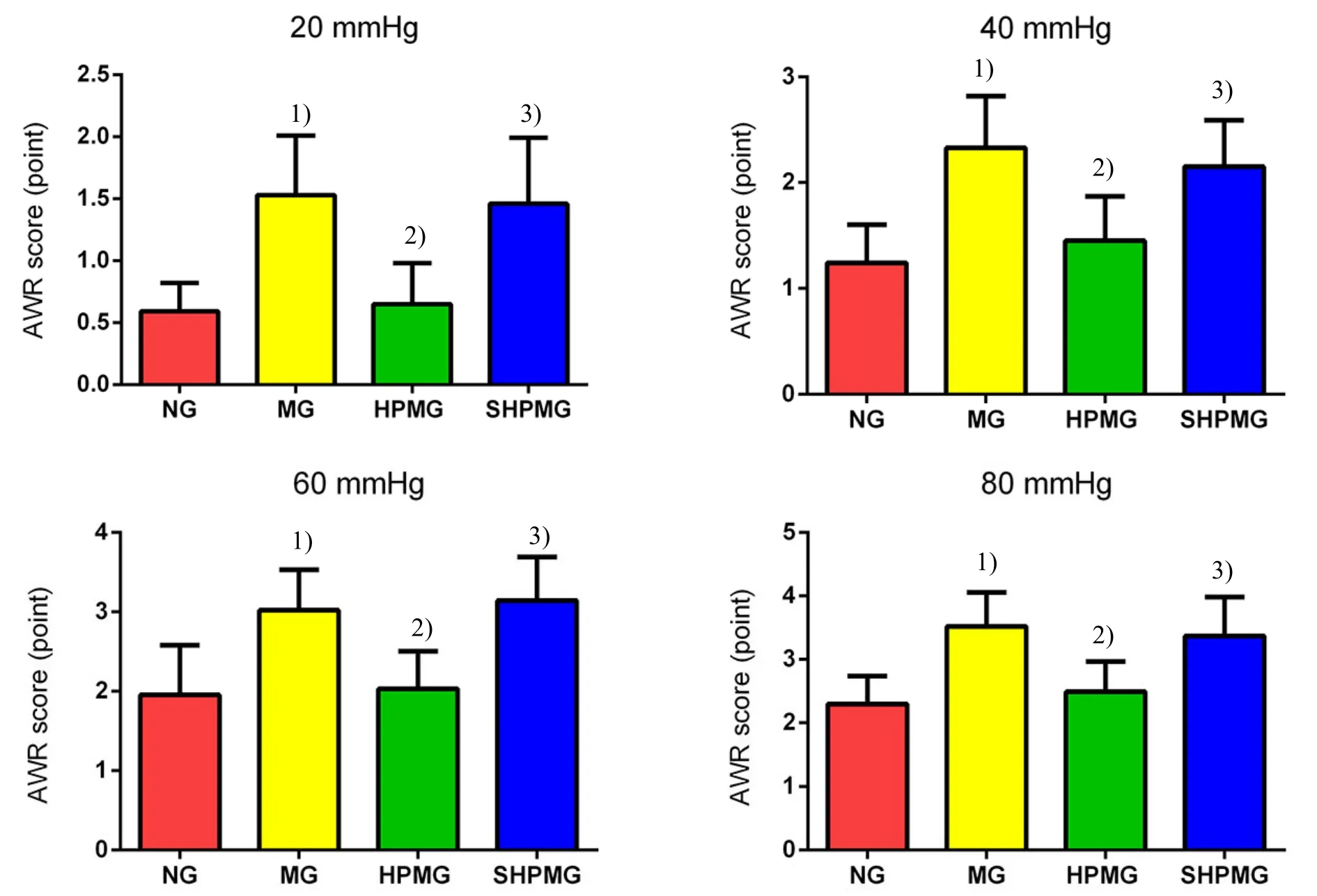
Figure 2. Comparison of the AWR score

Figure 3. Comparison of the OFT result

Figure 4. Comparison of the EPM result
2.3 Comparison of the contents of CRF and CRFR1 proteins in rat’s hypothalamus
Compared with the NG, the contents of CRF and CRFR1 proteins in rat’s hypothalamus were significantly higher in the MG (both P<0.01). Compared with the MG,the contents of CRF and CRFR1 proteins were significantly lower in the HPMG after the intervention(both P<0.05). There were no significant differences in the contents of CRF and CRFR1 proteins between the MG and SHPMG (both P>0.05). Compared with the HPMG, the contents of CRF and CRFR1 proteins were significantly higher in the SHPMG (both P<0.01),(Table 2).
Table 2. Comparison of the contents of CRF and CRFR1 proteins in rat’s hypothalamus (±s, ng/L)
Note: Compared with the NG, 1) P<0.01; compared with the MG, 2) P<0.05; compared with the HPMG, 3) P<0.01
Group n CRF CRFR1 NG 8 62.31±11.42 55.15±11.98 MG 8 143.74±16.821) 169.77±15.931)HPMG 8 87.92±16.232) 93.78±17.592)SHPMG 8 135.47±11.843) 152.17±23.603)
2.4 Comparison of the expressions of CRF and CRFR1 mRNAs in rat’s hypothalamus
Compared with the NG, the expressions of CRF and CRFR1 mRNAs in rat’s hypothalamus were significantly higher in the MG (both P<0.01). Compared with the MG,the expressions of CRF and CRFR1 mRNAs were significantly lower in the HPMG after the intervention(both P<0.05). There were no significant differences in the expressions of CRF and CRFR1 mRNAs between the MG and SHPMG (both P>0.05). Compared with the HPMG, the expressions of CRF and CRFR1 mRNAs were significantly higher in the SHPMG (both P<0.01),(Table 3).
Table 3. Comparison of the expressions of CRF and CRFR1 mRNAs in rat’s hypothalamus (±s, ×10-3)

Table 3. Comparison of the expressions of CRF and CRFR1 mRNAs in rat’s hypothalamus (±s, ×10-3)
Note: Compared with the NG, 1) P<0.01; compared with the MG, 2) P<0.05; compared with the HPMG, 3) P<0.01
?
3 Discussion
International Association for the Study of Pain (IASP)defines pain as ‘an unpleasant sensory and emotional experience associated with actual or potential tissue damage’[23]. This implies that pain contains two elements: sensory discrimination and affective dimensions. The former mainly encodes and experiences the nature of stimulation, including its property, intensity and site, etc.; the latter refers to the feature of emotion and affection, involving negative emotions such as hatred, anxiety and fear induced by nociceptive stimuli. Inflammatory visceral pain is commonly seen in chronic colitis patients, while moxibustion can produce satisfactory effect in easing the pain[5,7,24]. It has been proved that TNBS-induced experimental colitis model has significant inflammatory visceral pain[25]. Many studies have focused on inflammation-induced visceral pain and have achieved a great progress[26-27]. However, regarding the emotional changes triggered by visceral pain, such as anxiety and depression, relevant studies are rarely seen. More and more clinical observations have shown that, anxiety,depression and fear, these negative emotions experienced by the chronic pain patients bring more serious psychosomatic harm than pain itself[28].Therefore, further studies targeting this subject are crucial. Our previous study found that experimental colitis rats manifested emotional changes caused by visceral pain, including anxiety and depression[4].
Hypothalamus resides on the ventrolateral side of the brain. As an important component of the hypothalamicpituitary-adrenal axis (HPA), it produces a variety of hormones and factors including CRF, thyrotropinreleasing hormone (TRH), growth hormone-releasing hormone (GHRH) and melanocyte-stimulating hormone releasing factor (MRF), participating in a wide range of stress reactions in mental and endocrine systems[29-30].In recent years, constant studies have indicated that various hormones and receptors produced by hypothalamus are involved into the negative emotions such as anxiety, depression and fear[31-33]. As a type of brain-gut peptides, CRF works together with other peptides to modulate the function of HPA under stress,coordinating the stress responses of endocrine system,autonomic nervous system, immune system, physiology and behavior. CRFRs are a typical type Ⅱ G proteincoupled receptor family. There are two receptors in the family, which have biological activities, designated as CRFR1 and CRFR2. Their binding with CRF can lead to different biological effects, modulating the function of nervous, endocrine and gastrointestinal systems[34]. CRF plays a crucial role in regulating metabolism,neuroendocrine and response to external stimuli[35].When triggered by stresses, hypothalamic paraventricular nucleus increases the secretion of CRF to adapt to the stimuli to maintain the balance among different organs and tissues and the production of adrenocorticotropic hormone (ACTH). The increase in CRF is considered as the essential factor causing increased activity of HPA and also a factor associated with anxiety and affective disorders in pathophysiology and etiology[12]. It has been found through clinical observation that people with mental disorders such as depression, anxiety and suicide attempt present a significantly higher level of hypothalamic CRF than normal people[36]. By observing rat models with early-stage posttraumatic stress disorder (PTSD), Li CT,et al[37]found that rats in the stress group manifested more significant anxiety and depression with an increased expression of hypothalamic CRFR1. They also discovered that after intervention with CP-154, 526, a CRFR1 antagonist, the expression of CRFR1 was inhibited and rat’s anxiety and depression symptoms were released. The results showed that CRFR1 plays an important role in the development of anxiety and depression. Cipriano AC, et al[38]also proved the role of CRFR1 in causing anxiety by adopting a mouse model.Major depressive disorder (MDD) is a destructive disease and has affected over 0.3 billion people worldwide. Recent clinical and preclinical studies on genetic screening and genetically modified rodent models found that CRFR1 mRNA plays a significant role in the development of MDD and the wide distribution of CRFR1 mRNA in brain tissues regulates both short-term and long-term response to social and environmental stresses[39].
In recent years, the role of CRF and its receptors in pain and pain-related negative emotions such as anxiety and depression has drawn much attention. Chronic pain is a stressor that can cause over-expression of CRF to act on CRFR1, leading to pain sensitization; by stimulating certain areas of the brain including central amygdala,paraventricular nucleus and locus coeruleus, the over-expressed CRF also results in a series of painrelated negative emotions such as anxiety, depression and fear, which may exacerbate the chronic pain via influencing some neural pathways[11].
In this study, the rat model of TNBS-induced inflammatory visceral pain was adopted. After modeling,rats in the MG had significantly higher pain behavior score and lower pain-related emotion scores than rats in the NG, which conformed to the previous study results[4]. The expressions of hypothalamic CRF and CRFR1 proteins and mRNAs in rats in the MG were significantly higher than those in the NG (P<0.01),suggesting that hypothalamic CRF and CRFR1 may play an important role in the development of chronic inflammatory visceral pain and the regulation of the subsequent anxiety, fear and depression emotions in rats. After HPM intervention, the expressions of hypothalamic CRF and CRFR1 proteins and mRNAs decreased. In combination with the changes in painrelated behaviors and emotions, the results indicated that the decrease in the expressions of hypothalamic CRF and CRFR1 may be one of the action mechanisms of HPM in releasing visceral pain and pain-related emotions in chronic inflammatory visceral pain rats.Thus, we may conclude that when stimulated by chronic inflammation, rat’s hypothalamus will increase the transcription of CRF and CRFR1 mRNAs, as well as the expressions of their proteins, to activate the CRF-CRFR1 signaling pathway, leading to visceral pain and pain-related emotions such as anxiety and depression; HPM can inhibit the activation of the CRF-CEFR1 signaling pathway to mitigate visceral pain and the pain-related emotions of the experimental colitis rats.
Conflict of Interest
The authors declared that there was no potential conflict of interest in this article.
Acknowledgments
This work was supported by National Natural Science Foundation of China (国家自然科学基金项目, No.81674073, No. 81273843); Excellent Academic Leader Cultivation Project of Shanghai Municipal Commission of Health and Family Planning (上海市卫生计生系统优秀学科带头人培养计划项目, No. 2017BR047); National Basic Research Program of China (973 Program, 国家重点基础研究发展计划项目, No. 2015CB554501); Project of Shanghai Municipal Commission of Health and Family Planning (上海市卫生和计划生育委员会课题,No. 201540167).
Statement of Human and Animal Rights
The treatment of animals conformed to the ethical criteria in this experiment.
Received: 8 November 2017/Accepted: 10 December 2017
 Journal of Acupuncture and Tuina Science2018年4期
Journal of Acupuncture and Tuina Science2018年4期
- Journal of Acupuncture and Tuina Science的其它文章
- Therapeutic efficacy observation on acupuncture for persistent allergic rhinitis
- Effects of acupuncture on ovarian blood supply and pregnancy outcomes in patients receiving assisted reproduction
- Effect of Governor Vessel-unblocking and mindrefreshing acupuncture plus functional training on neural development in infants with brain damage
- Correlation analysis on clinical effects of acupuncture for elderly patients with sensorineural deafness and ear distending sensation
- Observation of therapeutic effects of point application at Shenque (CV 8) plus moxa-salt hot compress for prevention of gastrointestinal adverse reactions after chemotherapy for non-Hodgkin lymphoma
- Application and exploration of suspended magnetic moxibustion cup for obesity
