Carcinoma ex pleomorphic adenoma of the trachea:A case report
Heng-Xing Gao,Quan Li,Wen-Li Chang,Ya-Long Zhang,Xiao-Zhi Wang,Xue-Xue Zou
Abstract
Key words: Case report;Carcinoma ex pleomorphic adenoma;Trachea;Pleomorphic adenoma
INTRODUCTION
Pleomorphic adenoma is the most common benign tumor of the salivary glands.Approximately 6% of pleomorphic adenomas have the potential to transform into carcinoma ex pleomorphic adenoma (CXPA)[1].The main histopathological finding in CXPA is the co-existence of the benign characteristics of pleomorphic adenoma with malignant changes in the epithelial components of the tumor.CXPA mainly involves the major salivary glands,of which the parotid gland is the most commonly involved,followed by the submandibular gland[2].Tracheal CXPA is an exceedingly rare entity.Herein,we present a case of CXPA arising in the trachea,and a review all cases of tracheal mixed malignant tumors reported in the literature.
CASE PRESENTATION
Chief complaints
A 56-year-old woman was admitted to our hospital with a complaint of progressive dyspnea over the last 3 mo.
History of past illness
The patient had no history of disease in the head and neck region.Her past history was unremarkable.
Personal and family history
The family history was unremarkable.
Physical examination
The patient's inspiratory phase was prolonged and the inspiration was laborious.There were wheezing,laryngeal ringing,and three depressions sign can be seen.Her temperature was 36.8 °C,heart rate was 102 bpm,respiratory rate was 26 bpm,blood pressure was 133/86 mmHg and oxygen saturation in room air was 96%.
Laboratory examinations
Blood analysis revealed normal.The blood biochemistries,as well as urine analysis were normal.
Imaging examinations
A computed tomography scan of the neck and thorax revealed an inhomogeneous,broad-based lesion arising from the tracheal wall on the right side.The lesion measured 1.8 cm × 1.7 cm.Calcification was observed in the anterior part of the lesion(Figure 1).On bronchoscopic examination,a subglottic neoplasm was observed at approximately 5 cm from the carina.The tumor caused up to 90% luminal stenosis of the trachea (Figure 2).
FINAL DIAGNOSIS
Take together,a final diagnosis of primary CXPA of the trachea was established.
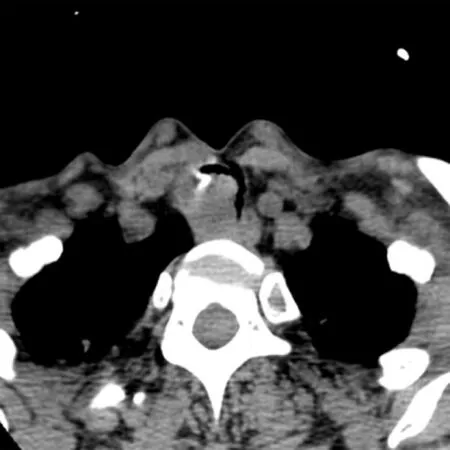
Figure1 Computed tomography scan showing an inhomogeneous,broad-based lesion arising from the tracheal wall on the right side.
TREATMENT
The tumor was resected using a high-frequency electrosurgical snare combined with argon plasma coagulation (APC).At 30 min before the operation,the patient was anesthetized with 5 mL of 2% lidocaine (inhaledviaoxygen-driven atomization) and an intranasal drip of lidocaine combined with 1% furosemide.Propofol 20 mg and fentanyl 100 mg were intravenously administered before surgery.During the surgery,intravenous propofol was administered through a micropump (2-4 mg/kg/h).Throughout the treatment,the patient’s pulse,oxygen saturation,respiration,and blood pressure were dynamically monitored.Routine nasal insertion of a bronchoscope was performed to reach the lesion site.A high-frequency electrosurgical snare and an APC catheter were inserted into the airway through the bronchoscope.The power supply for electrocutting (35-40 W) and electrocoagulation (30-35 W) was turned on at the same time.To resect the tumor,we placed the snare near the base of the tumor and slowly closed it around the tumor pedicle while simultaneously applying electrocoagulation.
For the remaining tumor tissue in the basal part,we placed the electrocoagulation probe on the lesion and applied a current for 0.5-1.0 s.Electrocoagulation was performed multiple times to coagulate and vaporize the lesion.The necrotic tissues were removed using biopsy forceps or bronchoscopic suction.The surgical field was intermittently rinsed with a cold saline solution containing adrenaline (dilution,1:10000) to maintain a clear view.The depth of electrocoagulation did not exceed 3 mm.After APC treatment,jelly-like cellulosic exudates and necrosis may form and lead to airway obstruction;these need to be cleaned regularly by using biopsy forceps or bronchoscopic suction.
Histopathological examination
On histopathological examination,benign pleomorphic adenoma-like areas and large malignant cells with pleomorphic and prominent nucleoli were recognized (Figure 3).The tumor was composed of glandular and tubular structures along with myoepithelial cells within stromal elements,which was suggestive of a pleomorphic adenoma.In the epithelial areas,solid nests and cords of polygonal tumor cells were observed.The adjacent areas showed chondromyxoid materials.The solid nests had a cribriform pattern,and were associated with dense hyalinized stroma,which was incorporated into the tumor islands and sheets.The cribriform pattern was suggestive of adenoid cystic carcinoma (Figure 4).
Immunohistochemistry revealed strong immunoreactivity with cytokeratins in both the ductal epithelial cells and myoepithelial cells.The tumor was negative for glial fibrillary acidic protein.The myoepithelial cells were positive for smooth muscle actin,the myoepithelial marker P63,vimentin,and CD43.Staining for s-100 protein and CD117 was positive in the ductal epithelial cells.Alcian blue staining was positive in the mucous-like substance that filled in the sieve-like structure of the tumor cells.Periodic acid-Schiff staining was positive in the luminal contents of the gland.
OUTCOME AND FOLLOW-UP
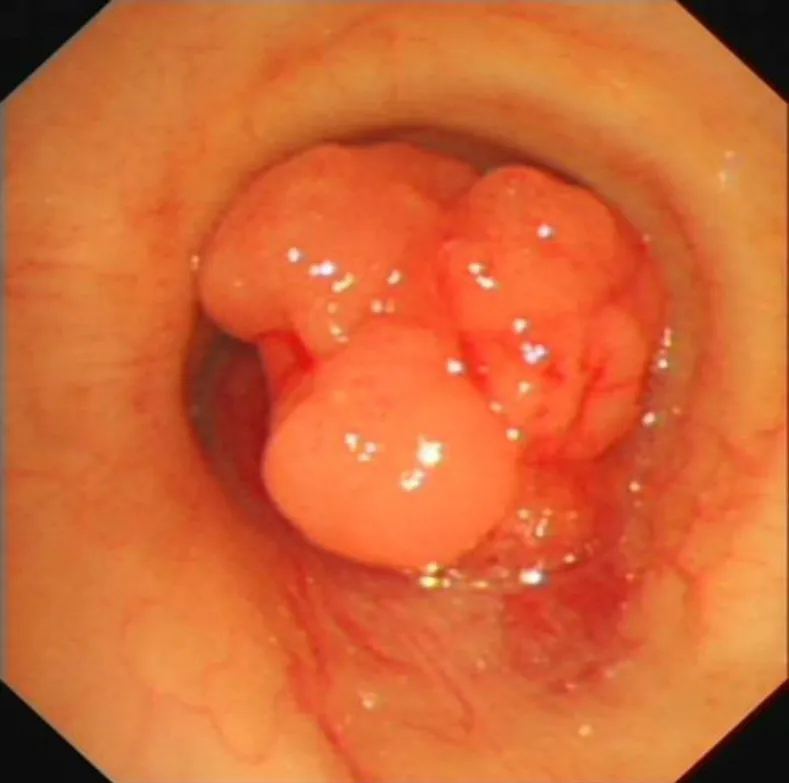
Figure2 Bronchoscopic examination showing a subglottic neoplasm causing up to 90% luminal stenosis of the trachea.
At 6 d after the tumor resection,the patient was well and was discharged.Unfortunately,fiberoptic bronchoscopy revealed tumor recurrence after 11 mo.The patient again underwent treatment with a high-frequency electrosurgical snare combined with APC.Additionally,postoperative radiotherapy (60 Gy) was performed.The patient has been well for 10 mo until now after the second surgery.
DISCUSSION
CXPA is defined as an epithelial malignancy arising in or from a primary or recurrent benign pleomorphic adenoma[1,3-4].This tumor most commonly affects the salivary glands.Primary CXPA of the tracheobronchial system has been reported only infrequently.The pathogenesis of CXPA is unknown.Choobacket al[5]proposed a role for the deficiency of some genes,such as those on chromosomal arms 8q,12q,and 17p.Kimet al[6]suggested that the accumulation of genetic instabilities was the main cause of malignant transformation in pleomorphic carcinoma.The above hypotheses were based on salivary gland tumors,and it is unclear whether these apply to CXPA of the tracheobronchial system.
Malignant mixed tumors of the salivary glands classically encompass three distinct tumors:CXPA,carcinosarcoma,and metastasizing pleomorphic adenoma[7].A review of the literature disclosed 11 previous cases of primary malignant mixed tumors of the trachea and bronchus[8-13].Of these,only four cases (Dinget al[10],Demirağet al[11],Hemmiet al[12],and Moriet al[13]) involved the trachea (Table 1);the others involved the hilum and/or bronchi.In the case reported by Hemmiet al[12],no foci of benign pleomorphic adenoma were found in the primary tumor.This indicates that the tumor was a malignant pleomorphic adenoma,and not a CXPA.Thus,only three cases of true primary CXPA of the trachea have been reported.The present case is the fourth report of a primary CXPA of the trachea.
A review of the four previous cases of tracheal malignant mixed tumors showed that the ages of the patients ranged from 56 to 69 years;there were two women and two men.Our patient was a 55-year-old woman.The common clinical symptoms were cough,asthma,and dyspnea;hoarseness was reported by Moriet al[13].Thus,tracheal CXPA may not have distinct symptoms.On imaging examination,no calcification could be seen in the previous four cases,but calcification was present in our patient.
The diagnosis of CXPA requires the presence of both the pleomorphic adenoma component and the malignant component.The presence of cohesive clusters of ductal cells,a background of myoepithelial cells,dense fibrillary metachromatic matrix,atypical cells,an abnormal chromatin pattern,and necrosis are essential to make a diagnosis of CXPA.In our patient,benign pleomorphic adenoma-like areas and large malignant cells with pleomorphic and prominent nucleoli were recognized on histopathological examination,confirming the diagnosis.The most common malignant component in CXPA is adenocarcinoma.Other malignant components include adenoid cystic carcinoma,myoepithelial carcinoma,and salivary duct carcinoma,and rarely acinic cell carcinoma,epithelial-myoepithelial carcinoma,basal cell carcinoma,myoepithelial carcinoma,squamous cell carcinoma,and clear cell carcinoma[14].In our patient,the malignant component was an adenoid cystic carcinoma.The malignant component in the case reported by Dinget al[10]was an adenocarcinoma,while the type of malignant component was not mentioned in the cases reported by Demirağet al[11]and Moriet al[13].
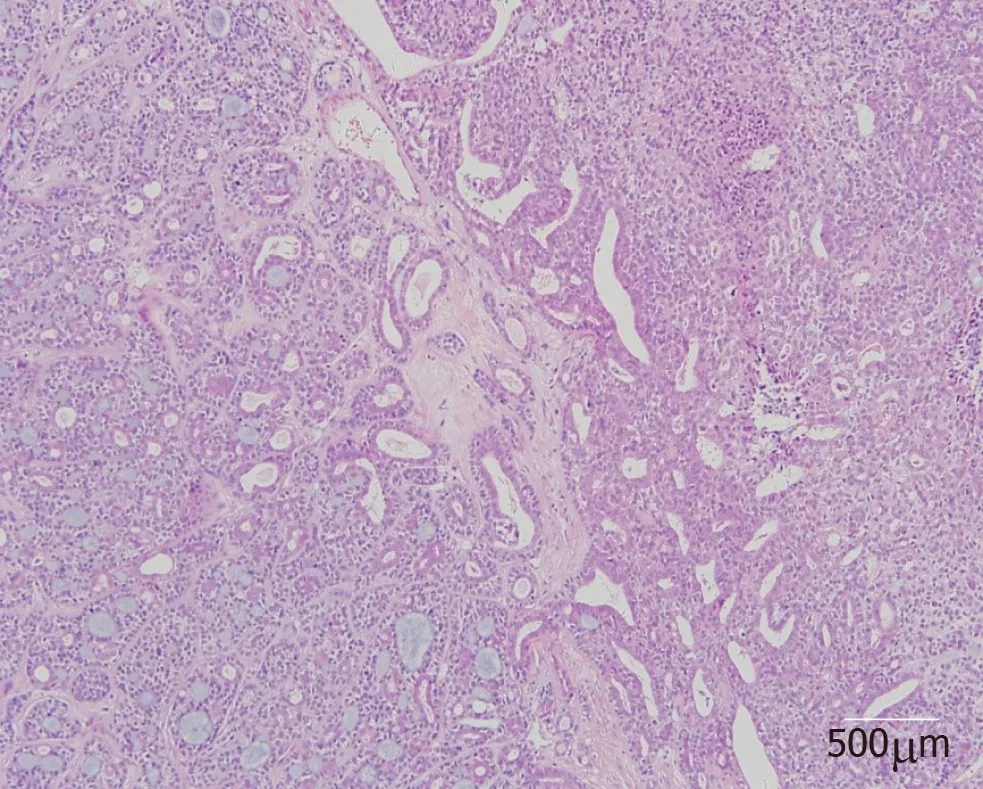
Figure3 Microscopic examination of the resected specimen showing a biphasic composition with benign histological characteristics suggestive of pleomorphic adenoma and malignant changes in the epithelial components (hematoxylin and eosin).
Given the rarity of tracheal CXPA,no standard systemic therapy options have been established.Surgery appears to be the primary treatment modality,and postoperative radiotherapy may be used in patients with poor prognostic factors,such as stage III/IV disease,perineural invasion,and distant metastasis[15].Endoscopic resection is simple,convenient,safe,and effective,and is associated with minimal injury and rapid recovery.It is widely applied in the diagnosis and treatment of benign airway stenosis,including that caused by tracheobronchial pleomorphic adenoma[16].However,Gaissertet al[17]noted that bronchoscopic resection does not provide confirmation of the resection margins and can leave tumor behind,which leads to tumor recurrence.Studies on the endoscopic resection of tracheal tumors have not provided long-term follow-up data[18].In the three previous reports of primary tracheal CXPA,all patients were treated conservatively with complete excision.For our patient,we successfully performed endobronchial resection of the tumor with a high-frequency electrosurgical snare and laser ablation.Demirağet al[11]and Moriet al[13]performed postoperative radiotherapy for their patients.Postoperative radiotherapy was not performed by Dinget al[10]and in the present case.The necessity and benefits of postoperative radiotherapy remain unclear at present.If distant metastases are present,effective regional radiation in addition to resection may provide meaningful palliation.The three previous patients were free of disease for 3 mo[9],16 mo[12],and 30 mo[10]after tumor resection.In our patient,the tumor recurred after 11 mo.However,whether bronchoscopic resection and the lack of postoperative radiotherapy led to tumor recurrence in our patient cannot be definitively stated at present.
CONCLUSION
In conclusion,given the rarity of CXPA in the trachea,no standard systemic therapy options have been established.Endoscopic resection is a simple,safe,minimally invasive,and effective method for treating CXPA patients.

Table1 Clinical features of the four patients with carcinoma ex pleomorphic adenoma of the trachea
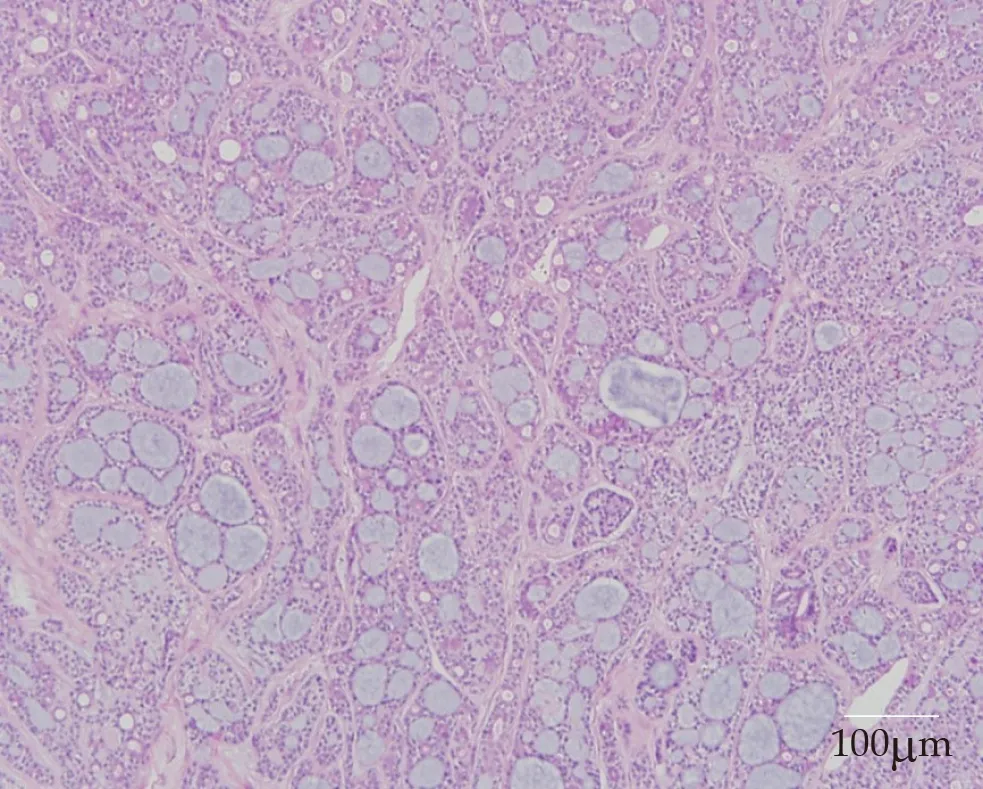
Figure4 Microscopic examination of the resected specimen showing solid nests in a cribriform pattern associated with hyalinized stroma,which is incorporated into the tumor islands and sheets (hematoxylin and eosin).
 World Journal of Clinical Cases2019年17期
World Journal of Clinical Cases2019年17期
- World Journal of Clinical Cases的其它文章
- Multifocal G1-G2 gastric neuroendocrine tumors:Differentiating between Type I,II and III,a clinicopathologic review
- Attention deficit hyperactivity disorder and comorbidity:A review of literature
- Dietary manipulation and testosterone replacement therapy may explain changes in body composition after spinal cord injury:A retrospective case report
- Risk factors,clinical features,and short-term prognosis of spontaneous fungal peritonitis in cirrhosis:A matched case-control study
- Incidence of portal vein thrombosis after splenectomy and its influence on transjugular intrahepatic portosystemic shunt stent patency
- Multiplex gene expression profile in inflamed mucosa of patients with Crohn’s disease ileal localization:A pilot study
