Endoscopic ultrasound guided liver biopsy for parenchymal liver disease
Aun Raza Shah, Muhannad Al-Hanayneh, Monica Chowdhry, Mohammad Bilal, Shailendra Singh
Abstract
Key words: Liver biopsy; Endoscopic ultrasound; Endoscopic ultrasound guided liver biopsy; Liver disease
INTRODUCTION
Liver biopsy plays an essential role in the diagnosis, evaluation and management of a vast proportion of liver diseases. History, physical exam, laboratory testing and radiological exams continue to be the mainstay in diagnosis of disease, however, the use of these modalities without liver biopsy can miss up to one-third cases of cirrhosis[1]. Histological examination of biopsy samples can not only help identify the underlying pathophysiology of liver disorder but also quantify its severity. This has a significant impact on the management of as many as one-fifth of all patients with liver disease[2]. In the past, liver biopsy was performedviathe percutaneous route without image guidance[3]. However this has now been largely replaced by ultrasound-guided or computed tomography (CT) guided biopsy to limit potential complications[4,5].When a percutaneous biopsy is not feasible a trans-jugular approach is used. Open or laparoscopic surgical biopsy is usually last resort. Endoscopic ultrasound guided liver biopsy (EUS-LB) is a technique that has recently gained popularity since it offers certain advantages over the traditional methods of obtaining tissue samples.Endoscopic ultrasound is an established imaging modality that is essential in the assessment of a broad array of luminal, hepatobiliary, and pancreatic disorders. It provides high resolution images of both lobes of the liver, hence allowing a potentially easier and safer biopsy technique whilst providing the opportunity to target focal hepatic lesions[6]. The choice of technique is eventually based upon expertise of the operator, anatomical barriers and risk profile of the patient(coagulopathy, hepatic vascularity and presence of ascites). In this review, we provide a detailed comparison between EUS-LB and traditional modalities of liver biopsy.
APPROACHES TO LIVER BIOPSY
The advent of liver biopsies is dated back to the 19th century, with Paul Ehrlich reporting the first successful liver aspiration in 1883[4,7]. However, it wasn't until four decades later that the first percutaneous liver biopsy was successfully performed in Germany in 1923[4,5]. Even a century later this remains the preferred approach to obtaining hepatic parenchymal tissue[3]. Over time, advances in imaging modalities have led to the addition of ultrasound and CT scan guided liver biopsy[5,8].
Previously percutaneous liver biopsy (PC-LB) was performed “blindly” using percussion to identify the liver anatomy[3]. This has now largely been replaced by image-guidance, either by ultrasonography or CT scan[8]. Most commonly large gauge needles (16-18) are used, although depending on expertise smaller needles are also utilized at some centers[9]. Percutaneous biopsy can be classified as transthoracic(transpleural) or subcostal depending on the site of entry. This requires an enlarged liver extending below the diaphragm for a safe approach. Pain, bleeding, infection,peritonitis, pleural injury resulting in pneumo- or hemo-thorax continue to be common complications of percutaneous biopsy[9,10]. Image guidance partly mitigates these risks, but studies have reported adverse event rates up to 1%[3,10].
Trans-jugular biopsy of the liver emerged as a viable technique in the 1960s based on the works of an interventional radiologist - Charles Dotter[11]. Over time it has become an accepted and safe alternative to percutaneous biopsy in select settings[12].The internal jugular vein is cannulated to gain access to the hepatic vein, allowing tissue acquisition without the need to traverse the liver capsule[13]. This approach is preferred in patients who have coagulopathy, hepatic peliosis, large volume ascites or morbid obesity[12]. Rates of success have been reported as high as 97% and the complication rates as low as 1.3%[14]. Complications include hepatic capsule perforation, major hemorrhage, pain from hematoma, hemobilia, arterial aneurysms and arrhythmias[12]. Fortunately however, major complications are rare and minor bleeding from the access site and transient abdominal pain from hematomas are the most commonly reported adverse events[14,15].
EUS was developed in the 1980s and has been gaining popularity. This was further revolutionized in the early 1990s with the advent of Fine Needle Aspiration (FNA)[16].Significant advances have been made since then and now EUS is widely used as both a diagnostic and therapeutic modality. EUS-LB has recently emerged as another technique for obtaining liver tissue. Although as described earlier; several approaches and techniques are there for obtaining a liver biopsy, EUS-LB offers several advantages over conventional approaches. EUS offers a more precise localization and characterization of target tissue which helps to improve diagnostic yield[17,18]. More so,it is arguably a less invasive and better tolerated approach than conventional methods[15,19]. It offers the advantage of good access to both the lobes of liver and the presence of doppler assistance decreases the chances of complications[20]. Other important considerations for choosing EUS-LB over conventional methods of liver biopsy include contraindications to percutaneous biopsy.
EUS GUIDED SAMPLING TECHNIQUES FOR PARENCHYMAL LIVER DISEASE
Since the onset of EUS-LB, multiple needle types and techniques have been reported for its use. In the next few segments, we review the historic timeline for various needle types and discuss the different techniques used to help in increasing the diagnostic yields of EUS-LB. Core sample obtainedviaEUS-LB is shown in Figure 1.
How is a good quality liver biopsy defined?
The criteria for an adequate liver biopsy had been well defined. Per the American Association for the Study of Liver Disease (AASLD), adequacy of samples are defined as number of complete portal triads (CPTs) to be 11 and total sample length (TSL) of 30 mm, and with no or minimum fragmentation of the sample[21]. However, the definition of adequacy for liver biopsy sample remains controversial in the literature[22-26].
Needle types
Tru-cut biopsy: In 2002, the initial experience with EUS-LB was in swine models using Tru-Cut biopsy needles. In a study by Wiersemaet al[27], they performed EUS-LB of multiple peri-gastric organs using a 19 gauge Tru-Cut needle. The median TSL was 4 mm for liver samples and 78% had fragmentation, however the number of CPT was not reported. They reported difficulty in the procedure due to the use of the stiff needle since problems were encountered in making the needle bend to traverse through the flexible endoscope. They concluded that the method is safe and feasible,however did not meet criteria for adequate liver biopsy samples and were technically difficult. Due to the aforementioned reasons this method was not widely used.
However, in 2009, Gleesonet al[28]also reported outcomes using the Tru-Cut needle.They reported that results of EUS Tru-Cut needle biopsy are comparable to those of trans-jugular liver biopsy. In their small study with the use of Tru-Cut needle on 9 patients, they reported the TSL of 16.9 mm and a median of 7 CPTs. Although the results do not suffice the criteria of having at least 11 CPT per AASLD[21], they were able to reach a histopathologic diagnosis in all 9 patients. However, the study was retrospective and only included 9 patients.
Overall, the EUS Tru-Cut biopsy did not gain wide spread popularity for diagnosing parenchymal liver disease and more novel needles and techniques emerged which made Tru-Cut biopsies fall out of favor.
19 Gauge FNA “non tru-cut” needle:Several studies reported using 19 gauge FNA needle, with the first one published in 2012[24]. In this study, Stavropouloset al[24]performed EUS-LB on patient undergoing EUS to rule out biliary obstruction when the exam was unrevealing. The median length of obtained specimens was 36.9 mm ranging from 2 to 184.6 mm, nine complete portal tracts (range: 1-73), diagnostic adequacy of 91%, and no post-procedure complications. The outcomes showed comparable biopsy quality results to percutaneous and trans-jugular liver biopsies.They concluded that for patients being investigated by endoscopic ultrasound for biliary obstruction; EUS-LB was a safe, reliable and cost-effective option to diagnose parenchymal disease.
In one large study published in 2015 by Diehlet al[29], liver biopsy specimens obtainedviaEUS were sufficient for pathological diagnosis in 98% of the cases. The aggregate length of tissue acquired ranged from 0 to 203 mm with a median of 38 mm.A total of 0 to 68 CPTs were obtained and the median was 14. This led the authors to conclude that EUS-LB using a 19 gauge FNA needle, is a safe technique yielding adequate tissue for pathological diagnosis in 98% of the patients.
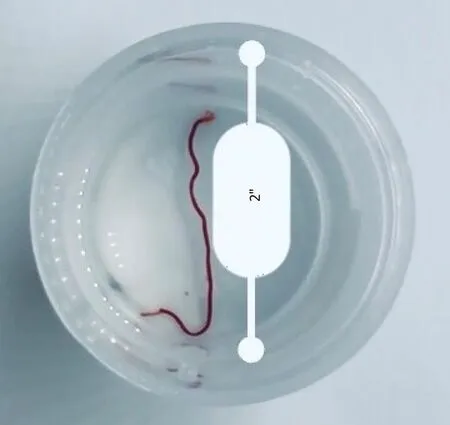
Figure 1 Core biopsy sample obtained via endoscopic ultrasound guided liver biopsy.
This needle provides a higher diagnostic yield and is less technically challenging to use in comparison with the Tru-Cut biopsy needle. However, the ideal technique has not been yet defined and larger studies are needed. Different biopsy techniques are discussed in the next section.
19 Gauge Fine Needle Biopsy needle:A new 19 gauge fine needle biopsy (FNB)needle has shown promising results and a higher diagnostic yield. Schulmanet al[30]compared the different needle types and biopsy techniques. They studied 6 different needle types (four EUS-LB needles and two percutaneous needles) on human cadaveric tissue and had a total of 288 liver samples. They concluded that a novel 19 gauge needle (SharkCore 19 gauge FNB needle) had significantly better diagnostic yield compared to all other needle types in the study including the second FNB needle used in the study, the ProCore FNB (Echo Tip HD ProCore).
In this study four discrete suction techniques were used in addition to one fanning passvsthree fanning pass patterns of needle excursion. Analysis of the subgroups showed that three fanning pass needle excursion pattern was an independent prognosticator of CPT, however the suction techniques had no effect on the adequacy of the tissue sample when other variables were controlled. This type of needle also had overall less tissue fragmentation rates compared to the other needles with an 84%mean of core samples from tissue obtained using this needle. This study was double blinded and randomized, however was done on ex-vivo on cadaveric tissue. This needle type seems to have a promising future, however more studies need to be done on non-cadaveric diseased liver with comparison to other biopsy modalities to confirm its superiority and overall cost-effectiveness.
Biopsy techniques
Several techniques have been used to increase the diagnostic yield of EUS-LB. The technique for performing EUS-LB is demonstrated in Video 1. Diehlet al[29]reported performing multiple movements with the needle “fanning technique” in which the needle is advanced to-and-fro at different areas to obtain tissue samples[31].
Most endoscopists use full suction with needle aspiration as well. Suction techniques include ten-/twenty-/thirty-mL method. Alternatively, a slow-pull technique may be used where the stylet is drawn out from the needle once it is in the desired location[7].
More recently, newer techniques have emerged in attempts to increase the diagnostic yields of EUS-FNB including the use of “wet suction”. In this technique a heparinized needle is used to reduce chances of coagulation and hence, improve tissue retrieval whilst minimizing comminution of tissues samples. A recent study by Moket al[32]compared this method to both “dry heparin” and “dry needle” technique.This was a prospective study on 40 patients, were they all had 3 EUS-FNA liver biopsies using the 3 different methods. In this method, needles are heparinized till drops are seen at the needle-point while ensuring no air is pushed through. Two milliliters of water are then drawn into the syringe and a twenty-milliliter vacuumsyringe is connected. They concluded that “wet suction” technique had better tissue yield in comparison to “dry needle” method. However, the question remains if this technique is necessary or even useful when using the more novel FNB needles as these needles provided superior results regardless if wet suction was used or not.
Another recently described technique is the “modified 1-pass 1 actuation wet suction technique [EUS-modified liver biopsy sampling (EUS-MLB)]”. This was described in a study by Nietoet al[33]They used the FNB-needle (SharkCore) which was prepped normal saline. Suction was applied to the FNB-needle at a depth of seven cm into the hepatic parenchyma. Large vessels were avoided using Doppler assistance. Both right and left lobes were sampledviaa “rapid-puncture” and one actuation for each lobe. The authors concluded that “EUS-MLB” was effective and safe in evaluation of inexplicable liver disease. The median TSL in their study was 6 cm, and the median number of CPTs per TSL was 18.
ADVANTAGES OF EUS-GUIDED BIOPSY
Historically percutaneous liver biopsy was done “blind”, however in present times this has largely been replaced by image guided biopsy. Image guidance is postulated to help increase sampling adequacy and more importantly reduce complications[4].There is some controversy regarding this and conflicting data have been reported[4,34].In 1991, Vautieret al[34]reported that ultrasound guidance dose not reduce bleeding complications from PC-LB and concluded that image guided liver biopsy may not be safer than blind biopsy. A retrospective analysis looked at the complications and safety profile of liver biopsy in patients enrolled in the HALT-C trial[35]. All the patients included in this trial had advanced chronic liver disease. A total of 2740 liver biopsies were performed and 90% were ultrasound guided. 16 of the total 29 cases of significant adverse events were from bleeding complications. EUS guidance aims to mitigate these complications further by better anatomical definition and doppler assistance.
Linear echoendoscopes were first introduced in the 1990s[36]. Linear echoendoscopes allowed the use of doppler ultrasound and the ability to track needles in real-time.Combined with high resolution imaging, the intrahepatic vessels and major bile ducts can be easily identified and avoided during biopsy, hence reducing potential complications[37].
Commonly a sixteen-gauge needle is used for percutaneous liver biopsy. On the contrary using nineteen-gauge needles for EUS-LB reduces possible complications. A large trial comprising over a hundred patients studied the diagnostic yield and safety of EUS-FNA using a 19-gauge needle[29]. Reported diagnostic yield was 98% as measured by the tissue sample length and presence of complete portal tracts. Serious adverse event was reported in one patient who developed a sub-capsular hematoma that required only conservative management. The authors concluded that EUS-LB was a safe technique with comparable diagnostic accuracy to PC-LB. Adleret al[38]performed a multicenter retrospective review of 200 patients, specifically looking at safety and performance when sampling solid lesions. They reported excellent diagnostic yield at 98.5%, however 6.5% of the patients needed a repeat procedure at some point. No adverse event was identified in the population. Table 1 summarizes the diagnostic accuracy and adverse event rates of EUS-LB.
EUS guidance has the benefit to sample and evaluate both lobes of the liver, hence achieving more accurate representation of liver histology, potentially addressing concerns about sampling error[24]. PC-LB and transjugular biopsies are both subject to sampling variability due to heterogeneity of parenchymal diseases[39]. This variability can be reduced by sampling both the liver lobes. EUS-LB allows easier access to the right and left lobe of liver; thus minimizing this variability[39].
For Pancreatic lesions EUS guided biopsy has proven superiority as an imaging modality for as it allows greater anatomical definition and higher resolution with the ability to sample ascites, local lymphatic structures and small liver nodules[40]. There is some evidence suggesting that for smaller liver lesions EUS-LB is indeed also superior and safer than PC-LB with CT or ultrasound guidance[41,42].
Other advantages of EUS-LB include a much shorter recovery time (about 4 h) than that of PC-LB (commonly at least 10 h)[13,43,44]. Another potential benefit is that patients are sedated for the EUS procedure, thus EUS-LB is better tolerated in most instances as compared with PC-LB[44,45]. However, it is important to remember that the benefits of sedation and anesthesia must be balanced against risk of respiratory depression. As described for trans-jugular biopsy, EUS-LB also has the potential advantage in patients with morbid obesity, large ascites, peliosis hepatis, and coagulopathy[14,15].
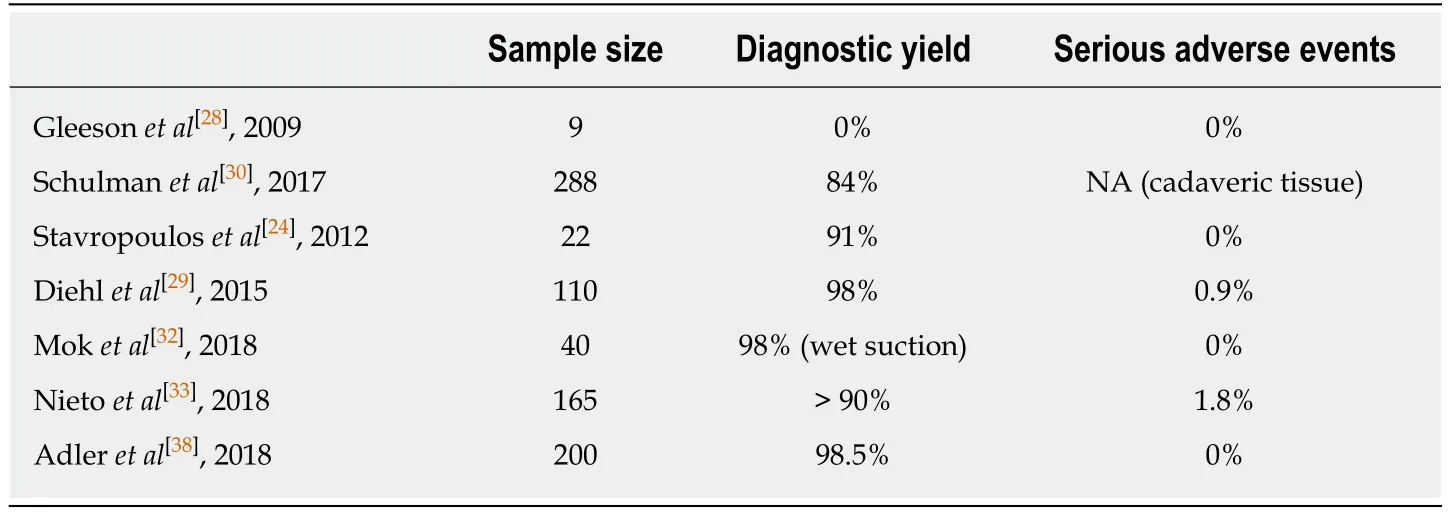
Table 1 Current evidence of diagnostic accuracy and adverse event rates of endoscopic ultrasound guided liver biopsy
DISADVANTAGES
Despite its advantages over the other liver biopsy techniques, the application of EUSLB in everyday practice has yet to reach its full potential. One of the barriers to this is the relative novelty of the technique. PC-LB and trans-jugular approaches have been used in clinical practice much longer than EUS-LB and hence operators have more experience with these. The conventional techniques are also easier and require less technical expertise. This is especially true with the use of Tru-Cut needle for biopsy which is more technically demanding and may have variable sample yield[46]. Tru-Cut needles have been largely replaced with more flexible needles that can be navigated with more ease[27,47].
Left lobe of the liver can be approached through the gastric wall, whilst the right lobe is accessedviathe duodenum. Right Hepatic Lobe sampling can be difficult in some cases due to difficulty in navigating the biopsy needle at sharp angles across the duodenum[15,48]. This again is more of an issue with Tru-Cut needles which have limited flexibility[47].
Another important consideration is the cost of procedure. EUS-LB has a much higher cost when compared to PC-LB and this can be prohibitive to the widespread use[15,39]. However, this drawback is offset in patients who are undergoing an endoscopy for another indication (such as esophageal varices screening). EUS-LB may be done during the same session with little additional time and risk. Patients intolerant or non-compliant of pre-procedure preparation can also prove to be a challenge to successful EUS-LB. Table 2 summarizes the comparison between PC-LB and EUS-LB.
CONCLUSION
Liver biopsy remains essential in diagnosis, evaluation and management of numerous liver diseases. Whilst percutaneous biopsy remains the test of choice, it has its drawbacks; and hence EUS guided liver biopsy has emerged over the resent past as a safe and effective alternative. Advantages of EUS-LB include easier access to both lobes of liver and improved diagnostic accuracy in heterogeneous parenchymal diseases as well as detecting multiple focal lesions. Procedure and recovery times are shorter with less reliance on patient cooperation. Additionally, the use of doppler assistance helps avoid blood vessels reducing risk of hemorrhage; which is the most common complication of liver biopsy.
Techniques of obtaining liver samples with EUS guidance and the equipment used,such as types of needles; is constantly changing. However, current evidence on EUSLB techniques is conflicting and there is no consensus on the best technique and type of needle used. Nevertheless, most centers have published positive results from their individual experiences. Despite these advances cost barriers and sparsity of technical expertise continue to remain limiting factors for the wide spread use of EUS-LB.
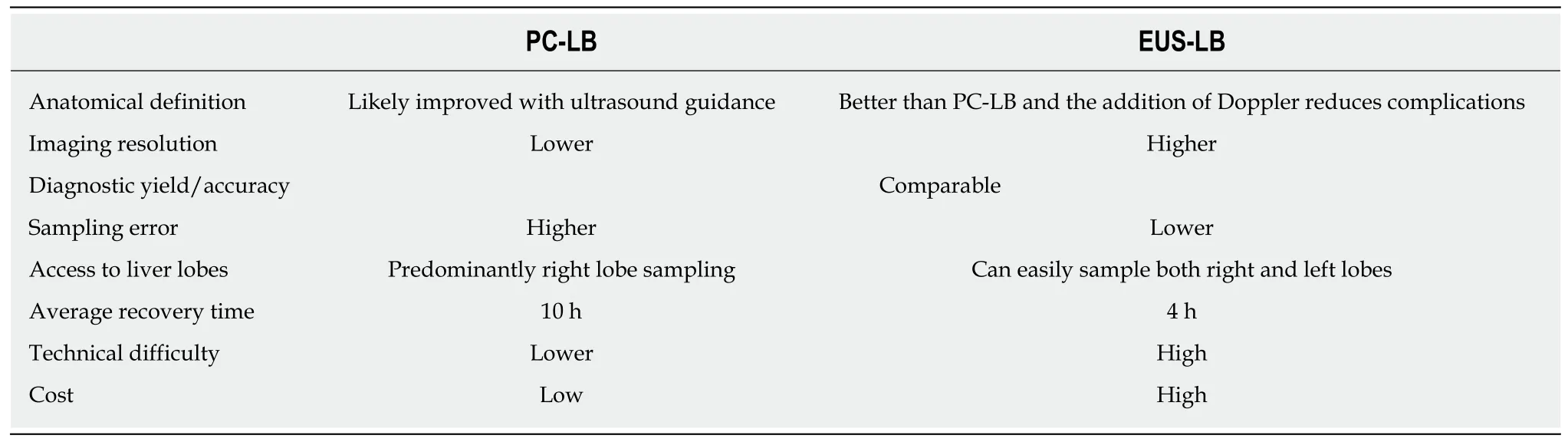
Table 2 Comparison of percutaneous liver biopsy with endoscopic ultrasound guided liver biopsy
 World Journal of Hepatology2019年4期
World Journal of Hepatology2019年4期
- World Journal of Hepatology的其它文章
- MicroRNAs contribute to ATP-binding cassette transporter- and autophagy-mediated chemoresistance in hepatocellular carcinoma
- Beneficial effects of losartan or telmisartan on the local hepatic renin-angiotensin system to counter obesity in an experimental model
- Being accompanied to liver discharge clinic: An easy measure to identify potential liver transplant candidates among those previously considered ineligible
- Effectiveness of venous thromboembolism prophylaxis in patients with liver disease
- Nonalcoholic fatty liver disease prevalence in an Italian cohort of patients with hidradenitis suppurativa: A multi-center retrospective analysis
- Leukocytoclastic vasculitis caused by hepatitis C virus in a liver transplant recipient: A case report
