Isolated colonic neurofibroma,a rare tumor:A case report and review of literature
Sara Ghoneim,Sonia Sandhu,Dalbir Sandhu
Sara Ghoneim, Department of Internal Medicine,Case Western Reserve University at MetroHealth Medical Center,Cleveland,OH 44109,United States
Sonia Sandhu,Department of Hematology and Oncology,Cleveland Clinic Akron General,Cleveland,OH 44307,United States
Dalbir Sandhu, Division of Gastroenterology,Case Western Reserve University at MetroHealth Medical Center,Cleveland,OH 44109,United States
Abstract
Key words:Neurofibroma;Colonoscopy;Neurofibromatosis type 1;Neurofibromatosis type 2;Spindle cell tumor;Endoscopic ultrasound;Case report
INTRODUCTION
Neurofibromas are peripheral nerve sheath tumors that consist of Schwan cells,perineural cells and myofibroblasts[1-3].They occur sporadically or as part of familial syndromes such as neurofibromatosis type 1(NF1)(von Recklinghausen's disease),NF2(central or bilateral neurofibromatosis),multiple endocrine neoplasia type IIb,or intestinal neurofibromatosis[2].NF1 and 2 are both autosomal dominant syndromes with variable clinical manifestations[1-3].The genes for NF1 and NF2 are found on chromosomes 17 and 22,respectively[3].Both genes encode tumor suppressor proteins.NF1 has no sex predilection and occurs with a prevalence of 1 in every 3000 individuals[3,4].About 50% of patients have a positive family history.In the remaining 50% of patients,the disorder represents a sporadic new mutation[3,4].The diagnosis of NF1 is largely based on clinical criteria established by the National Institutes of Health and involves the presence of two or more of the following features:Six or more café au lait patches,two or more neurofibromas,one plexiform neurofibroma,freckling in the axillary or groin region,Lisch nodules,optic glioma,a first degree relative with NF1 and/or the presence of osseous dysplasia[3].
Gastrointestinal involvement is seen in NF1 but not NF2[4].Abdominal neoplasms in NF1 can be divided into five categories:Neurogenic tumors,neuroendocrine tumors,gastrointestinal mesenchymal tumors,embryonal tumors and miscellaneous tumors.Neurogenic neoplasms seen in the abdomen include neurofibroma,plexiform neurofibroma,malignant sheath peripheral nerve sheath tumor,triton tumor and ganglioneuroma[3-4].Sporadic intestinal neurofibromas mainly arise in the small or large intestine and affect middle age adults[5].In the gastrointestinal tract,neurofibromas have been reported in the following order of decreasing frequency:the jejunum,stomach,ileum,duodenum and colon[3-7].Isolated colonic neurofibromas are rare with a few cases reported in literature(Table 1)[8-23].Here we present a case of an isolated colonic neurofibroma seen on a routine screening colonoscopy.
CASE PRESENTATION
Chief complaints
A 51-year-old Caucasian male was referred to our gastroenterology clinic for a routine screening colonoscopy.He had no complaints.
History of present illness
He was otherwise healthy and denied having bloody stools,fevers,chills or unintentional weight loss.
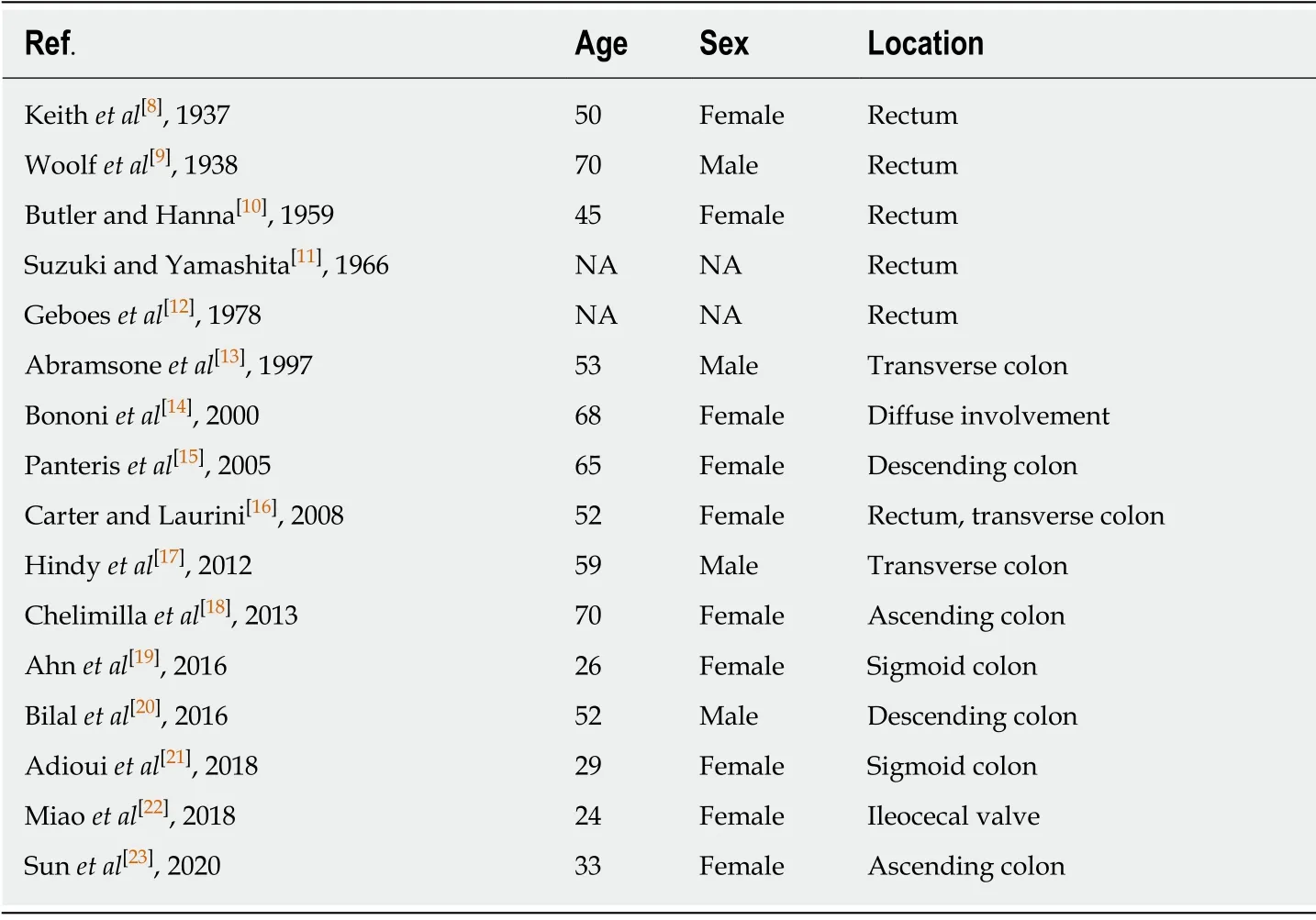
Table 1 Case reports of isolated colonic neurofibromas reported in English clinical literature
History of past illness
He had no significant past medical history or surgical history and was not taking any medications.
Personal and family history
Father had a history of hypertension.No family member had a history of cancer.
Physical examination upon admission
Temperature was 37 °C,heart rate was 75 beats per minute,respiratory rate was 18 breaths per minute,blood pressure was 129/72 mmHg and body mass index was 23.4 kg/m2.Physical examination was normal.His abdomen was soft with no tenderness or palpable masses.He had no skin lesions,pigmented or hypopigmented spots.
Laboratory examinations
Laboratory testing including complete blood count,basic metabolic panel,liver function tests and coagulation profile were all within normal limits.Hepatic serology was also negative.
Imaging examinations
He underwent a screening colonoscopy and was found to have a 3-cm submucosal pedunculated polyp about 15 cm from anal verge adjacent to the second rectal fold(Figure 1).Mucosal biopsies were obtained during the procedure.The specimen included fragments of colonic mucosa and a spindle cell tumor.As the mucosal specimens were unrevealing,the patient underwent magnetic resonance imaging of the pelvis which showed a 2.3 cm×1.4 cm lesion in the submucosa with no adenopathy.A subsequent endoscopic ultrasound revealed an ill-defined avascular lesion of mixed echogenicity measuring 2.8 cm×15.2 cm in the submucosa with no communication with muscularis mucosa or propria(Figure 2).Fine needle biopsy,with 19G SharkCore™ needle(Covidien),was obtained for pathology assessment(Figures 2 and 3).The tumor showed bland spindle cell proliferation in a uniform fascicular pattern with edematous stroma(Figure 3).The cells were elongated,with oval/wavy nuclei.No mitotic figures,necrosis,or tumoral hemorrhage were seen.The tumor showed strong and diffuse S100 staining,with rare penetrating axons deep within the tumor(Figure 4).Tumor cells were negative for c-kit,desmin and had low Ki-67 index.
FINAL DIAGNOSIS
These findings were consistent with a colonic submucosal neurofibroma.A detailed history and physical examination did not reveal any evidence of extraintestinal manifestations.

Figure 1 Findings at colonoscopy.A 3 cm submucosal pedunculated polyp is seen about 15 cm from anal verge.
TREATMENT
Our patient opted for transanal surgical resection.
OUTCOME AND FOLLOW-UP
The patient tolerated the procedure well without any complications.He will undergo a repeat colonoscopy in one year to evaluate for recurrence.
DISCUSSION
Our patient was diagnosed with a localized colonic neurofibroma without any clinical signs of NF1.The presence of such lesions in the intestinal tract without associated systemic manifestations is a rare finding.
Gastrointestinal involvement in NF1 has been reported in up to 25% of cases,with most lesions localizing to the upper gastrointestinal tract and rarely to the lower intestinal tract[24,25].The pathological forms seen in the gastrointestinal tract of patients with NF1 are characterized by hyperplasia and hypertrophy of the nerve plexus and ganglionic cells in the mucosa,submucosa,muscularis propria or even serosa[20,26].In addition to neurogenic tumors,patients may develop neuroendocrine and mesenchymal tumors such as gangliocytic paragangliomas,pheochromocytomas and gastrointestinal stromal tumors(GIST)[2-4].Intestinal neurofibromas predominately originate from the plexus of Meissner in the submucosa or the plexus of Auerbach[9].Dense growths known as plexiform neurofibromatosis may infiltrate the mesentery and lead to arterial compression or nerve injury[25].Endoscopically,neurofibromas are often sessile and wide-based or,as seen in this patient,pedunculated polyps[23].Clinically patients may present with abdominal pain,palpable masses,rectal bleeding,or obstruction due to intussusception or extra-luminal pressure,although most cases are found incidentally in asymptomatic patients.
Since there is no recommendation about modalities to explore these patients and because of the nonspecific clinical presentation of gastrointestinal lesion manifestations and limitations of endoscopic techniques,cross-sectional imaging may be used to aid in diagnosis.MR enterography is a non-invasive technique that has high sensitivity for detecting small bowel lesions and is more preferable than computed topography(CT)enterography for follow up of these patients because of concerns over exposure to ionizing radiation[24].CT colonography(virtual colonoscopy)is a potential alternative to conventional colonoscopy for the detection of colorectal tumors especially in poor risk patients[27].It is a non-invasive technique that requires no sedation and is well tolerated by most patients.CT colonography allows for complete visualization of the entire large bowel in almost all patients even following incomplete endoscopy and for colorectal examination proximal to an obstructing lesion.The use of multidector technology improves the detection of many colorectal lesions[27].Potential limitations of this modality include the inability to obtain tissue biopsy and exposure to ionizing radiation[27,28].
《剡录》又记:“金庭观,在剡金庭山,是为崇妙洞天,金庭福地。”“又东为洞山,山中人皆姓董,又曰董山。”“去观二里,曰再渡村(世传右军渡此,见山岭崇峻,以为罕有,故谓之‘罕岭’)。”“去观东一十五里,有大湖山。峰势入天,上有赤水、丹池(池可丈余,深不可测,其水色赤,勺之则其清如镜,祷雨甚灵)。旧为王右军宅,东庑设右军像,有书楼、墨池、鹅池。右军舍宅为观,初名金真馆,又改金真宫。”[7]2425
Tissue biopsy remains the gold standard for diagnosis[26].The differential diagnosis for neurofibroma of the abdomen includes schwannoma,myxoma,inflammatory fibroid polyp and GIST[2,25].Unlike myxomas,neurofibromas are diffusely positive for S-100[2].The absence of calretinin and a peripheral lymphoid cuff help distinguish these tumors from schwannomas and inflammatory fibroid polyps,respectively.In contrast to schwannomas,neurofibromas stain positively for CD34 and factor XIIIa[2].On the other hand,GIST stain positive for c-kit while neurofibromas do not[2].In our patient,histopathology revealed bland spindle cell proliferation in a fascicular pattern.Immunohistochemical staining was positive for S100,negative for c-kit and desmin.These features are consistent with a diagnosis of neurofibroma.
Malignant transformation of neurofibromas has been reported in patients with NF1[3,27].Malignant peripheral nerve sheath tumors are highly aggressive tumors associated with low survival rates(34%-52%)[29-31].The lifetime risk of these tumors in patients with NF1 is 8%-13%[3].Plexiform and larger neurofibromas are more likely to undergo malignant transformation[30-32].Malignant sheath peripheral nerve sheath tumors are often clinically silent when they arise in the abdomen and are often diagnosed at advanced stage.The prognosis remains poor and depends on the tumor size and location,resection margins,adjuvant chemotherapy,distant metastasis,stage and site[29-32].
The clinical significance of solitary neurofibromas is currently unknown,hence a thorough search should be made to exclude the possibility of colonic neurofibromas presenting as initial sign of NF1.Unfortunately,due to the rarity of this condition there is no consensus regarding management of these patients.Given the low incidence,and very few cases reported,long term follow up and screening goals are also unknown but close follow up is recommended to exclude neurofibromatosis and the associated risk of malignant transformation[29-32].

Figure 2 Findings with endoscopic ultrasound.A 2.8 cm×15.2 cm avascular lesion of mixed echogenicity seen in the submucosa with no communication with muscularis mucosa or propria.
CONCLUSION
An isolated colonic neurofibroma without associated signs of neurofibromatosis or systemic disease is a rare pathological finding.The clinical significance lies in the need to follow these patients as bowel involvement might be the first systemic manifestation of syndromic diseases such as NF1.
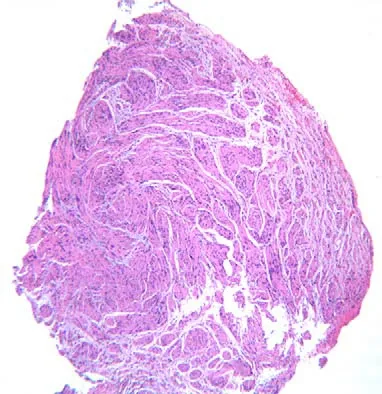
Figure 3 Histopathology of the tumor at low power×10 magnification.Bland spindle cell tumor is seen in a fascicular growth pattern.

Figure 4 Immunohistochemistry of the lesion at×50 magnification.Tumor is diffusely positive for S100.Note the penetrating axons with neurofilament stain.
ACKNOWLEDGEMENTS
We would like to thank Dr.Dan X Cai for providing the pathology slides.
 World Journal of Clinical Cases2020年10期
World Journal of Clinical Cases2020年10期
- World Journal of Clinical Cases的其它文章
- French Spine Surgery Society guidelines for management of spinal surgeries during COVID-19 pandemic
- Prophylactic and therapeutic roles of oleanolic acid and its derivatives in several diseases
- Macrophage regulation of graft-vs-host disease
- Antiphospholipid syndrome and its role in pediatric cerebrovascular diseases:A literature review
- Remotely monitored telerehabilitation for cardiac patients:A review of the current situation
- Keystone design perforator island flap in facial defect reconstruction
