Successful use of plasma exchange in fulminant lupus myocarditis coexisting with pneumonia:A case report
Zhou-Xiong Xing,Kun Yu,Hang Yang,Guo-Yue Liu,Ni Chen,Yong Wang,Miao Chen
Zhou-Xiong Xing,Kun Yu,Guo-Yue Liu,Ni Chen,Yong Wang,Miao Chen,Department of Critical Care Medicine,Affiliated Hospital of Zunyi Medical University,Zunyi 563000,Guizhou Province,China
Hang Yang,Department of Anesthesiology,Affiliated Hospital of Zunyi Medical University,Zunyi 563000,Guizhou Province,China
Abstract
Key words:Plasma exchange;Cardiogenic shock;Lupus myocarditis;Systemic lupus erythematosus;Immunosuppressive treatment;Case report
INTRODUCTION
Systemic lupus erythematosus(SLE)is the most prevalent autoimmune disorder with multisystem impairment and heterogeneous clinical presentations,and it typically affects females between puberty and the menopause[1].Although SLE is known to be associated with an increased risk of cardiac impairment which includes coronary atherosclerosis,valvular heart disease,myocarditis and pericarditis,fulminant lupus myocarditis is an uncommon but serious manifestation of SLE[2].Lupus myocarditis can be the first manifestation of the disease or occurs during follow-up[3].The clinical presentations of lupus myocarditis vary greatly from asymptomatic or oligosymptomatic to life-threatening fulminant myocarditis with cardiogenic shock,and the mortality rate is approximately 20%[4].Therefore,the diagnosis and treatment of severe lupus myocarditis remain challenging.
Aggressive immunosuppressive therapies,such as high-dose pulse corticosteroid therapy and immunosuppressive agents,are the most effective therapies for severe lupus myocarditis and most patients can achieve a satisfactory outcome[5].However,aggressive immunosuppressive therapies may significantly damage the host immunity and lead to a considerable risk of infection development and spread[6].Plasma exchange(PE),as an alternative therapy without immunosuppression,has been demonstrated to be safe and effective in treating severe lupus-related complications such as encephalitis,thrombotic thrombocytopenic purpura,antiphospholipid syndrome and nephritis,but it is rarely reported in cardiogenic shock induced by fulminant lupus myocarditis[7].Infection,especially pneumonia,remains a leading cause of morbidity and mortality among patients with SLE[8,9].Here,we report the case of a young woman requiring urgent ICU admission with a clinical diagnosis of cardiogenic shock induced by fulminant lupus myocarditis,with coexisting community-acquired pneumonia.Due to the presence of coexisting pneumonia,aggressive immunosuppressive therapies were not administered and PE was performed,which was shown to be safe and effective in improving impaired cardiac function without the risk of worsening the pneumonia.We also performed a review of the PubMed literature,and found no reports on the use of PE in severe lupus patients with associated infection.Thus,we believe that this is the first case of fulminant lupus myocarditis accompanied by pneumonia successfully treated with PE.
CASE PRESENTATION
Chief complaints
A 20-year-old Chinese woman,with anemia and thrombocytopenia,was admitted to the Hematology Department of our hospital due to progressive fatigue.
History of present illness
The patient presented with progressive fatigue three months ago,which had significantly worsened in the previous few days.Additionally,she had experienced intermittent knee pain with morning stiffness of both legs for almost six months.She had not seen a doctor until this hospital visit.She attended the emergency department of our hospital and initial laboratory tests showed anemia and severe thrombocytopenia.She was then admitted to the Hematology Department where further laboratory work-up was performed.On the second day of hospitalization,she was transferred to the ICU due to severe respiratory distress and shock.
History of past illness
The patient had no previous medical history.
Personal and family history
The patient did not have a history of smoking,drinking or drug abuse.
Physical examination
On physical examination,the patient was pale,awake,alert,responsive to questions and in acute respiratory distress.There was some skin petechiae,indicating a bleeding tendency,but there was no skin rash,oral ulcers,alopecia or enlarged lymph nodes.Her heart rate was 140 bpm,blood pressure was 112/70 mmHg with norepinephrine continuously pumped(0.8 μg/kg/min),respiratory rate was 42 breaths/min,and temperature was 37.6 °C.The oxygen saturation remained at 80%on room air and increased to 94% on a high-flow nasal cannula with FiO2of 40%.These findings suggested severe circulatory shock and respiratory failure.Heart auscultation showed low heart sounds without murmurs,and there were crackles over both lung fields,indicating heart failure associated with pulmonary edema or pneumonia.Her abdomen was soft and not tender,and the liver and spleen were not palpable.She had joint line tenderness in both knees and mild edema in both lower extremities.
Laboratory examinations
The initial laboratory tests are shown in Table 1.Blood tests revealed mild leukocytosis 10.71×109/L with moderate anemia(hemoglobin 71 g/L)and severe thrombocytopenia(platelet count 33×109/L).Alanine aminotransferase(98 IU/L)and aspartate aminotransferase(301 IU/L)were increased,which may have been attributed to liver congestion induced by heart failure.Creatinine(1.54 mg/dL)was slightly elevated,indicating mild acute renal damage.Activated partial thromboplastin time and prothrombin time were roughly normal.Cardiac damage markers,including myohemoglobin(864.3 ng/mL)and hypersensitive troponin T(142.9 ng/L),were increased.Her plasma N-terminal pro-B-type natriuretic peptide level(> 35000 pg/mL)was significantly high.Autoimmune profiles showed hypocomplementemia with C3of 36 mg/dL and C4of 13.7 mg/dL,positive antinuclear antibodies with a titer 1:1000(speckled nuclear pattern),positive SS-A antibodies(+++),positive SS-B antibodies(++)and positive Ro-52 antibodies(+++).An arterial blood gas on admission to ICU revealed a pH of 7.46,PaCO2of 21 mmHg,PaO2of 66 mmHg,lactate of 5.6 mmol/L,and HCO3-of 18 mmol/L with FiO2of 40%on a high-flow nasal cannula,indicating respiratory failure and circulatory shock.An admission electrocardiogram showed sinus tachycardia with low voltage.Respiratory and blood samples were sent for culture,without positive results.Other laboratory investigations revealed normal thyroid function and urine analysis.
Imaging examinations
Computed tomography of the chest showed an enlarged heart,increased pulmonary vascular diameter,ground-glass attenuation and interlobar fissure effusion,which suggested heart failure and pulmonary interstitial edema(Figure 1).Additionally,consolidation was found in both lower lobes in the lung,indicating pneumonia(Figure 1).Point-of-care ultrasound revealed an enlarged left ventricle(50 mm)(Figure 2A),global hypokinesia of the left ventricle and significant systolic impairment with a low left ventricular ejection fraction of 39.69%(Figure 2B),a distended inferior vena cava(22 mm)with loss of respiratory variation(Figure 2C)and diffuse B lines in both lung fields(Figure 2D).Based on these imaging findings,cardiogenic shock,pulmonary edema and pneumonia were confirmed.
Further diagnostic work-up
Viral myocarditis,one of the most common causes of cardiogenic shock in young people,was considered in the primary differential diagnosis.However,the patient had no previous medical history of upper respiratory tract infection and further virological serum tests,such as influenza A and B,enterovirus,adenovirus and cytomegalovirus,were negative.Therefore,viral myocarditis was excluded as the cause in this case.SS-A antibodies and SS-B antibodies were positive;thus,primary Sjogren's syndrome was considered.However,the patient did not have a dry mouth or dry eyes,and further Schirmer paper-strip tear tests were normal,with 12 mm/5 min and 13 mm/5 min for both eyes.Based on the 2016 American College of Rheumatology and European League Against Rheumatism classification criteria for primary Sjogren's syndrome[10],this was unlikely to be the cause in this case.

Table 1 Initial laboratory values
FINAL DIAGNOSIS
According to the 2012 Systemic Lupus International Collaborating Clinics(SLICC)classification criteria[11],lupus is a serologic diagnosis associated with a clinical diagnosis.The SLICC criteria require at least one clinical and at least one immunologic criterion for a total of four.The patient had thrombocytopenia,knee pain with morning stiffness,positive antinuclear antibodies,hypocomplementemia,severe heart failure and consolidation in the lungs with leukocytosis;thus,the final diagnosis in this case was cardiogenic shock induced by fulminant lupus myocarditis with coexisting community-acquired pneumonia.

Figure 1 Computed tomography scan of the chest.A:Image showing increased pulmonary vascular diameter(orange horizontal arrow),ground-glass attenuation(orange oblique arrow),interlobar fissure effusion(orange vertical arrow)and consolidation in the right lower lobe of the lung(white vertical arrow);B:Image showing an enlarged heart(horizontal arrow)and consolidation in both lower lobes of the lung(vertical arrow).
TREATMENT
Figure 3 shows the core treatment procedures and clinical course.Given the lifethreatening lupus myocarditis which can lead to cardiogenic shock and pulmonary edema,a vasopressor(norepinephrine)and diuretics were administered immediately.Due to the accompanying community-acquired pneumonia,high-dose corticosteroids and immunosuppressants were not used.To treat lupus myocarditis,intravenous immunoglobulin(IVIG)(0.4 g/kg/d)and methylprednisolone(80 mg/d)were administered for five consecutive days,resulting in complete recovery of platelet count,but cardiac function did not improve with the initial treatment.On the basis of methylprednisolone administered at a conventional dose,the patient was treated with PE of fresh frozen plasma(2000 mL/d)twice,and vasopressors were successfully discontinued within 48 h after initiating PE therapy.In addition,the patient received 10 days of intravenous broad-spectrum antibiotic therapy(moxifloxacin and meropenem),which resolved her pneumonia.
OUTCOME AND FOLLOW-UP
On the tenth day after admission to the ICU,repeated transthoracic echocardiogram showed a normal left ventricular size and function with a left ventricular ejection fraction of 63.3%(Figure 4).The patient remained asymptomatic,and on the twelfth day of admission,the patient was discharged from hospital followed by outpatient clinical follow-up on oral prednisone of 50 mg/d and hydroxychloroquine of 200 mg/d.The patient and her parents were satisfied with this treatment.At ten months after discharge,the patient was followed up in the outpatient department where a rheumatologist assessed the responsiveness to treatment,the activity of SLE,and adverse drug effects.Follow-up evaluations were approximately normal,including blood cell counts,hemoglobin,serum creatinine,urine analysis,bone density screening,ocular screening,electrocardiogram and echocardiography.The patient had no adverse drug reactions or infection caused by corticosteroids,and she gradually reduced and then stopped oral prednisone,and she remained healthy without recurrence of cardiac dysfunction,anemia,thrombocytopenia,fatigue and knee pain.Additionally,there were no manifestations of tumors or tuberculosis.Therefore,SLE was the final cause of cardiogenic shock.

Figure 2 Point-of-care ultrasound before undergoing therapy.A:Image showing an enlarged heart with a left ventricular end diastolic diameter of 50 mm(white line);B:Image showing a decreased left ventricular ejection fraction of 39.69%;C:Image showing a widened inferior vena cava with a diameter of 22 mm(orange vertical arrow);D:Image showing diffuse B lines in both lung fields(white horizontal arrow).
DISCUSSION
Cardiogenic shock is defined as a condition with low cardiac output caused by a cardiac disorder resulting in both clinical and biochemical manifestations of inadequate tissue perfusion[12].Fulminant lupus myocarditis is a rare cause of cardiogenic shock and common causes include myocardial infarction,viral myocarditis,Takotsubo cardiomyopathy,hypertrophic cardiomyopathy and idiopathic dilated cardiomyopathy[13].Myocardial infarction,with characteristics of ST-segment and T-wave on specific leads on the electrocardiogram,remains the most common cause of cardiogenic shock in the middle-aged and elderly population.Viral myocarditis can mimic lupus myocarditis with elevated serum markers of cardiac injury,low cardiac output and similar electrocardiogram manifestations.A definitive diagnosis relies on endomyocardial biopsy which is the gold standard for diagnosis.However,in medical practice,physicians diagnose viral myocarditis based on a combination of clinical features,laboratory analyses,and imaging findings[14].Similarly,the diagnosis of lupus myocarditis depends largely on clinical suspicion and echocardiographic findings rather than biopsy[3,15].In our case,clinical presentation,abnormal autoimmune profiles,significantly elevated troponin,global hypokinesia on echocardiogram,electrocardiogram with low voltage and normal viral assays led to the diagnosis of fulminant lupus myocarditis,rather than viral myocarditis causing the cardiogenic shock.
Fulminant lupus myocarditis is a rare but potentially fatal manifestation of SLE,which is a heterogeneous autoimmune disease and may involve almost all organs such as the skin,joints,the central nervous system,the kidneys,the heart and even the gut[16].SLE usually displays a variable clinical course with insidious onset,making early diagnosis challenging[17].Therefore,the patient in the current report was previously misdiagnosed with blood disease due to anemia and thrombocytopenia.Additionally,patients with fulminant lupus myocarditis may present with fatigue,fever,dyspnea and hypotension,mimicking pneumonia and septic shock that increases the difficulty of definitive diagnosis[18].

Figure 3 Clinical course and vasopressor doses.Moxifloxacin and meropenem were prescribed on days 1-10.Methylprednisolone was administered on days 1-12.IVIG was administered on days 1-5.PE was conducted twice on days 6 and 7,respectively.IVIG:Intravenous immunoglobulin;PE:Plasma exchange.
Currently,there are only classification criteria for SLE,but no gold diagnostic standard,thus hampering the definitive diagnosis.The 2012 SLICC criteria,with sensitivity of 97% and specificity of 84%[19],have facilitated the diagnosis.Nevertheless,classification criteria are often misused as diagnostic criteria,which may affect early diagnosis and lead to more misdiagnosed cases[20].Several conditions,especially disseminated tuberculosis and lymphoma,have clinical and laboratory features that can masquerade those present in SLE[21,22].Therefore,lupus,tuberculosis,lympho-proliferative disorders,as well as other autoimmune diseases,are often difficult to identify and are easily misdiagnosed.Clinicians should diagnose SLE on the basis of a complete medical history as well as on the adequate constellation of clinical or laboratory findings,after excluding other diseases[20].Patients with an initial diagnosis of lupus should be followed up for a period to exclude latent tuberculosis and lymphoma.In our case,the ten-month follow-up period showed no tuberculosis or lymphoma;thus,the final diagnosis was fulminant lupus myocarditis.
As myocarditis is not considered in the standard classification criteria for SLE and severe lupus myocarditis is an infrequent manifestation of SLE,current treatment strategies are based on isolated case reports rather than randomized clinical trials[18,23,24].Several case reports and series have demonstrated a favorable response to aggressive immunosuppressive therapies which mainly include high-dose pulse corticosteroids,methylprednisolone 0.5-1 g for 3-5 d[5,25,26],alone or with immunosuppressive agents,such as cyclophosphamide,azathioprine and mycophenolate mofetil[27,28].Reports have also shown some benefit from IVIG[29,30].Moreover,it is reported in one case that IVIG can be used in lupus myocarditis coexisting with infective endocarditis,for which immunosuppressive drugs were contraindicated[31].In some severe cases of cardiogenic shock,mechanical circulatory support,such as extracorporeal membrane oxygenation,is required[32].In recent years,biologic therapy,such as rituximab,has been demonstrated to be effective in refractory lupus myocarditis patients[33].
The use of immunosuppressive therapy in SLE carries significant risks of infection.The effect of these drugs on infection is also dose dependent,thus high-dose corticosteroids may create a more significant risk of infection[34].On the one hand,dysfunction of the innate immune system increases the risk of infection in patients with SLE;on the other hand,patients with SLE may have an increased risk of infection that is augmented by immunosuppressive therapies[9].Infection,especially pneumonia,is the main cause of mortality in patients with SLE[8].Considering the adverse effect of aggressive immunosuppressive therapies in worsening or spreading the confirmed or potential infection,this is a dilemma for clinicians when confronting severe lupus myocarditis which may coexist with infection or should be differentiated from infection.
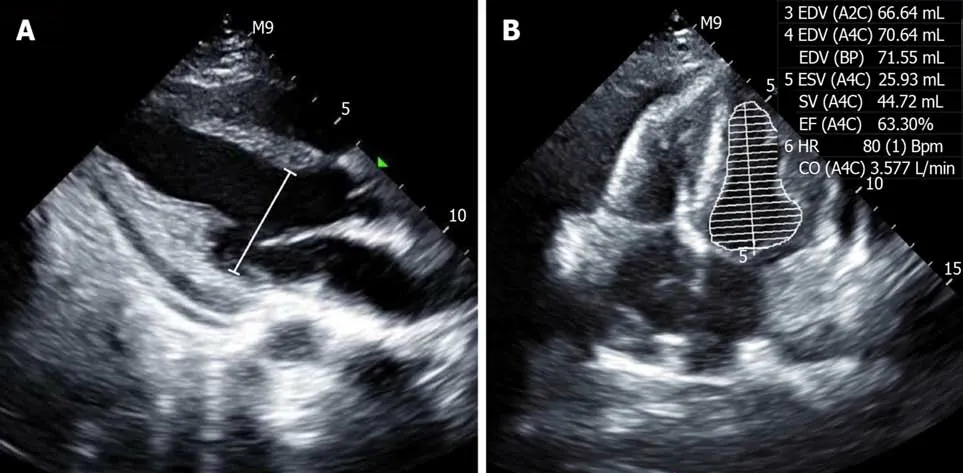
Figure 4 Point-of-care ultrasound after undergoing therapy.A:Image showing a normal left ventricular end diastolic diameter of 38 mm(white line);B:Image showing a normal left ventricular ejection fraction of 63.3%.
PE is a therapeutic procedure in which the patient's blood is passed through a device which separates the plasma from other components of blood.The plasma is removed and replaced with fresh frozen plasma[35].This can remove putative pathogenic autoantibodies and circulating immune complexes from the blood of patients with SLE[36].PE does not attenuate host immunity and adverse events of PE are uncommon.The indications for PE are acute life-threatening manifestations and severe therapy-resistant manifestations,such as diffuse alveolar hemorrhage,neurolupus,thrombotic thrombocytopenic purpura,catastrophic antiphospholipid syndrome and refractory SLE renal disease,and in pregnancy[36].Moreover,a small multicenter trial indicated that PE could be considered as a treatment option for refractory lupus nephritis in the setting of a high risk of infection[7].PE is considered effective and safe in treating these severe complications of SLE,but few cases of PE in lupus myocarditis have been reported to date[7,24,35,37].
Immunosuppression is the cornerstone of therapeutic interventions for SLE[38].Aggressive immunosuppressive therapies,especially high-dose pulse corticosteroids,are the most effective therapies for severe lupus myocarditis.However,our patient did not receive high-dose pulse corticosteroid therapy due to the adverse effect of immunosuppression which may have aggravated her community-acquired pneumonia.Corticosteroids at a conventional dose and IVIG were prescribed for five days as the initial treatment.As her impaired cardiac function did not improve with this initial therapy,high dose vasopressors were used.PE,a valuable option for treating severe SLE complications without immunosuppression,was performed with administration of corticosteroids at a conventional dose for two days and the patient discontinued vasopressors within 48 h.
Following treatment with corticosteroids,PE therapy was performed and reversed her impaired cardiac function.The limitation of our case report is that the improvement in impaired cardiac function could not be attributed exclusively to PE,as the patient had received IVIG therapy and corticosteroids before undergoing PE therapy.However,there is no doubt that PE can be used as a valuable therapeutic option when infection coexists in severe SLE patients.Our case has demonstrated that PE therapy can be used as an alternative treatment to aggressive immunosuppressive therapies in the background of infection.There are limited clinical data on the management of severe SLE accompanied by infection[7,31,39].We suggest that the indications for PE in SLE should include acute life-threatening SLE with the comorbidity of infection.
CONCLUSION
The early diagnosis and optimized treatment for severe lupus myocarditis remain challenging for clinicians.The diagnosis of lupus myocarditis should be considered in young people with acute onset of cardiogenic shock accompanying other organ involvement.Detailed medical history,careful examination and thorough laboratory work-up can aid early diagnosis.Moreover,this case indicates that PE is a good choice without immunosuppression for severe SLE patients with coexisting infection.
 World Journal of Clinical Cases2020年10期
World Journal of Clinical Cases2020年10期
- World Journal of Clinical Cases的其它文章
- French Spine Surgery Society guidelines for management of spinal surgeries during COVID-19 pandemic
- Prophylactic and therapeutic roles of oleanolic acid and its derivatives in several diseases
- Macrophage regulation of graft-vs-host disease
- Antiphospholipid syndrome and its role in pediatric cerebrovascular diseases:A literature review
- Remotely monitored telerehabilitation for cardiac patients:A review of the current situation
- Keystone design perforator island flap in facial defect reconstruction
