Efficacy observation of long-retaining scalp acupuncture plus interactive training for upper-extremity dysfunction after cerebral stroke
Qi Cong-hui (齐丛会), Cui Lin-hua (崔林华), Yuan Ye (袁野), Tian Yao (田瑶), Yang Jie (杨洁), Xing Xiao (邢潇), Zhang Sha (张沙), Chen Yuan-wu (陈元武)
1 Department of Acupuncture, Hebei General Hospital, Shijiazhuang 050051, China
2 Department of Rehabilitation, Hebei General Hospital, Shijiazhuang 050051, China
3 Department of Rehabilitation, Hebei Yiling Hospital, Shijiazhuang 050000, China
Abstract
Keywords: Acupuncture Therapy; Scalp Acupuncture; Scalp Stimulation Areas; Needle Retaining; Stroke; Poststroke Syndrome; Upper Extremity; Shoulder Pain
Cerebral stroke has become the leading cause of adult death and disability in China[1]. About 70%-80% of the sufferers present a certain level of disability[2], among which, limb dysfunction is the direct cause of impaired self-care ability in daily life. Upper-limb function is closely associated with the quality of life, since most of the basic living activities, such as eating, drinking, clothing, and going to toilet, all depend on the upper-limb function. Therefore, the recovery of upper-limb function should be emphasized after a cerebral stroke. However, in clinical practice, we found that some patients still counted on the conventional acupuncture-moxibustion treatment protocol and thus gained little progress in recovery. Given this phenomenon, this study adopted long-retaining scalp acupuncture plus interactive training to treat post-stroke upper-limb dysfunction, aiming to boost the healing process. The report is given as follows.
1 Clinical Materials
1.1 Diagnostic criteria
1.1.1 Diagnostic criteria in Western medicine
The Western medicine-based diagnostic criteria referred the Key Diagnostic Points for Cerebrovascular Diseases[3].
1.1.2 Diagnostic criteria in traditional Chinese medicine (TCM)
The TCM-based diagnostic criteria for cerebral stroke referred theStandard for Diagnosis and Therapeutic Effect Evaluation of Stroke (Trial)[4], with the assistance of head CT or MRI examination for confirmation.
1.2 Inclusion criteria
Conformed to the above diagnostic criteria; aged 20-80 years; first onset, with a duration of 1-5 months; presented unilateral upper-limb dysfunction; stable vital signs, in absence of progressive neurological signs within 48 h; willing to sign the informed consent form.
1.3 Exclusion criteria
Severe comorbidities, including liver or kidney dysfunction, myocardial infarction, heart failure, gastrointestinal bleeding, severe infection, mental disorders, dementia, Parkinson disease, and osteoarthropathy, etc.; acupuncture intolerant; epilepsy not under control; at high risk of bleeding or with blood coagulation dysfunction; visual, auditory or cognitive impairment, which may affect the evaluation; the affected limb was disabled before the onset of stroke.
1.4 Suspension and dropout criteria
Severe adverse events happened during the trial, and it was no longer suitable for the patient to go on receiving treatment; the condition got worse; failed to follow the requirement for observation and could not be taken into efficacy evaluation; those who quitted halfway; those evaluated as unsuitable to continue treatment concerning about possible damage to the patient.
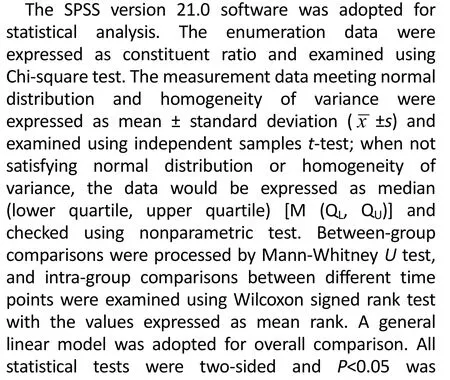
1.5 Statistical methods
1.6 General data
A total of 95 subjects diagnosed with upper-limb dysfunction after cerebral stroke were recruited from the Acupuncture-moxibustion and Rehabilitation Departments of Hebei General Hospital between December 2017 and September 2019. They were randomized into a treatment group and a control group by the random number table method, with 48 cases in the treatment group and 47 cases in the control group. There were no significant differences in the baseline including gender, age and disease duration between the two groups (allP>0.05), (Table 1).
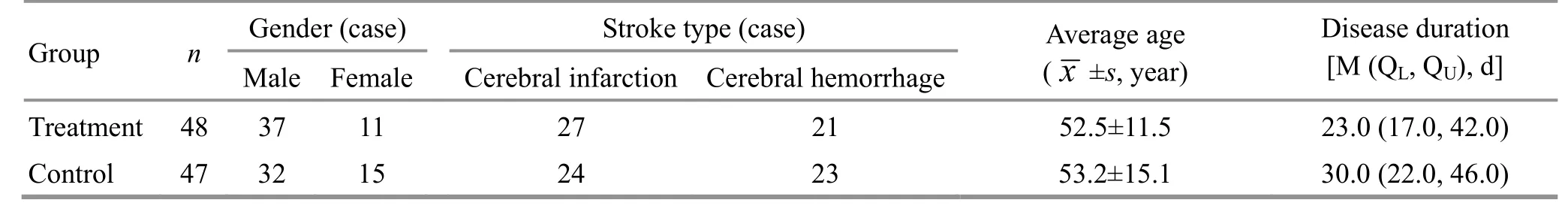
Table 1. Comparison of the general data between the two groups
2 Treatment Methods
Conventional internal medicine treatment was offered to both groups.
2.1 Treatment group
Scalp acupuncture stimulation areas: On the same side of the brain lesion, the middle 2/5 of the Anterior Oblique Line of Vertex-temporal [MS 6, located on the lateral side of the head, the middle 2/5 of the line between Qianding (GV 21) and Xuanli (GB 6)], and the middle 2/5 of the Posterior Oblique Line of Vertex- temporal [MS 7, located on the lateral side of the head, the middle 2/5 of the line between Baihui (GV 20) and Qubin (GB 7)].
Body acupoints: Jianyu (LI 15), Binao (LI 14), Quchi (LI 11), Shousanli (LI 10), Waiguan (TE 5), Hegu (LI 4) and Baxie (EX-UE 9) on the affected limb.
Methods:According to theStandardized Manipulations of Acupuncture and Moxibustion-Part 2:Scalp Acupuncture[5], the physician took disposable aseptic acupuncture needles, 0.30 mm in diameter and 40 mm in length, to puncture the scalp acupoints after standard sterilization of his own hands and the to-be-treated acupoints. The needle was firstly inserted beneath scalp by 15° and then turned parallel to the scalp and inserted more deeply when its tip reached the subgaleal layer where the physician could sense a notable reduction of resistance. The needles for scalp acupuncture were retained for 7 h. For acupoints on the trunk, acupuncture needles of different sizes were chosen according to the thickness of the topical muscles, either 0.25 mm in diameter and 25 mm in length or 0.35 mm in diameter and 75 mm in length. Needling sensation should be attained when these acupoints were treated and the needles were retained for 30 min. The trunk acupuncture was performed while the scalp acupuncture needles were still remained and one session of interactive training was finished. One more session of interactive training was performed before the removal of the scalp acupuncture needles.
Interactive training: The patient was asked to move the affected limb following the physician’s instruction while the physician was applying twisting manipulation to the scalp acupuncture needles at 200 times/min by 90-360°, which lasted for about 3 min. During this period of time, both the physician and the patient must focus their attention on the affected limb. The assistant could help the patient to perform those movements that he could not do alone. The physician should make clear of the target range and track of each movement according to the patient’s condition, and gradually increase the expectation and confidence of the patient. For example, the physician could determine the goal before each training session by measuring the height and angle of the shoulder, elbow and wrist joints when the affected limb lifted.
The above treatment was performed 5 consecutive days each week at 2-day intervals for a total of 4 weeks.
2.2 Control group
The control group received the same intervention as the treatment group except that the interactive training was skipped.
3 Observation of Therapeutic Efficacy
3.1 Observation items
3.1.1 Functional test for the hemiplegic upper extremity-Hong Kong (FTHUE-HK)[6]
The function of the affected limb was evaluated using the FTHUE-HK. It measured the function of the hemiplegic upper limb by 7 levels consisting of 14 items. The test should be finished within 3 min (each item can be tested 3 times). A higher level indicated better limb function. This test has a good reputation for its high validity and reliability in assessing upper-limb motor function and activities of daily living (ADL)[7]. 3.1.2 Fugl-Meyer assessment-upper extremity (FMA- UE)[8]
Simplified FMA-UE was adopted to assess the motor coordination and reflexes of the shoulder, elbow, wrist and hand. The full score was 66 points, and the higher the score, the better the limb function.
The two groups were evaluated once before treatment and at 2 and 4 weeks of treatment. The evaluation was conducted by a rehabilitation physician who had no access to grouping and treatment.
3.2 Criteria for therapeutic efficacy
The treatment efficacy was evaluated based on the relevant criteria in the Standard for Diagnosis and Therapeutic Effect Evaluation of Stroke (Trial)[4]in combination of the improvement rate of FMA-UE.
FMA-UE improvement rate = (Post-treatment FMA-UE score - Pre-treatment FMA-UE score) ÷ Post- treatment FMA-UE score × 100%.
Substantially recovered: FMA-UE improvement rate ≥81.0%.
Markedly improved: FMA-UE improvement rate ≥56.0% and <81.0%.
Improved: FMA-UE improvement rate ≥36.0% and <56.0%.
Slightly improved: FMA-UE improvement rate ≥11.0% and <36.0%.
Invalid: FMA-UE improvement rate <11.0% or even negative.
3.3 Results
There were no suspension or dropout cases in the trial.
3.3.1 Comparison of the total effective rate
The total effective rate was 97.9% in the treatment group, significantly higher than 74.5% in the control group (χ2=9.158,P=0.002), (Table 2).
Table 2. Comparison of the therapeutic efficacy (case)
3.3.2 Comparison of the FTHUE-HK score
There was no significant difference in the FTHUE-HK score between the two groups before treatment (P>0.05), indicating the comparability. Intra-group comparison: the FTHUE-HK score was higher at 2-week and 4-week treatment than before treatment in both groups, presenting statistically significant intra-group differences (allP<0.001); the FTHUE-HK score was higher at 4-week treatment than at 2-week treatment in both groups, presenting statistically significant intra-group differences (bothP<0.001). Between-group comparison: the FTHUE-HK score was higher in the treatment group than in the control group at 2-week and 4-week treatment, showing statistical significance (bothP<0.05). Overall comparison: the FTHUE-HK score increased gradually in both groups. Although the treatment group had a higher score throughout the whole treatment process, the between-group difference in the increasing trend was statistically insignificant at 2-week treatment (P>0.05), while a significant difference was found after 4 weeks of treatment (P<0.05). The results showed that both groups had improved upper-limb function, but the treatment group had better results. Speaking of the overall trend, the treatment group started to show advantage in efficacy since treatment week 2, and finally won out the control group at treatment week 4, showing statistical significance (Table 3 and Table 4).
3.3.3 Comparison of the FMA-UE score
There was no significant difference in the FMA-UE score between the two groups before treatment (P>0.05), indicating the comparability. Intra-group comparison: the FMA-UE score was higher at 2-week and 4-week treatment than before treatment in both groups, presenting statistically significant intra-group differences (allP<0.001); the FMA-UE score was higher at 4-week treatment than at 2-week treatment in both groups, presenting statistically significant intra-group differences (bothP<0.001). Between-group comparison: the FMA-UE score was higher in the treatment group than in the control group at 2-week and 4-week treatment, showing statistical significance (bothP<0.01). Overall comparison: the FMA-UE score rose up gradually with the increase of the treatment session in both groups. There were significant between-group differences in the increasing trend at 2-week and 4-week treatment (bothP<0.05). The results showed that both groups had improvement in the FMA-UE score, but the treatment group had better results. Speaking of the overall trend, the treatment group presented its advantage throughout the whole process with statistical significance (Table 3 and Table 4).
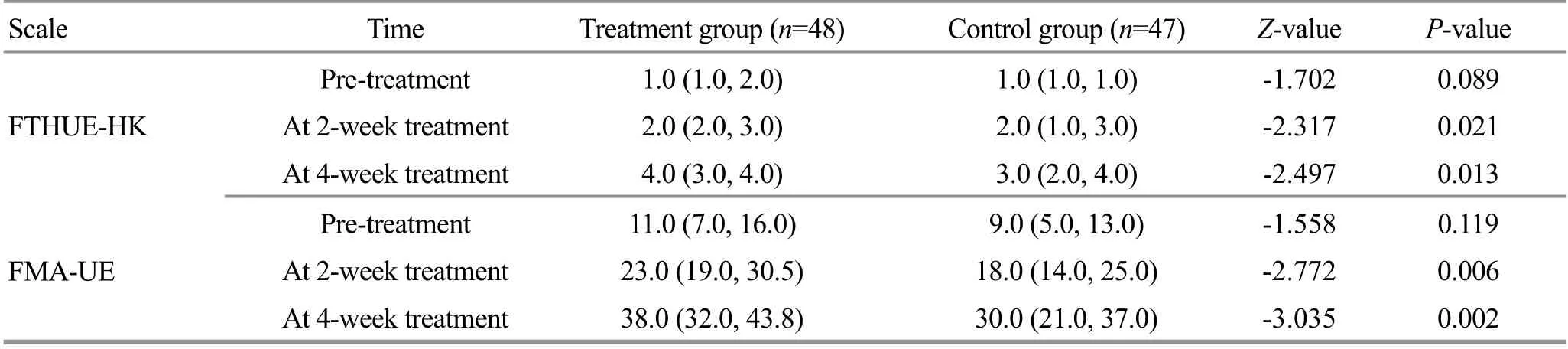
Table 3. Between-group comparison of the FTHUE-HK and FMA-UE scores [M (QL, QU), point]

Table 4. Intra-group comparison of the FTHUE-HK and FMA-UE scores
4 Discussion
Scalp acupuncture produces significant efficacy in treating cerebrovascular diseases. Research demonstrated that scalp acupuncture improved limb motor function, walking ability and ADL in cerebral stroke patients[9-11], while the conclusion on the needle-retaining time is still controversial[12-16]. Our previous study obtained valid efficacy by retaining the needles for 7-10 h during scalp acupuncture for improving post-stroke limb dysfunction and ADL, and this long-retaining scalp acupuncture achieved better result than retaining the needles for only 30 min[17]. On this basis, we conducted current study to further observe the effect of long-retaining scalp acupuncture combined with interactive training on upper-limb function in post-stroke patients (disease duration range 1-5 months).
The results showed that long-retaining scalp acupuncture plus interactive training was effective for post-stroke upper-limb dysfunction. The interactive training made both physician and patient focus their attention on the affected limb, which can help regulate mind and guide qi flow. This training method is based on the psycho-neuromuscular theory. Wang LL,et al[18]found that electroacupuncture plus movement ideas worked successfully for early-stage stroke (within 72 h after the onset); Xu LW,et al[19]achieved significant result by combining electroacupuncture and intensive motor imagery therapy in improving walking function in post-stroke hemiplegic patients, and its mechanism may be associated with the change in brain blood flow and the subsequent reorganization of brain function.
According to the current study, long-retaining scalp acupuncture plus interactive training produced more significant efficacy than using long-retaining scalp acupuncture alone for post-stroke (1-5 months after the onset of stroke) upper-limb dysfunction. Hopefully, this study can provide novel idea for the management of this medical condition.
Conflict of Interest
The authors declare that there is no potential conflict of interest in this article.
Acknowledgments
This work was supported by Project of Hebei Provincial Administration of Traditional Chinese Medicine (河北省中医药年理局项目, No. 2018083); Self-finance Project of Hebei Provincial Key Research and Development Program (河北省重点研发计划自筹项目, No. 172777194); Medical Technology Tracking Project in Hebei Province (河北省医学适用技术跟踪项目, No. G2018012).
Statement of Informed Consent
Informed consent was obtained from all individual participants.
Received: 20 January 2020/Accepted: 2 April 2020
 Journal of Acupuncture and Tuina Science2021年1期
Journal of Acupuncture and Tuina Science2021年1期
- Journal of Acupuncture and Tuina Science的其它文章
- Effect of electroacupuncture on calcium-activated chloride channel currents in interstitial cells of Cajal in rats with diabetic gastroparesis
- Effect of electroacupuncture pretreatment on the protein expression of c-fos in fastigial nucleus and lateral hypothalamus area in rats with acute myocardial ischemia-reperfusion injury
- Effect of herb-partitioned moxibustion in improving tight junctions of intestinal epithelium in Crohn disease mediated by TNF-α-NF-κB-MLCK pathway
- Ginger-partitioned moxibustion plus pediatric massage for treating infantile diarrhea due to spleen deficiency: a randomized controlled clinical trial
- Observation on therapeutic efficacy of thunder-fire moxibustion for hypomenorrhea after induced abortion
- Clinical observation on the time-effect relationship of moxibustion for primary dysmenorrhea due to stagnation and congelation of cold-damp
